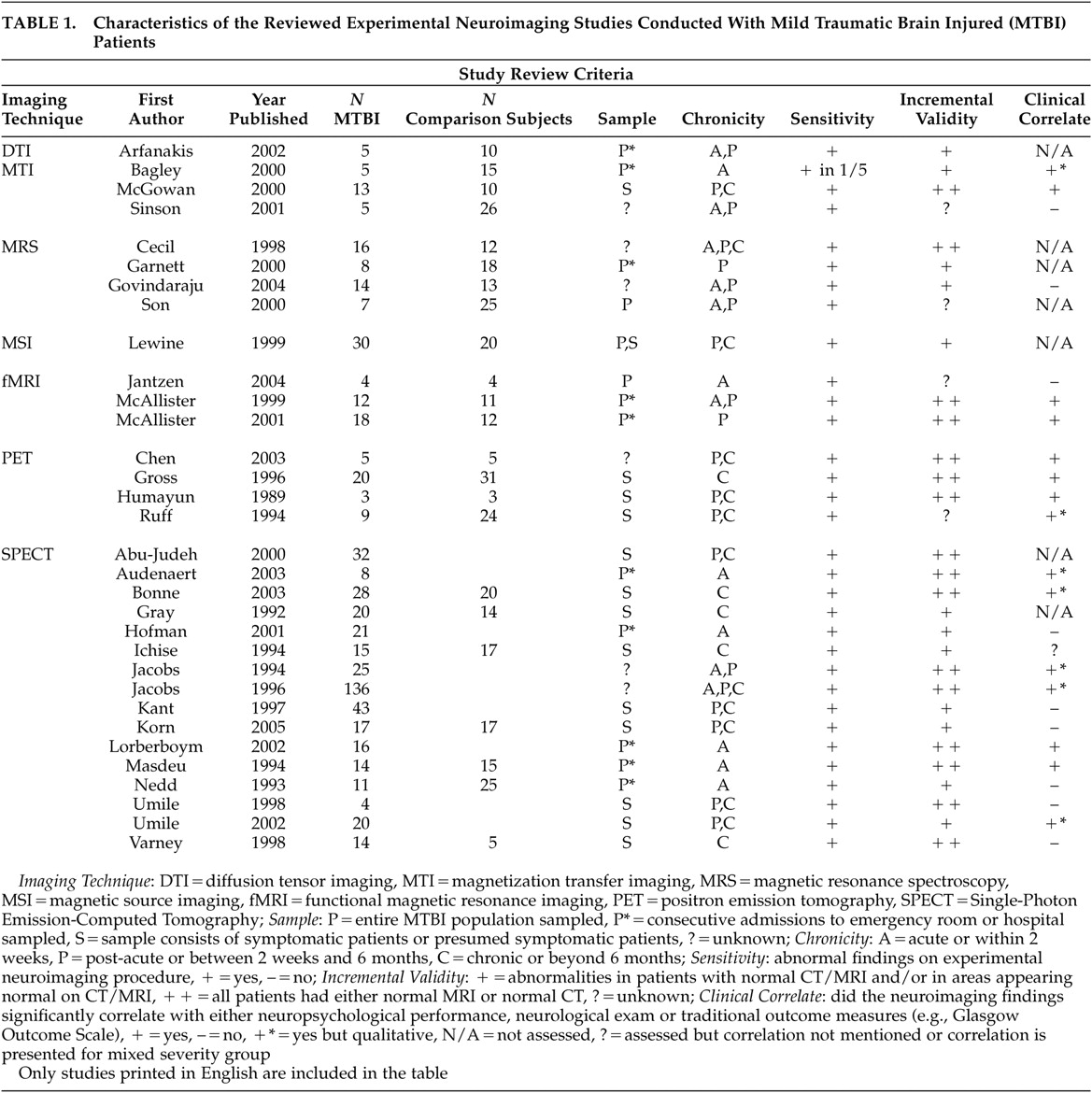
Functional MRI
Functional MRI (fMRI) is a widely used neuroimaging technique for measuring brain functioning. The assumption behind blood-oxygen-level-dependent (BOLD) fMRI, which is most commonly utilized, is that an increase in neuronal activity results in an increase in local blood flow, leading to reduced concentrations of deoxyhemoglobin, a product of oxygen consumption. This reduction of deoxyhemoglobin leads to a smaller local magnetic field gradient, which results in a greater T2 image and an increase in MRI signal. However, the relationship between the signal change in T2 weighted images and vascular flow differences are not fully understood and may be nonlinear. There is an initial hypo-oxygenation response to stimulation that is highly localized and then followed by several seconds of widely dispersed hyperoxygenation. Studies of working memory in moderate to severe TBI suggest blood flow abnormalities relative to comparison subjects, particularly in the frontal lobes.
