T raumatic brain injury is a leading cause of morbidity and mortality, accounting for approximately 2 million emergency room visits annually in the United States and over 500,000 hospital admissions. Another 5.8 million survivors of traumatic brain injury (TBI) in the United States have chronic disability due to their injuries. Because the age range of peak TBI incidence is 15 to 24 years, survivors may have relatively long life spans to cope with their impairments.
1 Therefore, community integration, with social and vocational rehabilitative strategies, is a primary treatment goal following acute medical stabilization and subacute rehabilitation. Psychiatric complications of TBI interfere with rehabilitative interventions and, more importantly, affect survivors’ abilities to function autonomously following their discharge from structured medical rehabilitative settings. Though the literature contains a wealth of case and retrospective studies, there is only a limited body of prospective studies using clearly defined criteria or structured instruments.
This report of the American Neuropsychiatric Association (ANPA) Committee on Research reviews the body of literature on post-TBI psychiatric disorders and identifies studies that provide information regarding various TBI-related neuropsychiatric syndromes. In the process, gaps in the literature are identified, yielding recommendations for future research. This report is intended to provide an evidence-based review of TBI-related noncognitive psychiatric disorders and considers the nosology, epidemiology, and risk factors and assessment of the quality of the evidence in the literature. We define TBI as any extracranial mechanical force to the brain that leads to any of the following:
1.
Any period of loss of consciousness
2.
Any loss of memory for events immediately before or after the event
3.
Any alteration in mental state at the time of the event
This definition is generally consistent with those used by the American Congress of Rehabilitation Medicine (ACRM) and the Centers for Disease Control (CDC).
2 Due to the complexity of the topic, references were limited to those that addressed nonpenetrating TBI. Due to the breadth of potential post-TBI syndromes and for the sake of practicality, we elected to confine this review to:
4.
Posttraumatic stress disorder
We excluded personality changes as a specific area of study because they represent a broad class of syndromes with an extremely diverse range of symptom presentations, which were determined to be beyond the scope of this study. Aggression, however, was included because of its high prevalence following TBI, clinical significance, and the Committee’s opinion that its diversity of presentation was manageable within the scope of this study. The Committee recognized that though post-TBI aggression may span several diagnostic entities, such as personality changes and psychotic and mood disorders, a discussion of post-TBI aggression represents an opportunity to clarify the relationship between neuropathology and psychopathology. The postconcussional syndrome was excluded because it represents a complex syndrome with associated pain and cognitive symptom domains that distinguish it from the syndromes in this study, which only involves behavioral symptoms.
The decision to exclude a focused review of post-TBI cognitive deficits in this review was made with the recognition that cognitive impairments, such as dysexecutive syndromes, amnesias, and perceptual disturbances, may contribute to, mimic, or alter the clinical presentation of psychiatric disturbances. The interactions between cognitive deficits and behavioral disturbances constitute a broad topic that exceeds the scope of this study. We have limited this discussion to the role of cognitive impairment as a risk factor for developing the secondary syndromes, or the impact of these syndromes on cognitive functioning.
The Committee’s rationale for reviewing neuropsychiatric sequelae of TBI was to assess the quality and extent of data on the relationship between TBI and psychiatric illness (i.e., what mechanisms and risk factors contribute to these syndromes, and how reliably the disorders may be identified). It is expected that clarification of the neural substrates of TBI-related psychiatric illness may, in turn, lead to a clearer understanding of the neural substrates of idiopathic psychiatric disease. The current DSM-IV-TR classification of mental disorders “secondary to” a general medical condition, such as TBI, denotes a causal relationship but lends little symptom-driven specificity to assist in the diagnosis of such syndromes. Notable exceptions are the diagnosis of “mood disorder due to a general medical condition with major depressive-like episode,” in which full criteria for major depressive disorder are met. However, in other cases the descriptive criteria lack the specificity demonstrated in other categories. As a result, their clinical utility is limited beyond assigning a descriptive label to patients.
METHOD
Relevant articles published between 1978 and 2006 were identified by searching MEDLINE using the following MeSH search terms for traumatic brain injury: brain injuries; brain concussion; craniocerebral trauma; head injury, closed. Each of these terms was cross-referenced with one of the following MeSH terms: psychosis; depression; mania; agitation; aggression; psychiatric status rating scales; anxiety. The results were limited to human studies and English language articles. We then manually excluded articles that met the following criteria: the topic of interest was not the central focus; review articles; letters to the editor. Articles were then reviewed based on the American Academy of Neurology’s (AAN’s) criteria for classification of articles on diagnostic methods:
3Class I
Evidence provided by a prospective study of a broad spectrum of persons with the suspected condition, using a “gold standard” for case definition where the test is applied in a blinded evaluation, and enabling the assessment of appropriate tests of diagnostic accuracy.
Class II
Evidence provided by a prospective study of a narrow spectrum of persons with the suspected condition, or a well-designed retrospective study of a broad spectrum of persons with an established condition (diagnosed by the “gold standard”) compared with a broad spectrum of comparison subjects, where the test is applied in a blinded evaluation, and enabling the assessment of appropriate tests of diagnostic accuracy.
Class III
Evidence provided by a retrospective study where either persons with the established condition or comparison subjects are of a narrow spectrum, and where the test is applied in a blinded fashion.
Class IV
Any design where the test is not applied in blinded evaluation or evidence is provided by expert opinion alone or in descriptive case series (without comparison subjects).
One limitation of this approach is that there are currently no “gold standards” for the diagnosis of psychiatric illness in neurological disorders. The best available approaches are validated and reliable instruments for the diagnosis of idiopathic psychiatric disorders. In situations where “gold standard” instruments and criteria were used, such studies were classified as Class I or II. This was determined to be the closest approximation to a reliable test available for the purposes of this study. Even using such constructs, however, we caution that these instruments have yet to be validated in populations with a high propensity for cognitive impairment. In fact, because of the effects of TBI on somatic, motivational, and cognitive functioning, the use of such instruments may result in over- or underdiagnosis of the syndromes.
RESULTS
We identified 66 studies meeting criteria for review. General findings included inconsistencies in TBI definitions, severity criteria, nosological methods, control for premorbid psychiatric disorders, duration of follow-up period, and tiered screening approaches.