72 –
74McAllister et al.
75,
76 studied working memory in mild TBI patients with normal structural scans who were approximately 1 month postinjury. In the first study,
75 12 mild TBI patients (GCS=13 to 15, LOC<30 minutes) were recruited from emergency room records and tested between 6 to 35 days postinjury. These patients had poor memory, trouble concentrating, and difficulty with their jobs, but did not express greater levels of anxiety or depression relative to comparison subjects. Mild TBI patients had poorer performance on neuropsychological measures of simple reaction time and sustained attention, but not on a variety of other measures, including psychomotor speed, executive functions, and memory. In the scanner, they were asked to complete an auditory “n-back” task that entailed successive levels of working memory tested through presentation of a series of letters.
During the 1-back condition, for example, participants were asked to discern whether a letter presented aurally represented a target letter presented visually a moment before. During the 2-back condition, they had to decide whether the letter heard matched the letter seen two letters prior. Both patients and comparison subjects activated bilateral frontal and parietal regions in response to increasing demands on working memory but produced different brain activation patterns in response to different processing loads. Whereas comparison subjects primarily showed increases in activation from 0-back to 1-back, mild TBI patients primarily showed increases in activation from 1-back to 2-back. However, the mild TBI patients and comparison subjects showed comparable overall levels of activation on the 2-back task and comparable performance on the
n -back task. The authors suggest that, rather than neuronal loss, mild TBI patients may have decreased ability to allocate or modulate resources according to processing load.
75In a follow-up study,
76 these researchers added a 3-back condition with 18 mild TBI patients, six of whom had participated in the prior study. All 18 mild TBI subjects had normal clinical (or structural) MRI scans. Mild TBI participants again showed more cognitive symptoms than comparison subjects and again had poorer performance than comparison subjects on attention measures. Their scores again were comparable to those of comparison subjects on all
n -back conditions and activated similar regions (bilateral frontal and parietal regions) in response to increasing demands on working memory.
Consistent with the prior study, the pattern of activation differed between mild TBI and comparison subjects. Mild TBI subjects had higher levels of activation than comparison subjects going from 1-back to 2-back, but less activation than comparison subjects going from 2-back to 3-back. Activation levels between 0-back to 1-back were not reported. This study again suggests subtle differences in brain functioning during increased working memory load. Rather than simply demonstrating additional activation with each increase in task difficulty, the observation was one of variable activation of mild TBI subjects compared to comparison subjects.
Finally, Jantzen et al.
77 conducted a prospective fMRI study of mild TBI using four concussed football players (no LOC but transient confusion) and four player comparison subjects. The scores of both groups on tests of sensorimotor coordination, working memory, memory, and mental calculations did not reliably change from preinjury to within 1 week postinjury. At baseline, the cognitive tasks elicited the expected brain activation patterns in frontal, parietal, and cerebellar regions. Within 1 week following injury to the concussed group, both groups showed increased activation during the cognitive tasks. However, the concussed players demonstrated much larger increases in supplementary motor, bilateral premotor cortex, superior and inferior parietal regions, and bilateral cerebellar regions.
These studies meet the sensitivity, incremental validity, and first step of the functional correlate criteria. However, the finding in McAllister et al.’s second study
76 revealed an anomalous pattern that is inconsistent with the first McAllister et al. study.
75 In the second McAllister et al. study,
76 comparision subjects actually showed significantly greater increases in activation than the mild TBI patients as the
n -back task became more demanding. Future research is needed to clarify these differences. Future studies also will need to address a number of methodological considerations, including the difficulty inherent in “controlling” for mood in TBI patients and the susceptibility of fMRI to artifact in regions commonly affected by TBI (i.e., the frontal lobes; see Hillary et al.
78 for a detailed discussion of these and other issues related to conducting fMRI research with TBI patients). In addition, it is unclear how long these anomalous patterns persist given that all studies to date have examined mild TBI participants within the first month postinjury. These issues aside, fMRI offers some of the most promising findings to date.
Positron Emission Tomography
Positron emission tomography (PET) is a diagnostic imaging technique for measuring regional brain metabolism. Glucose is brought to the brain via the bloodstream; accordingly, the rates of regional cerebral blood flow (rCBF) within various brain regions are regulated depending on the changing demands of these regions. Radionuclides used in PET scanning are typically isotopes with short half lives. These isotopes are incorporated into compounds normally used by the body, such as glucose or water, and then are injected into the body to trace where they become distributed.