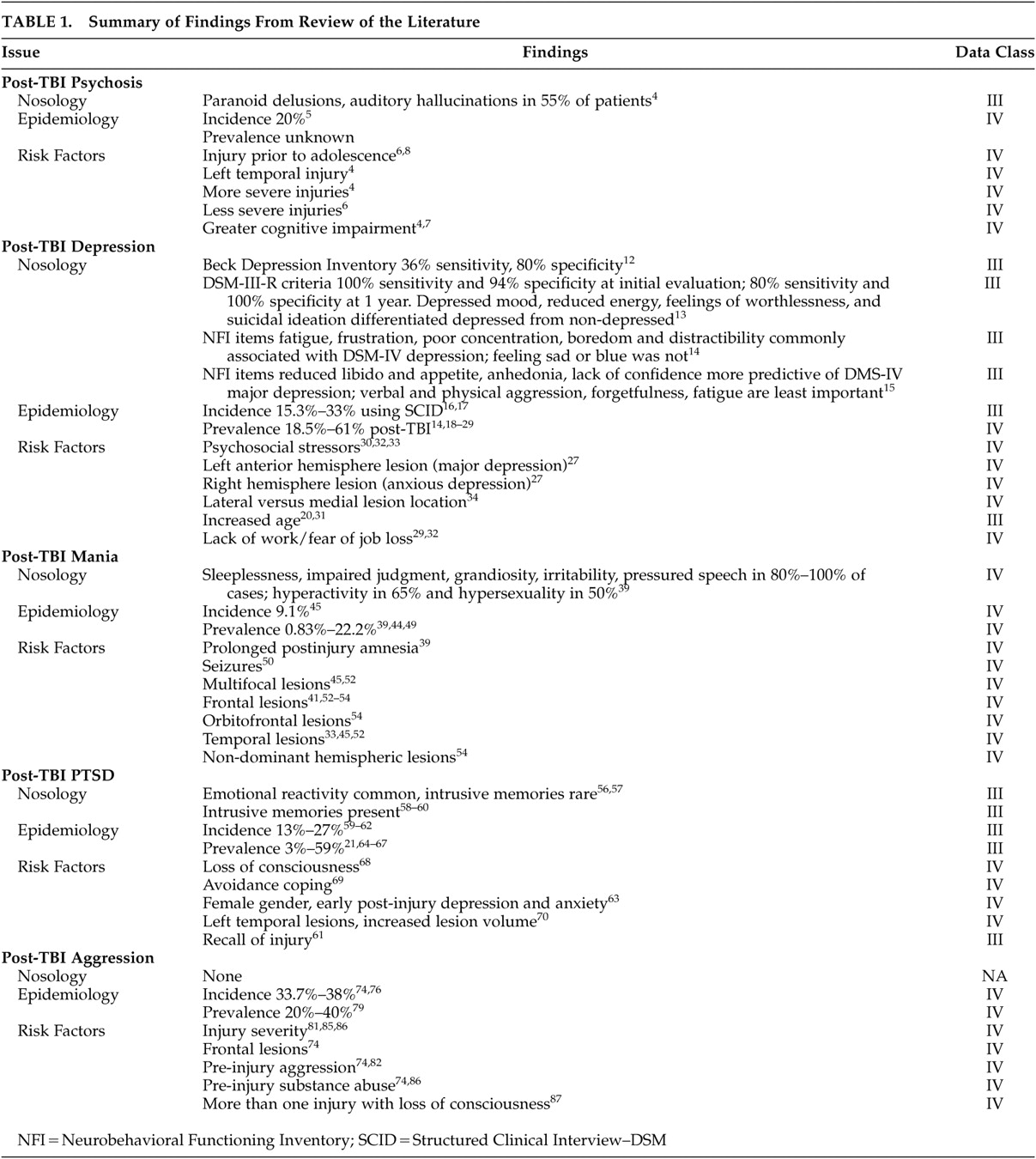
Table 1 summarizes our findings across all disorders reviewed.
Posttraumatic Psychosis
Nosology
Definitions of “psychosis” have varied widely in the literature. Sachdev et al.
4 matched participants on gender, age at injury, current age, and time since injury in a case-control study comparing 45 patients with “schizophrenia-like psychosis following TBI” (which included meeting DSM-IV criteria for schizophrenia or schizophreniform disorder) to 45 head-injured subjects without psychosis. In addition, all had received a computed tomography (CT) head scan and neuropsychological testing. The psychoses had a mean age of onset of 26.3 years, a mean latency of 54.7 months after head injury, and usually a gradual onset and a subacute or chronic course. Paranoid delusions and auditory hallucinations were present in 55% of patients, with formal thought disorder, catatonic features, and negative symptoms being uncommon.
Epidemiology
Incidence of Psychosis Following TBI
Thomsen
5 followed 40 survivors of severe TBI for 10 to 15 years after sustaining their injuries. In this sample, 20% developed psychotic disorders, though diagnostic criteria were not defined and hallucinations and delusions were not mentioned. This raises significant questions as to the validity of this figure.
Prevalence of Psychosis Following TBI
Strictly defined, no prevalence studies of psychosis following TBI were identified meeting search criteria.
Risk Factors
Fujii and Ahmed
6 conducted a retrospective chart review comparing 25 state hospital inpatients meeting DSM-IV criteria for a diagnosis of psychosis secondary to TBI to 21 outpatient TBI survivors without psychotic symptoms. TBI severity was based on American Congress of Rehabilitation Medicine criteria.
2 Regression analysis indicated the posttraumatic psychosis group was more likely to have had a previous congenital neurological disorder or to have sustained a head injury prior to adolescence. No differences were found between the groups with respect to handedness, highest education level attained, IQ, socioeconomic status, average age for sustaining the TBI associated with onset of psychosis, and type of TBI. More general prior substance use was present among those who developed posttraumatic psychosis, but no differences were found in the use of psychosis-inducing substances (e.g., LSD, amphetamine, and cocaine). There was also no difference found in proportion of seizure occurrence between psychosis and comparison subjects. However, because subjects were not matched for age or gender, and family history of psychosis was an exclusion criterion, it could not be determined whether these factors would have served as significant predictors of psychotic symptom development following a TBI. In this study, most subjects with posttraumatic psychosis had a mild head injury, whereas more severe injuries were reported in the comparison group. This study is limited by its retrospective nature and the comparison of severely psychotic state hospital patients with fewer impaired outpatients.
Sachdev et al.
4 found no significant differences between those with post-TBI psychosis and nonpsychotic TBI comparison subjects with respect to type of injury, prior alcohol and drug use, and posttraumatic behavioral and personality changes. Family history of schizophrenia, duration of loss of consciousness, language impairment, and frontal and parietal lobe deficits were more common in patients with posttraumatic psychosis. Preinjury neurological or developmental abnormalities were not significantly different between the two groups. The schizophrenia-like psychosis group had more widespread brain damage on neuroimaging, especially in the left temporal and right parietal regions, and was more impaired cognitively. On regression analysis, a positive family history of psychosis and duration of loss of consciousness were the best predictors of schizophrenia-like psychosis.
Fujii et al.
7 conducted a retrospective review of neuropsychological testing results comparing three samples: 24 state hospital inpatients with psychotic disorder following TBI (PDFTBI); 12 outpatients with a history of TBI without psychosis (TBIWP); and 24 state hospital inpatients with schizophrenia but no history of TBI. Tests included the Wechsler Adult Intelligence Scale (WAIS), verbal fluency, immediate recall of a narrative story, and the Wisconsin Card Sorting Test (WCST). The PDFTBI group demonstrated significantly lower scores than the TBIWP group in the WAIS IQ, semantic memory, verbal fluency, and WCST. The pattern of deficits was similar to that of the schizophrenia group, though the schizophrenia group demonstrated more severe and global impairments than the PDFTBI group. The study was limited by small sample size and the different function status of the study groups. The retrospective study design is also a limitation.
A different approach to clarifying risk factors for post-TBI psychosis involves retrospectively assessing prior head injuries in patients currently diagnosed with schizophrenia. Abdel Malik et al.
8 compared 67 patients with structured clinical interview-confirmed diagnoses of schizophrenia or schizoaffective disorder with 102 unaffected siblings in families with multiple occurrences of schizophrenia. Childhood head injuries (age of occurrence ≤10 years) occurred in 24% of schizophrenia patients versus 12% of unaffected siblings. Moreover, childhood head injuries were associated with a younger age of onset of schizophrenia. The median time between injury and first psychosis was 12 years. Malaspina et al.
9 utilized the Diagnostic Interview for Genetic Studies to determine the onset, nature, duration of loss of consciousness, severity, and number of traumatic brain injuries in 565 subjects with at least two first-degree relatives with schizophrenia. Schizophrenia patients had a threefold increase in their risk for a prior TBI compared with relatives without psychiatric illness. In contrast, Silver et al.