Following severe TBI, brain cells exhibit a metabolic state called hyperglycolysis in which glucose metabolism is increased above normal levels. The initial brief response of hyperglycolysis is followed by a relatively prolonged period of metabolic depression that is followed by recovery. One study suggests that this recovery occurs at approximately 1 month regardless of severity.
79 This triphasic metabolic pattern has been demonstrated in animal models of TBI
80 and in research with humans using PET technology.
79,
81 –
84 Nonetheless, the studies summarized below suggest that metabolic abnormalities may persist chronically in at least some mild TBI patients.
Humayun et al.
85 studied three mild TBI patients (GCS=13 to 15, LOC<20 minutes, normal CT and MRI) who were 3 to 12 months postinjury and three matched comparison subjects. All three patients had deficits on neuropsychological testing in attention/concentration and memory abilities. None had a history of prior head injury. Mild TBI patients performed more poorly on a computer-based vigilance task during the scan, but not statistically so given the small number of participants. There were no significant group differences in global metabolic rate. However, decreased glucose metabolism was found in the left posterior lateral temporal cortex, right anterior frontal cortex, and left caudate nucleus of mild TBI patients, while increased metabolism was noted in left and right medial temporal cortices.
Ruff et al.
86 studied nine mild TBI patients (LOC<20 minutes) who were an average of 18 months postinjury (range=1 to 37 months), presented with significant neuropsychological deficits, and were consequently referred for PET scans. The authors reported that CT and/or MRI findings in these patients were “generally negative.” Both mild TBI patients and comparison subjects performed a continuous performance test during scanning. Unfortunately, results were not presented quantitatively. According to the authors, hypoactivity was more prevalent in frontal areas in the mild TBI participants.
Gross et al.
70 studied 20 patients with mild-to-moderate TBI who were being treated for TBI-related complaints (e.g., irritability and decreased attention) an average of 43 months postinjury. Based on loss of consciousness (<30 minutes), 17 of the 20 patients were mildly injured. All but two had normal MRI/CT scans. Both mild TBI patients and comparison subjects (N=31) performed a continuous performance test during scanning. Eighty-two ROIs were collapsed to temporal, frontal, and parietal regions. All 20 patients demonstrated some type of abnormality in at least one region. Although both hypo- and hyper-metabolism were found in the same regions across different mild TBI patients relative to comparison subjects, there was a significant correlation between the overall number of subjective complaints and number of PET metabolic abnormalities. There was also a significant relationship between attention/concentration complaints and temporal lobe abnormalities on PET within the mild TBI patients. Finally, there was an overall significant correlation between metabolism abnormalities in the three brain regions of mild TBI patients and performance on neuropsychological measures of memory and executive functions.
Chen et al.
87 examined differences between five mild TBI patients (GCS=13 to 15, LOC<30 minutes, normal CT/MRI) and five comparison subjects in rCBF, measured via H
2 15 O during a spatial working memory task. Mild TBI patients were an average of 16.6 months postinjury and presented with persisting complaints. They did not differ from comparison subjects, however, on a checklist measure of depression or anxiety and none of the patients was involved in litigation. Mild TBI patients performed more poorly on neuropsychological measures, particularly recognition memory and psychomotor speed, and expressed more postconcussive symptoms. Though there were no rCBF differences between patients and comparison subjects during the resting scan, there was a smaller percentage increase for mild TBI patients in the right inferior frontal gyrus during the spatial working memory task on which the groups performed comparably.
In summary, the results of PET studies conducted with mild TBI patients in the chronic stage are very inconsistent, with findings ranging from no global abnormalities but significant regional hypometabolism,
70,
85,
86 no overall abnormalities in metabolism except during a working memory task,
87 and both hypo- and hyper-metabolism in the same regions across different mild TBI patients.
70 As all of these studies were conducted at least 3 months postinjury, the inconsistency is troubling. In addition, although mild TBI patients typically perform comparably to comparison subjects on attention tasks, both hypometabolism and hypermetabolism are noted regionally in association with these tasks. The Chen et al.
87 study is an exception but utilized H
2 15 O methodology and showed frontal rCBF changes with the spatial working memory task in mild TBI subjects. PET abnormalities generally are associated with neuropsychological performance,
70 though these comparisons are sometimes made qualitatively.