10 noted that among 5,034 participants interviewed as part of a National Institute of Mental Health (NIMH) Epidemiologic Catchment Area study in New Haven, prior head injuries were not significantly associated with a current diagnosis of schizophrenia. These results suggest that in individuals with a genetic vulnerability for schizophrenia, TBI may be a contributing factor to the expression of the disorder.
Summary and Recommendations
The literature on posttraumatic psychosis is limited by a lack of clear operational criteria to define it. The DSM diagnosis of psychosis due to TBI has been inconsistently used across studies and has limitations, prompting proposals for modifications to the criteria. No firm conclusions can be made regarding the incidence or prevalence of posttraumatic psychosis. A particular limitation of the literature has been difficulty in distinguishing patients with posttraumatic psychosis from patients with an “idiopathic” psychosis who have a prior history of head injury. The issue of a temporal versus causal relationship is not possible to resolve in the absence of a clearer understanding of the pathophysiological mechanism underlying posttraumatic psychosis, and a reliable means of distinguishing this process from that underlying idiopathic psychosis. The use of case-control versus prospective follow-up studies is problematic in that patients in primary mental health settings may have other etiological factors for their psychotic illness. Future research is necessary to accomplish several goals:
1.
To clarify the diagnostic criteria for psychosis due to traumatic brain injury. Specifically, this would require:
a.
Defining and validating core symptoms that distinguish “psychoticism” from cognitive or perceptual disturbances. In particular, so-called negative symptoms may prove nonspecific in their diagnostic validity in the presence of amotivational frontal symptoms.
b.
Defining a minimum and maximum time frame between injury and onset of psychosis. Though this would establish formal criteria for the temporal relationship between TBI and psychosis, it would not necessarily validate any causal relationship. Nevertheless, a consistent definition of the temporal relationship is a necessary prerequisite to research on causality.
c.
Defining exclusionary criteria that would differentiate TBI-related psychoses from idiopathic psychotic disorders.
2.
To clarify the incidence, prevalence, and natural time-course of posttraumatic psychosis in larger population samples of patients in primary TBI settings who are followed prospectively. This would require large-scale prospective multicenter descriptive studies. The TBI Model Systems (TBIMS) network, funded by the National Institute on Disability and Rehabilitation Research (NIDRR), consists of 16 sites that provide TBI services from acute care through community reentry. A network of this magnitude would likely be necessary to recruit sufficient numbers of patients to establish valid epidemiological and time course data. However, given the presumed low incidence and prevalence of posttraumatic psychosis, such a study would be justifiable only in the context of a larger study of all major psychiatric syndromes following TBI.
3.
To identify genetic, neuropsychological, and clinical correlates that are predictive of the development of post-TBI psychosis.
4.
To clarify the pathophysiological mechanism of posttraumatic psychosis compared with that of schizophrenia. Functional neuroimaging and post-mortem histological studies may help differentiate the two syndromes and contribute to more reliable diagnostic specificity. This is a prerequisite to distinguishing causal from temporal relationships between TBI and psychosis.
Post-TBI Depression
Nosology
Because symptoms of depressed mood and anxiety can represent appropriate situational reactions, transient normative variations, or pathological states, defining meaningful post-TBI depressive syndromes is a crucial first step. The DSM-IV diagnosis of mood disorder due to a general medical condition includes two subtypes that incorporate virtually the entire spectrum of post-TBI depressive phenomena. The subtype “with depressive features” refers to depressive symptoms that fail to meet full criteria for major depressive disorder, while the subtype “with major depressive features” includes those that meet full diagnostic criteria for major depression.
One challenge to using these criteria is that the effect of TBI on somatic and motivational symptoms may occur independently of effects on mood. For example, fatigue, sleep disturbance, concentration difficulties, and apathy are common signs and symptoms in TBI survivors with and without mood disorders. The addition of depressed mood to this constellation will result in meeting criteria for major depressive disorder. As a result, the prevalence of major depressive disorder in TBI survivors may be overestimated if unmodified DSM criteria are used.
11Given this all-inclusive range, a review of the entire literature in this area is unrealistic. Different authors, depending upon the purpose of their study and the decade of their work, used different approaches. Since the mid-1990s, there has been a consistent move toward using criteria listed in DSM-IV and DSM-IV-TR rather than rating scales alone which measure symptom severity irrespective of whether diagnostic criteria for the disorder are met. Sliwinski et al.
12 evaluated the relationship between the Beck Depression Inventory (BDI) and clinical depression using an SCID in 100 survivors with TBI. Twenty-five subjects were diagnosed as depressed. BDI symptoms correlated with depression but were more strongly related to other problems identified by The Institute for Rehabilitation and Research (TIRR) symptom checklist. The BDI had sensitivity of only 36% for discriminating depressed from nondepressed individuals, and a specificity of 80%.
Jorge et al.
13 examined the stability and change of psychological and somatic symptoms over the course of 1 year in 66 patients hospitalized for TBI, finding a 42% incidence of major depressive disorder. The standard DSM-III-R criteria for major depression had 100% sensitivity and 94% specificity at initial evaluation and 80% sensitivity and 100% specificity at 1 year. Four symptoms consistently differentiated depressed from nondepressed patients: depressed mood, reduced energy, feelings of worthlessness, and suicidal ideation. Though the authors suggest that DSM criteria are valid for the diagnosis of major depressive disorder in TBI survivors, the lack of discriminatory validity of all criteria suggests that some symptoms (e.g., sleep disturbance, diminished thinking ability, anhedonia) may be less useful in this sample.
Kreutzer et al.
14 evaluated 722 outpatients an average of 30 months post-TBI in an outpatient TBI clinic using the Neurobehavioral Functioning Inventory (NFI) to identify and quantitate symptoms consistent with diagnostic criteria for major depressive disorder. The authors categorized various items in the NFI to be consistent with DSM-IV diagnostic criteria. In this sample, 42% of patients met criteria for major depressive disorder. This study did not employ a gold-standard psychiatric diagnostic interview to confirm major depressive disorder diagnosis or validate the item clustering methodology used. The most commonly reported symptoms included fatigue, frustration, poor concentration, boredom, and distractibility. Feeling sad or blue (NFI item) was not endorsed frequently in this sample. This is at variance with the findings of Jorge et al.
13 that depressed mood was a differentiating symptom.
Kennedy et al.
15 evaluated 78 TBI patients in outpatient follow-up an average of 76 months postinjury using the SCID-I and the patient version of the NFI to evaluate the usefulness of the NFI in identifying depression. The SCID was used to identify patients meeting current DSM criteria for major depressive disorder. NFI items with the greatest importance in predicting a diagnosis of major depressive disorder included: loss of interest in sex, poor appetite, difficulty enjoying activities, lack of confidence, being uncomfortable around others, forgetting to do chores, feeling lonely, feeling sad or blue, and feeling frustrated. Items with the least importance included: threatening to hurt oneself, cursing at others, cursing at oneself, hitting others, sitting with nothing to do, screaming or yelling, restlessness, forgetting yesterday’s events, and tiring easily during physical activity. The authors cite the sample size as a limitation of the study’s generalizability and also call into question the validity of using DSM-IV criteria in diagnosing depression in TBI, given the overlap of neurovegetative symptoms in idiopathic depression and TBI without depression. Despite these limitations, this study represents a strong validation of the use of nonvegetative signs in assessing post-TBI depression.
Epidemiology
Given the variability in nosology described above, we adopted the most restrictive epidemiological approach, examining studies of major depressive disorder following TBI. Though this may underrepresent the actual incidence and prevalence of post-TBI depression, it was felt to be a more rigorous approach.
Incidence of Major Depressive Disorder After TBI
Rapoport et al.
16 assessed 170 consecutive survivors of mild TBI using the SCID at their first follow-up appointment in a TBI clinic an average of 48 days postinjury. Patients with preexisting major depression or bipolar disorder were excluded from this sample. In this sample, 15.3% of the patients met DSM-IV criteria for major depressive disorder. Subjects with major depressive disorder had higher rates of psychosocial dysfunction on the Rivermead Head Injury Follow-up Questionnaire, and psychosocial distress as measured on the General Health Questionnaire. In a subsequent study, Rapoport et al.
17 evaluated 74 patients with the SCID in the same setting an average of 200 days postinjury, finding a 28.4% incidence of major depression.
Jorge et al.
18 assessed 91 consecutive TBI patients admitted to a general hospital at 3, 6, 9, and 12 months postinjury. They were compared with 27 patients admitted for multiple trauma without TBI. In the TBI sample, 51.6% met DSM-IV criteria for mood disorder due to TBI, 33% with major depressive features, 9.9% with depressive features, and 8.8% with manic or mixed features. In the comparison group, major depression was identified in 7.4% of patients and 14.8% had depression without major depressive features.
Chamelian and Feinstein
19 evaluated 63 outpatients at a TBI clinic 6 months following a mild to moderate TBI using the SCID, Rivermead Post Concussion Symptoms Questionnaire, and a neuropsychological battery. They noted an 18.5% incidence of post-TBI depression in this sample. Levin et al.
20 evaluated 129 patients with mild TBI admitted to a trauma center at 1 week and 3 months postinjury using the SCID, noting an 11.6% incidence of major depression at 3 months.
Prevalence of Major Depressive Disorder After TBI
Hibbard et al.
21 evaluated 100 adults an average of 8 years post-TBI using the SCID to identify Axis I psychiatric disorders. This study yielded a prevalence rate of 61% for major depressive disorder following TBI. A separate analysis of major depressive disorder with onset following TBI led to a lower but still substantial rate of 48%. This second prevalence estimate may be a more reliable indicator of depression with a higher likelihood of being caused by TBI. One limitation of this study is that the sample was self-selected: participants responded to active recruitment through TBI newsletters and other means. This may have led to an “enriched” sample of TBI patients with an excess of psychiatric symptomatology.
Seel et al.
22 studied 666 outpatient survivors of TBI in a prospective multicenter study. Data regarding major depressive disorder were extracted from the NFI, which was administered as part of a comprehensive outpatient evaluation an average of 35.3 months following TBI. In this sample, 27% of patients met DSM-IV criteria for major depressive disorder. Symptoms with the highest discriminatory power between depressed and nondepressed patients included hopelessness and feelings of worthlessness. Koponen et al.
23 recruited 60 patients who had sustained TBIs between 1950 and 1971 and assessed them using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN). Major depression was identified in 26.7% of the sample. Onset of depression occurred either in the first year (32.5%) or more than 10 years postinjury (67.5%). The original population sample for this study was 210 patients. Of the original sample, 76 had died, and the rest either refused to participate or had nontraumatic neurological diseases that resulted in exclusion from the study.
Fann et al.
24 interviewed 50 consecutive survivors of TBI in a brain injury clinic an average of 32.4 months postinjury using the NIMH’s Diagnostic Interview Schedule (NIMH-DIS) and the Medical Outcomes Study Health Survey (MOSHS). In this sample, 26% met criteria for current major depression and another 28% met criteria for major depression that developed and resolved following injury. The mean time since injury was 32.5 months. Jorge et al.
25 and Fedoroff et al.
26 assessed 66 survivors of TBI during acute hospitalization and at 3-, 6-, and 12-month follow-ups for prevalence of primary mood disorder (DSM-III). Twenty-eight (42%) subjects had major depression at some time during the study period. Seventeen (26%) had acute-onset depression. Eleven (17%) had delayed-onset depression, which appeared to be influenced by psychosocial factors as well. Jorge et al.
27 also examined those 66 survivors of TBI for prevalence of major depression and generalized anxiety disorder. Ten (15%) acute-onset subjects met criteria for major depression without generalized anxiety disorder and seven (11%) subjects had both major depressive disorder and generalized anxiety disorder.
Holsinger et al.
28 investigated the lifetime rates of depression in World War II veterans who had a documented closed head injury using a modified version of the NIMH-DIS. Men with dementia or penetrating head injuries were excluded. Their sample included 520 veterans with head injury and 1,198 veterans without head injury. The lifetime prevalence of major depression in the group with head injury was 18.5%. In the comparison group, the lifetime prevalence was 13.4%. This diagnosis was not attributable to cardiovascular diseases or alcohol abuse. Lifetime risk of depression increased with severity of head injury. Bowen et al.
29 screened 99 survivors of TBI for emotional state about 6 months after injury. Using the Wimbledon Self-Report Scale, the rate of clinically significant mood disorder was 38%. Preinjury lack of occupation correlated with postinjury mood disorder. Psychosocial disability was more strongly associated with mood disorder than physical disability.
Risk Factors
Luis and Mittenberg
30 assessed 96 children consecutively admitted to a general hospital who were subsequently followed for 6 months postinjury. The sample consisted of 42 patients with mild TBI (GCS 13–15), 19 with severe TBI (GCS<13), and 35 children who had sustained skeletal fractures without head trauma or neurological abnormalities. Assessment was measured using the depression and anxiety modules of the Diagnostic Interview Schedule for Children-IV (DISC-IV). Sequential logistical regression was utilized to examine the impact of brain injury, demographic variables, preinjury psychiatric disturbance, developmental disorders, litigation status, and postinjury environmental stress on emotional outcomes. Postinjury level of stress and severity of brain injury accounted for 23% of the variance in the production of new onset depression and/or anxiety disorder. Glenn et al.
31 studied 41 outpatients in a rehabilitation hospital an average of 41 months post-TBI using the Beck Depression Inventory-II. Logistical regression demonstrated a positive relationship between depression and age, being female, having mild TBI, and use of antidepressant medications.
Gomez-Hernandez et al.
32 examined social factors contributing to the development of major depression after TBI. They studied 65 individuals from in-hospital care to 3-, 6-, 9-, and 12-month follow-ups. Fear of job loss was significantly associated with depression early in recovery. Fear of job loss and impaired close personal relationships were associated with depression at 6–12 month follow-up. The semistructured psychiatric interview, Hamilton Depression Rating Scale, and Social Functioning Exam were the objective measures used. Bay et al.
33 interviewed 75 TBI survivors and their significant others. All survivors were within 2 years of the date of injury and were living in the community. Using selective neuropsychological tests, the Perceived Stress Scale, the Interpersonal Relatedness Inventory, the Sense of Belonging Instrument, the Neurobehavioral Functioning Inventory, and the Center for Epidemiological Studies Depression Scale, the authors found a positive correlation between perceived levels of stress and depression. Sense of belonging was negatively related to new onset of depression.
Paradiso et al.
34 compared two small groups of TBI survivors with focal lesions identified by magnetic resonance imaging (MRI) who were matched for age, race, education, sex, socioeconomic status, and etiology of lesion. Eight survivors had medial lesions and eight survivors had lateral lesions. At 3 months after injury, survivors with lateral damage had worse depressive symptoms and apathy, with greater impairment of activities of daily living and social functioning. Satz et al.
35 examined 100 survivors of TBI using self-rated depression scales. Compared to 30 trauma survivors (nonbrain injuries), the severity of depressive symptoms correlated with the functional level of the Patient Competency Scale but did not correlate with neurocognitive performance measures. Jorge et al.