86 PET studies offer promise, having demonstrated sensitivity to mild TBI, incremental validity, and functional correlates. Nonetheless, more studies conducted exclusively with patients with mild head injury are needed to understand the clinical correlates of hyper- versus hypometabolism.
Single Photon Emission Computed Tomography
Single photon emission computed tomography (SPECT) has been used as a less expensive and more readily available alternative to PET, with its primary application being the gross localization of rCBF. Unlike PET studies, however, SPECT studies typically measure the patient’s brain at rest. Measuring blood flow is considered an indirect gauge of brain metabolism. Also unlike PET, most applications of SPECT imaging require comparisons between an ROI and another brain region presumably free of injury. This methodological requirement is problematic for TBI work, given the potential diffuse nature of the injuries. It should further be noted that blood flow is not necessarily equivalent to metabolism. Although in healthy individuals the two are highly correlated, this relationship is less clear following TBI.
79 Indeed, some data suggest discordance between blood flow and metabolism following TBI.
88,
89 as has been demonstrated in the PET literature.
90 These caveats aside, SPECT offers promise with regard to meeting the criteria of sensitivity, incremental validity, and clinical correlates.
In patients within 2 days of injury, Audenaert et al.
91 found evidence of focal abnormalities in frontal and temporal regions using cobalt-57-SPECT in mild TBI patients (GCS=15, no loss of consciousness) with no evidence of pathology on CT or EEG. Clearly, incremental validity above and beyond CT is established, although no comparison subjects were studied. As such, there is no way to evaluate the extent to which these findings are specific to brain injury. These investigators found an association with neuropsychological testing in seven of eight patients, although this correlation was made qualitatively. In contrast, Hofman et al.
18 found no consistent relationship between neuropsychological tests and 99mTcHMPAO SPECT abnormalities in patients 2 to 5 days postinjury. In these mild TBI patients (GCS=14 to 15, LOC<20 minutes), SPECT again showed incremental validity over conventional MR images, identifying abnormalities in frontal, parietal, and thalamic regions. Most abnormalities represented hypoperfusion, although, again, there was no comparison with comparison subjects.
Finally, in 20 mildly to moderately injured patients who were 1 to 9 days postinjury, Nedd et al.
92 reported incremental sensitivity over CT scans in terms of both identifying more lesions (87.5% versus 37.5%) and greater surface area of involvement using 99mTcHMPAO SPECT. Most abnormalities reflected hypoperfusion compared with comparison subjects, although three cases exhibited hyperperfusion. This discrepancy could be due to the variability in certain patient characteristics of the group (i.e., differences between those measured at 1 versus 9 days postinjury). No attempt was made to correlate these SPECT findings with functional data.
More studies have examined patients in the postacute and chronic stages. As in the acute stages, SPECT demonstrates increased sensitivity beyond conventional CT/MRI. Umile et al.
93 found that four symptomatic mild TBI (GCS=13 to15, LOC<30 minutes) patients had decreased perfusion on SPECT (primarily frontal-temporal) an average of 19 months postinjury. However, these abnormalities were assessed subjectively, without benefit of a comparison group. All of the patients endorsed symptoms of depression and were impaired on neuropsychological tests of attention, memory, and information processing. Expected relationships between abnormalities within eight ROIs and neuropsychological tests were not demonstrated. Similarly, Varney and Bushnell,
94 in a sample of 14 mild TBI patients (GCS=13 to 15, LOC<30 minutes) with normal CT/MRI who were at least 5 years postinjury and chronically unemployed (despite a preinjury history of responsible employment), demonstrated 99mTcHMPAO SPECT hypoperfusion relative to comparison subjects primarily in anterior mesial temporal lobe. However, given that this sample is not representative of typical mild TBI (i.e., chronically disabled), it is difficult to draw conclusions. Finally, Bonne et al.,
95 in a symptomatic group of 28 mild TBI patients (GCS=13 to 15, LOC<20 minutes) an average of 5.2 years postinjury with normal CT/MRI scans, found 99mTcHMPAO SPECT abnormalities (hypoperfusion) relative to comparison subjects primarily in medial and lower temporal and frontal regions. These authors reported meaningful relationships between hypoperfusion in frontal, left posterior and subcortical regions and corresponding neuropsychological tests. However, these relationships were reported qualitatively in a dichotomous fashion with no indication of the strength of association.
Other studies conducted with patients in the chronic stages have tended to use a mixture of patients with both normal and abnormal CT/MRI scans. For instance, Gray et al.