27 noted that patients with major depression alone tended to have left anterior hemisphere lesions, while depression with anxiety was associated with right hemisphere lesions.
Piccinelli et al.
36 elicited written responses from 158 survivors of TBI 60 months after injury. Thirty-eight percent reported “definite” anxiety and/or depressive disorders, although only 21% admitted to taking medications. Factors associated with development of depression or anxiety disorder were: sequelae of head injury (cognitive problems, seizures, facial pain), writing impairment, thorax problem, and new trauma. Initial injury severity and overall disability rating by the investigator were not strong predictors of anxiety or depression at follow-up. Bowen et al.’s study
29 found that preinjury lack of occupation correlated with postinjury mood disorder. Psychosocial disability was more strongly associated with mood disorder than physical disability.
Levin et al.
20 found that older age at occurrence of injury, CT abnormalities, and higher scores on the Center for Epidemiologic Studies Depression Scale at 1 week postinjury predicted the development of depression at 3 months.
Summary and Recommendations
There is substantial evidence that depression is a common complication of TBI, with a prevalence of 15.6% to 61% meeting criteria for major depressive disorder. This high variability suggests limitations in the diagnostic methods used, or perhaps variability in sampling methods (randomized versus self-selected based on referral/recruitment patterns). Because fatigue, poor concentration, and sleep disturbances are common post-TBI symptoms in the absence of depression, these criteria may inflate the frequency with which major depressive disorder is diagnosed in this population. However, the threshold for identifying “clinically significant” depressive syndromes is not clearly defined. Depression is a common cause for functional impairment in the general population, and there is substantial evidence of a similar effect in TBI. Rapoport et al.
16 and Fann et al.
24 found that TBI patients with depression had poorer functional and psychosocial outcomes. Risk factors for post-TBI depression appear to be related to stress, social isolation, and maladaptive coping styles, suggesting that reactions to injury-related deficits drive depressive symptomatology. Moreover, lateral lesion locations are associated with an increased risk of developing depression compared with medial lesions, with right lateral lesions increasing risk of anxious depression and left anterior lesions increasing risk for major depression. Future research is necessary to enhance knowledge in the following areas:
1.
Diagnostic criteria: Develop standardized categorical and dimensional criteria for post-TBI depression that have clinical and discriminative validity. In particular, DSM criteria of reduced energy, impaired concentration, and sleep disturbance may not reliably differentiate TBI-related depression from nonspecific neuropsychiatric sequelae of TBI. If this is the case, such symptoms should be eliminated from the diagnostic criteria in order to prevent the inappropriate use of antidepressant medications that may have little or no clinical value.
2.
Post-TBI course of depression: Given the large direct and indirect costs of depression identified in the general population and other medical populations, it seems logical to prioritize the detailed study of the incidence, prevalence, and post-TBI course of depression in the TBI Model Systems network using standardized, validated criteria and instruments.
3.
Long-term effects of post-TBI depression: Describe the long-term psychosocial, functional, and physical impact of post-TBI depression, particularly the impact of early recognition and treatment on longitudinal outcome. Once standardized criteria for diagnosis are developed, both prospective and retrospective studies using case control methodologies could facilitate this objective.
4.
Predictors of post-TBI depression: Identify biological, psychosocial, and cognitive predictors for developing post-TBI depression. Such variables could include family history of mood disorder, preinjury psychological trauma, or post-TBI executive cognitive impairment. The interactions between objective cognitive impairment and the processes by which TBI survivors adjust to altered vocational options as either knowledge workers or unskilled laborers create additional variability that has yet to be studied.
Posttraumatic Mania
Nosology
A variety of diagnostic criteria have been applied to posttraumatic mania including those of Dalén,
37 Feighner,
38 the Research Diagnostic Criteria (RDC),
39,
40 DSM-III,
39,
41 –
44 DSM-III-R,
44,
45 and DSM-IV.
46 Criteria for secondary mania
47,
48 have been inconsistently applied. Dalén
37 utilized clinical criteria and introduced exclusion criteria consisting of other organic insults and genetic diathesis. Assessment methodology has involved the use of clinical diagnostic criteria and semistructured diagnostic clinical interviews. Gureje et al.
40 utilized the Composite International Diagnostic Interview (CIDI) to determine RDC diagnoses. Shukla et al.
39 utilized the Schedule for Affective Disorders and Schizophrenia–Lifetime version (SADS-L) to ascertain RDC diagnoses, and both Shukla et al. and van Reekum et al.
44 used the SADS-L to determine DSM-III diagnoses. Jorge et al.
45 used the Present State Exam (PSE) to determine DSM-III-R diagnoses. Van Reekum et al.
44 used the Structured Interview for Diagnosing Personality–Revised (SIDP-R) for DSM-III-R Axis II disorders. DelBello et al.
46 used the SCID to ascertain DSM-IV bipolar disorder. Varney et al.
49 interviewed at least one first-degree relative to corroborate symptoms in subjects. Shukla et al.
39 examined specific symptom patterns in posttraumatic mania, including psychosis and assaultiveness. They also considered longitudinal illness course with respect to episodes of depression and hypomania. Jorge et al.
45 determined the duration of manic episodes as well as mood and assaultiveness.
There are no identifiable studies that have evaluated posttraumatic mania diagnostic validity or reliability. There have been several approaches to diagnosing posttraumatic mania. One straightforward approach ascertains posttraumatic mania when mania is present in the context of a previous history of TBI.
39,
41,
43 This approach, however, does not take into account the presence of mania prior to TBI, a genetic diathesis toward bipolar disorder, or other etiologies of mania. Thus, while in an ideal setting the diagnosis of posttraumatic mania would differentiate mania clearly
attributable to TBI from that simply
observed following TBI, in the absence of a validated pathophysiological model for the disorder, it is difficult to do so. As a result, the use of a temporal relationship in the absence of alternative explanatory etiologies may be the most useful approach.
Feighner et al.
38 have been credited with first extending nosological status to the concept of mania ascribable to a medical condition. Krauthammer and Klerman
47 introduced the concept of secondary mania attributable to specific primary medical etiologies; however, neither their report nor an update by Stasiek and Zetin
48 mentioned a posttraumatic etiology. Stipulating that mania must be attributable to TBI is a refinement in posttraumatic mania nosology, but specificity can be improved further. At some point, however, sensitivity will be sacrificed. To attain greater specificity, attempts have been made to exclude other potential etiologies of mania, such as family genetics. Dalén
37 examined the hypothesis that mania can be attributed to neurological disease. He used the clinical criteria of distinct elevation in mood, increased activity, tendency to act without proper judgment during discrete time periods, and an episodic course to define mania. Attribution of mania to trauma, perinatal insult, infectiousness, or family histories was assessed by review of medical records and interview of relatives, introducing to the nosological concept of posttraumatic mania the inclusion criterion of premorbid TBI and the exclusion of infectious etiology and positive family history of bipolar disorder. Other investigators, including Wilcox and Nasrallah,
50 Pope et al.,
42 and Hoff et al.,
43 have similarly required posttraumatic mania onset to be temporally subsequent to TBI, suggesting attribution to TBI.
The specific application of inclusion and exclusion criteria to posttraumatic mania was suggested by Riess et al.
51 in a review of the literature. They concluded that the diagnosis of posttraumatic mania should be considered in manic patients with an atypical age of onset, absence of previous psychiatric illness, negative family history for bipolar illness, and a close temporal relationship to TBI.
Epidemiology
Incidence of Posttraumatic Mania
Only one study in the literature used a systematic approach sufficient to yield information pertaining to incidence. Jorge et al.
45 followed up 66 consecutive patients with closed head injury at 3, 6, and 12 months. Inclusion criteria specified patients over age 18 with acute closed head injury free of multiple body injuries but with various levels of consciousness. Severity of brain injury was determined using the 24-hour Glasgow Coma Scale score, but patients with mild scores
12 –
15 who underwent intracranial surgical procedures or had focal lesions greater than 25cc were considered to have moderate head injuries. Forty-five of the 66 patients were classified as having moderate head injuries. Patients were evaluated using a modified version of the PSE semistructured psychiatric interview for DSM-III-R diagnoses, the Hamilton Depression Rating Scale, Mini-Mental State Examination, Johns Hopkins Functioning Inventory for activities of daily living, Social Functioning Exam, and Social Ties Checklist. CT scans were obtained on admission and 1 to 2 weeks later, and lesion location analysis was undertaken using logistic regression analysis. Patients with delirium or affective disorder at the time of the TBI were excluded. Though not specifically stated, it appears that patients with a history of bipolar disorder prior to TBI were also excluded. Six patients (9.1%) met criteria for mania over the 12-month follow-up period. Irritability, sometimes coupled with euphoria, was present in all and half were aggressive. None had seizures. The investigators point out that the sample was primarily of young white men from lower socioeconomic classes, with alcohol or drug abuse and multifocal brain injuries, and that 35% of patients were lost to 6- or 12-month follow-up, with dropouts significantly correlating with cortical and orbitofrontal lesions. The authors therefore suggest that the rate of 9.1% with posttraumatic mania may be a conservative figure because of the high dropout rate. If one considers the possibility that a majority of posttraumatic mania cases develop after a period of at least a 1-year delay, the figure may indeed constitute an underestimate.
Any future determination of posttraumatic mania incidence must be interpreted within the context of the duration of surveillance post-TBI, because several studies have reported a substantial delay between the TBI and the development of posttraumatic mania. For example, Dalén
37 observed two patients in whom posttraumatic mania developed 4 to 5 years post-TBI. Shukla et al.
39 found that posttraumatic mania followed a latency of 2.8 (SD=3.4) years. Consequently, studies of incidence should look at different incidence surveillance periods relative to the injury because incidence of new cases of posttraumatic mania may depend upon time elapsed since the lesion. On the other hand, the longer the period of delay, the more the attribution to the index TBI may be questioned.
Prevalence of Posttraumatic Mania
Strictly defined, only the study of Jorge et al.
45 was adequately designed to assess 12-month period prevalence of posttraumatic mania. In this study, described in the section on incidence, the authors followed up 66 consecutive patients with closed head injury at 3, 6, and 12 months and found a 12-month posttraumatic mania incidence of 9.1%, which might also be viewed as a 12-month period prevalence figure. Mania was brief, with a duration of about 2 months. Irritability, sometimes coupled with euphoria, was present in all and half were aggressive. None had seizures. Considerations regarding the validity of this 1-year figure were discussed under “Incidence of Posttraumatic Mania.”
Varney et al.
49 reviewed a sample of 120 patients with closed head TBI referred for neuropsychological testing at several hospitals, with a range of coma durations lasting a few minutes to 8 days. These subjects were compared with 60 comparison subjects with back injuries (without head injuries) referred for assessment with the Minnesota Multi-Phasic Personality Inventory (MMPI) and an interview at one of the hospitals. Subjects were interviewed at least 2 years after the injury (range=2 to 8 years, mean=3.4 years) with regard to DSM-III symptoms of mania and family history. At least one first-degree relative was interviewed to corroborate the family history and the subjects’ symptoms. A structured interview was not used and a family history of mania was not specifically inquired about. Four patients (3.3%) with closed head injury met DSM-III criteria for mania, but three had a family history of bipolar affective disorder and were already being treated with lithium. It is not clear how many of the patients were ill before the onset of the head injury, so it is possible, yet inconclusive, that one patient (0.83%) had secondary mania attributable to the head injury.
Van Reekum et al.
44 studied 18 subjects under age 40 from a regional TBI rehabilitation program at least 2 years postinjury. These subjects had no documented preinjury psychiatric illness or cognitive deficits. All subjects were interviewed by a psychiatric nurse using the SADS-L for DSM-III-R Personality and the SIDP-R. The subjects included 10 women and eight men with an average duration from TBI to assessment of 4.9 years. Three patients were diagnosed with bipolar affective disorder and two were diagnosed with cyclothymia, with one (5.6%) subject experiencing onset of the disorder prior to TBI. It was not clear whether this subject was diagnosed with posttraumatic mania or cyclothymia, and the follow-up period was not specified. Four subjects had severe TBI while one had moderate severity of TBI. The low participation rate and the highly selected and retrospective nature of the study may inflate the prevalence observed and call for caution in generalizing the findings. However, the authors point out that four of the five subjects with bipolar spectrum disorders were men and that the actual prevalence of bipolar disorder in head injured patients may be higher than observed in this sample, since men tend to predominate in the TBI population, in contrast to the demographics of the sample studied.
Shukla et al.
39 examined the course of posttraumatic mania in 20 TBI survivors referred from hospital clinics with posttraumatic mania diagnosed by RDC and DSM-III criteria and ascertained using the SADS-L. All subjects lacked mania in first- and second-degree relatives although six (30%) probands had one or more relatives with depression. They found that manic episodes predominated over depressive episodes, 10 to 1, and that hypomanic episodes predominated over depressive episodes, 5 to 1. The mean follow-up period of the study appears to be 11 years after TBI, but a specified prevalence surveillance period was not uniformly applied to each patient. Posttraumatic mania episodes were characterized by sleeplessness in 100%, impaired judgment in 100%, grandiosity in 90%, irritability in 85%, pressured speech in 80%, flight of ideas in 75%, assaultiveness in 70%, hyperactivity in 65%, and hypersexuality in 50%. Euphoria occurred in 15%, the same rate as for psychotic features.
Risk Factors
Shukla et al.
39 found that posttraumatic mania was associated with more severe TBI (long durations of posttraumatic amnesia) among 20 outpatients with relatively severe TBI. It should be noted that study subjects had neurological sequelae and were referred by neurologists, neurosurgeons, and consulting psychiatrists at a large city hospital, leading to selection of more severe TBI cases than usually encountered. Seizures occurred in 50% of their sample of 20 outpatients with posttraumatic mania, a rate 10 times that of the usual seizure rate post-TBI. However, selection of patients with more severe TBI and neurological sequelae might also contribute to the high rate of posttraumatic seizures in the sample. Hypomania and bipolar II disorder were associated with milder trauma defined by briefer durations of posttraumatic amnesia among 20 outpatients with relatively severe TBI. However, chronic hypomania, bipolar I, and schizoaffective disorder were associated with more severe trauma (longer posttraumatic amnesia) in this study.
In the Jorge et al.
45 study, posttraumatic mania was associated with multifocal lesions, primarily in temporal basal polar regions. Posttraumatic mania risk was not associated with posttraumatic seizures, brain injury severity, physical or cognitive impairment, social functioning, or previous family or personal history of psychiatric disorder. Dropouts from the study (35%) significantly correlated with cortical and orbitofrontal lesions. Wilcox and Nasrallah,
50 in searching for preexisting head injury occurring before age 10 in patients with seemingly primary mania, found lesions of the right temporal (two patients), left temporal (one patient), and occipital (one patient) areas among their six patients with posttraumatic mania. Starkstein et al.