96 utilized a sample of 20 mild TBI patients (GCS=13 to 15, LOC<20 minutes), 25% of whom had abnormal CT scans at least 6 months postinjury. Using 99mTcHMPAO SPECT, hypoperfusion (relative to comparison subjects) was found in 60% of patients, with an overall concordance between CT and SPECT of 55%. Ichise et al.
97 drew a sample of 15 mild TBI patients (GCS=13 to 15, LOC<20 minutes) from the same rehabilitation practice, for whom initial CT scans were available for about half of the sample (88% normal). These patients were again at least 6 months postinjury and were compared with normal comparison subjects. 99mTcHMPAO SPECT revealed relative hypoperfusion primarily in frontal and temporal regions. SPECT was more sensitive than CT/MR images. An anterior-posterior gradient was calculated by summing the activity in four anterior ROIs and dividing by the sum of four posterior ROIs. Whereas volumetric brain volume, as measured using structural T1-weighted MR images was not sensitive to mild TBI, the anterior-posterior SPECT gradient was sensitive to mild TBI and correlated with neuropsychological tests of attention, memory, and executive function in the whole group (both mildly and severely injured patients).
In a larger sample of 43 mild TBI patients (LOC<20 minutes) who were 1 to 65 months postinjury, Kant et al.
98 found 99mTcHMPAO SPECT hypoperfusion in 53% of their sample, with only 12% having documented abnormalities on CT/MR scans. Most SPECT abnormalities were in frontal and temporal regions. Neither memory and executive deficits nor self-reported depressive symptoms were significantly related to these abnormalities. As these analyses were conducted using dichotomous data (i.e., normal versus abnormal), less statistical power was available to detect potential differences. Umile et al.,
99 in a sample of 20 mild TBI patients (GCS=13 to15, LOC<30 minutes) who were referred for postconcussive symptoms from 2 weeks to nearly 8 years postinjury, reported inconsistent findings with regard to neuropsychological and PET/SPECT findings. Fourteen patients (70%) had the predicted memory problems coincident with temporal lobe abnormalities, while six patients (30%) had discordant findings (e.g., temporal lobe abnormalities but no memory deficits); these comparisons were made qualitatively.
Jacobs et al.
100,
101 examined the predictive power of SPECT by following 136 patients with GCS >13 and normal admission CT scans for 1 year postinjury. Clinical outcomes were measured categorically using a neurological exam, postconcussive symptom checklist, and memory and concentration tests. They found initial positive predictive power (i.e., conditional probability of subsequent poor clinical outcome given the presence of an initial abnormal SPECT scan) of SPECT to be 44% at 3 months with improvement to 83% at 12 months, while negative predictive power (i.e., conditional probability of a normal clinical outcome given initial normal SPECT) of the initial scan was 92% at 3 months with improvement to 100% at 12 months. Due to the high number of false positive errors at 3 and 6 months postinjury, these authors recommend caution in attributing an abnormal SPECT finding to posttraumatic sequelae in mild TBI; an abnormal initial SPECT scan postinjury does not preclude good clinical recovery.
However, a normal initial SPECT scan is highly suggestive of good clinical outcome. Indeed, the American Academy of Neurology guidelines recommend the use of SPECT as an investigational tool only, as the clinical significance of positive findings is unknown.
102 The Jacobs et al. study exemplifies one of the best attempts to address the relevant issues with regard to validity issues. It demonstrates the sensitivity of SPECT to mild TBI, its incremental validity by using subjects with normal CT scans, and its relationship with clinical variables. Moreover, this study followed patients prospectively to study predictive validity.
In summary, most SPECT studies, when conducted within the first few weeks postinjury, reveal hypoperfusion associated with mild TBI,
18,
91,
92 although relationships to clinical variables were either not demonstrated,
18 reported in a qualitative fashion,
91 or not studied. Studies conducted with more chronic mild TBI patients (i.e., 6 months or more postinjury) also reveal hypoperfusion on SPECT;
93 –
99 patients in all of these studies were symptomatic or presumably symptomatic (e.g., recruited from rehabilitation centers). These studies found inconsistent relationships between both symptom complaints and SPECT findings with neuropsychological testing. Some studies,
95,
97,
99 on the other hand, did find a relationship, although the location of metabolic abnormalities detected via SPECT and the site of cerebral dysfunction inferred from neuropsychological testing did not consistently correspond. In the only study to use the anterior-posterior gradient as the comparison with neuropsychological findings, a relationship was observed.
97Finally, very few of the reviewed SPECT studies used comparison groups, relying instead on clinical judgment. Nonetheless, there is a relatively consistent presence of hypoperfusion in the frontal and temporal regions across studies.