41 considered 11 consecutive patients with vascular, tumoral, or traumatic brain lesions and DSM-III major affective disorder, manic episode, two of whom had mania in the wake of TBI. Lesions were present in the frontal lobe in both patients, and one had a brain stem injury as documented by CT. The laterality of the lesion loci was not specified. Moreover, past personal and family histories were not specified in these patients, so it is not clear that these subjects had secondary mania by the criteria of Krauthammer and Klerman.
47Starkstein et al.
52 considered two patients with posttraumatic mania in a series of 12 patients with mania after brain injuries of various types. Presumably, both patients lacked personal and family histories of pertinent psychiatric disorders. Although mania was suggested to correlate with frontal disturbance in both and cerebellar injury in one, CT was apparently obtained only in the patient with the frontal injury and it actually indicated multifocal lesions. Starkstein et al.
53 also noted neuroradiological and metabolic findings in eight patients with mania (all lacked personal histories but one had a family history of mood disorder) after brain injuries of assorted types, but it appears that only two subjects had posttraumatic mania, one with a small right frontal white matter contusion and one with bilateral orbitofrontal contusions. The rest of the subjects appeared to have suffered mania as a sequel to a vascular event. Starkstein et al.
54 later reported bipolar and pure manic states in 19 patients, but it appears that only two suffered traumatic brain injuries, one involving the right orbitofrontal white matter and left temporal tip, and one with bilateral orbitofrontal lesions. Other patients had vascular or tumor lesions, and personal and family histories of mood disorders did not appear to represent exclusion criteria.
On the other hand, in contrast to right hemisphere injuries associated with secondary mania, Lim
55 documented six cases from the literature wherein mania was associated with left hemisphere pathology, including one case following head injury. Lim suggested that the unifying theme reconciling right and left hemisphere associations with posttraumatic mania was involvement of the nondominant hemisphere, although handedness was not established in three of the cases.
Sexual offenses may complicate the course of posttraumatic mania. DelBello et al.
46 assessed 25 convicted sex offenders, six of whom also had a history of TBI and SCID-diagnosed DSM-IV bipolar disorder. They found that sex offenders with bipolar disorder had a higher rate of head trauma than either sex offenders without bipolar disorder or 15 bipolar patients lacking sexual offenses. Head injury preceded commission of the sexual offense in all six subjects. This study suggests that sexual offense may complicate the outcome of bipolar disorder following TBI in selected patients; however, future studies should study the prevalence of sexual offenses in patients with posttraumatic bipolar disorder to establish this potential outcome.
Summary and Recommendations
Diagnostic validity and reliability studies in regard to posttraumatic mania are greatly needed. These studies should consider diagnostic sensitivity and specificity as a function of various inclusion and exclusion criteria.
No firm conclusions can be drawn at this point about incidence or prevalence rates of posttraumatic mania. There is only one study designed to ascertain 12-month posttraumatic mania incidence and prevalence (9.1% in the study of Jorge et al.
45 ) and no studies that assess period prevalence over longer periods. Future studies should follow each TBI patient through specified surveillance periods and determine 1-year rates at varying intervals from TBI onset to take into account posttraumatic mania development after a period of delay. Diagnostic criteria for posttraumatic mania should be clearly specified, including exclusion criteria. Incidence and prevalence rates may vary depending upon other factors as well, such as duration of unconsciousness, posttraumatic amnesia, presence of seizures, penetrating versus closed head injury, other TBI severity indices, study setting, referral base, selection factors, posttraumatic mania diagnostic criteria, diagnostic ascertainment method, and other factors.
Similarly, there is insufficient evidence to form definite conclusions regarding the prevalence of manic symptoms or the characteristics of posttraumatic mania, although two studies
39,
45 found irritability in 85% to 100% and aggression in 50% to 70% of subjects.
The point prevalence of posttraumatic mania in patients with mania would be better viewed as life prevalence of preexisting TBI in patients with seemingly “primary” mania. These data are also problematic, with limitations of recall bias and other methodological concerns, including prevalence period ambiguities. Estimates of 5% in 122 patients,
50 14.3% in 56 patients,
42 and 22.9% in 35 patients
37 span a considerable range, and selection factors are suspect, among other concerns. There is the possibility of modifying population factors, such as neurological patients
43 with a posttraumatic mania point prevalence of 21.4% in 14 patients, and sex offenders
46 with a posttraumatic mania point prevalence of 33.3% in nine subjects. Potential complicating factors include observations of birth injuries in patients with mania
40 and a possible familial predisposition toward head injury.
9 An agenda for future research includes:
1.
Development of a uniform operational definition of posttraumatic mania using DSM-IV or RDC mania, evidence of TBI preceding mania onset, evidence of attribution to TBI, and the absence of clear alternative explanatory etiologies, such as substance use or other neurological illness. The stipulation of additional inclusion (atypical age of onset, specific temporal interval between TBI and mania onset) and exclusion (previous psychiatric illness, family history consistent with bipolar disorder) criteria should be evaluated in future research.
2.
Establishment of the incidence and prevalence of posttraumatic mania using prospective observational studies and standardized diagnostic criteria in TBI rehabilitation settings.
3.
Clarification of clinical and neurophysiological risk factors for posttraumatic mania, such as injury location, cognitive impairment, genetic predisposition, and prior psychiatric illness. Additional factors to be studied would also include postinjury psychotropic treatments (e.g., antidepressants, anticonvulsants) that increase or reduce risk for developing posttraumatic mania.
4.
Determination of the impact of posttraumatic mania on functional outcomes and quality of life posttraumatic stress disorder (PTSD) after TBI.
Posttraumatic Stress Disorder
Nosology
Bryant et al.
56 evaluated 96 survivors of severe TBI 6 months postinjury using a structured clinical interview based on DSM-III-R criteria for PTSD. In this study, the positive and negative predictive power of PTSD symptoms was assessed. The symptoms with the highest predictive power were intrusive memories, nightmares, and emotional reactivity. Those with the lowest power included concentration deficits, detachment, diminished interest, and sense of a foreshortened future. Predictive power defines the specificity of symptoms. Sensitivity was quite different; only 19.2% of patients meeting PTSD criteria experienced intrusive memories, 23.1% had nightmares, and 96.2% experienced emotional reactivity. Warden et al.
57 evaluated 47 active-duty service members with moderate TBI and posttraumatic amnesia lasting at least 24 hours using the PSE and extracting questions consistent with DSM-III-R criteria for PTSD. In this study, no patients met full criteria for PTSD due to the absence of reexperiencing symptoms, though 15% met avoidance and arousal criteria.
These findings are contrasted by the study of Feinstein et al.
58 who examined 282 TBI outpatients a mean of 53 days post injury using the 15-item Impact of Event Scale (IES) which measures symptoms of PTSD divided into two subscales—reexperiencing phenomena and avoidant behavior related to the traumatic event. Patients were divided into four groups based on duration of posttraumatic amnesia ranging from 1 hour to 1 week. There were no group differences in the mean scores on the intrusion subscale, though a subsequent analysis dividing patients into less than or greater than 1 hour of posttraumatic amnesia found more intrusive symptoms with the shorter duration.
Turnbull et al.
59 solicited 371 patients who had been discharged from a trauma center in the previous 6 months, yielding 53 consenting subjects. They were assessed using the IES and the Clinician-Administered PTSD scale for DSM-IV (CAPS-D). Patients were divided into three groups: those with no memory of the event, those with an “untraumatic” memory of the event (i.e., the patient could recall the event but did not recall feeling scared), and those with a traumatic memory of the event. The majority of patients had been assaulted and had posttraumatic amnesia for less than 1 hour. In this sample, patients with no memory or traumatic memories of their injury scored significantly higher on the intrusive and avoidant subscales of the IES. The authors used the IES score as a basis for validating or invalidating a CAPS-D diagnosis of PTSD. Using the CAPS-D alone, 27% of patients met criteria for PTSD. When the authors eliminated patients with low IES scores, that rate fell to 17%. The study is limited by the low response rate, with a predominance of mild TBI due to assault. However, it did employ a novel means of refining the diagnosis of PTSD based on both categorical (symptom presence) and dimensional (symptom severity) criteria that may provide better specificity. Creamer et al.
60 evaluated 301 consecutive patients admitted to a trauma center following mild TBI prior to discharge and 12 months postinjury using the CAPS-D. Of the patients with PTSD at 12 months, there were no differences in reexperiencing, avoidance, or arousal symptom domains in patients with full, partial, or no recall of the injury.
In summary, the phenomenology of PTSD following TBI is similar to that of PTSD without TBI, though there are some inconsistent findings on the presence of reexperiencing symptoms. PTSD with or without reexperiencing symptoms may occur even in the absence of specific memories of the event leading to TBI. It appears to be a contradiction that one can have PTSD without recall of the event. Gil et al.
61 suggested that the traumatic memories could be formed by circuits bypassing cortical structures, leading to implicit (unconscious) memories, or that formation of explicit memories within hippocampal structures might be disrupted by stress-related glucocorticoid surges. In any case, it appears that intrusive memories are not always present in post-TBI PTSD, nor do they rule out the presence of a TBI in patients with PTSD.
Epidemiology
Incidence of Posttraumatic Stress Disorder
Bryant and Harvey
62 assessed 79 patients with mild TBI within 1 month of their injury and at 6 months postinjury using the PTSD module of the CIDI. Acute Stress Disorder was diagnosed in 14% of patients at 1 month, and PTSD was identified in 24% of patients at follow-up. Eighty-two percent of the patients diagnosed with acute distress disorder developed PTSD during the follow-up period. The study was limited by a relatively small sample size for epidemiological purposes but used a standardized and validated diagnostic measure. Gerring et al.
63 evaluated 95 children admitted to a neurorehabilitation unit following severe TBI with a mean coma duration of 11 days. The patients were evaluated using the Diagnostic Interview for Children and Adolescents (DICA), the Child Behavior Checklist (CBCL), and the Psychosocial Adversity Scale early postinjury upon enrollment and then again at 1 year postinjury. In this sample, 13% of patients developed PTSD at 1 year postinjury. In contrast to adult studies, 71% of the children with PTSD experienced intrusive recollections of the event. As described above, Turnbull et al.
59 noted a 27% incidence of PTSD within 6 months post-TBI using a structured instrument based on DSM-IV criteria, and a 17% incidence using stricter criteria that required a minimal level of symptom severity. Gil et al.
61 assessed 120 patients admitted to a trauma center with mild TBI immediately following admission, at 1 week and 3 and 6 months postinjury using the CAPS-D, finding a 14% incidence of PTSD over the 6 month follow-up period. Creamer et al.’s
60 study noted a 10% incidence of PTSD over 12 months postinjury.
Prevalence of Posttraumatic Stress Disorder
Bryant and Harvey
64 compared 46 patients with mild TBI to 59 multiple trauma survivors without TBI at 6 months postinjury using the PTSD module of the CIDI. Posttraumatic stress disorder was identified in 20% of TBI patients and 25% of non-TBI patients. In a separate study, Bryant
65 interviewed 96 survivors of severe TBI 6 months postinjury for the prevalence and influence of PTSD on the recovery process. Despite the fact that most patients had no cohesive recall of the traumatic event, 27% met criteria for PTSD on the Posttraumatic Stress Disorder Interview. A diagnosis of PTSD was also associated with higher scores on the Beck Depression Inventory and General Health Questionnaire.
Glaesser et al.
66 evaluated 46 inpatients on admission to a neurorehabilitation unit at 1 to 82 months postinjury, dividing them into those with more than 12 hours of unconsciousness (N=31) and those with less than 1 hour of unconsciousness (N=15). Diagnosis was obtained using the PTSD module of the SCID. The prevalence of PTSD was 27% in patients with limited or no unconsciousness, and 3% in patients with extended unconsciousness. The low prevalence of PTSD in patients with more severe brain injuries contrasts Bryant’s
65 findings. Limitations of this study include small sample size and greater variability with respect to time postinjury. Thus, strict comparison of the results is not possible.
Sumpter and McMillan
67 assessed 34 severe TBI survivors at least 3 months postinjury using the CAPS-D and the Posttraumatic Diagnostic Scale (PDS), a self-report questionnaire. Though the self-report instrument yielded a 59% prevalence of PTSD, the CAPS-D led to only a 3% prevalence. The authors concluded that the structured interview was a more reliable method of case ascertainment for post-TBI PTSD. Because of the small sample size, no statistical analysis was possible to determine which items on the PDS were most likely to lead to an overreporting of PTSD. Hibbard et al.’s
21 study (described in the section on depression) reported a 19% prevalence of PTSD in patients following TBI.
Risk Factors
Mayou et al.
68 prospectively screened 1,148 individuals who survived road traffic accidents at 3 and 12 months after their visit to the emergency department. They found that the rate of PTSD and other anxiety symptoms 3 months after injury were more common in individuals who had been unconscious than in those who had not been unconscious. At 1 year follow-up, the rates were similar in both groups, by self-report.
As mentioned previously, Bryant et al.
62 noted that 82% of mild TBI survivors with acute distress disorder at 1 month postinjury developed PTSD at 6 months postinjury. This indicates that acute distress disorder is a risk factor for the subsequent development of PTSD. Harvey and Bryant
69 searched for predictors of acute stress disorder in 48 survivors of motor vehicle accident with a TBI using the Acute Stress Disorder Interview (ASDI). The Eysenck Personality Inventory (EPI) and Coping Style Questionnaire (CSQ) were administered to assess coping style. The rate of acute distress disorder was 15%, with an additional 4% meeting subsyndromal criteria. Avoidance coping and BDI scores were significantly associated with a risk of developing acute distress disorder.
Gerring et al.
63 found that female sex and early postinjury depressive and anxiety symptoms identified with the CBCL and DICA were associated with an increased risk of developing PTSD at 1 year in children with severe TBIs and posttraumatic amnesia. Vasa et al.
70 subsequently reviewed brain MRI scans in 95 of the original subjects in Gerring et al.’s
63 study. PTSD was associated with the presence of left temporal lesions, with increased lesion volume increasing the risk of PTSD. Left orbitofrontal cortex lesions decreased the risk of hyperarousal symptoms, while diffuse brain lesions increased the risk of avoidant symptoms. The presence of post-TBI anxiety symptoms was a risk factor for developing PTSD.
Gil et al.
61 assessed 120 patients admitted to a trauma center with mild TBI immediately following admission, at 1 week and 3 and 6 months postinjury using the CAPS-D, dividing the sample into those with (45%) and without (55%) memory of the event. Recall of the event was a strong predictor of PTSD within 6 months postinjury.
Summary and Recommendations
There is substantial evidence that survivors of TBI can develop subsequent PTSD symptoms, even when the traumatic event is associated with altered consciousness and amnesia. Prevalence of the condition ranges from 3% in one subset of patients with more severe TBI, to approximately 27%, which has been reported in several studies. The clinical presentation of PTSD in this population is less clear—some studies indicate a relative absence of reexperiencing symptoms, such as nightmares, intrusive memories, and ruminations of the traumatic event. As a result, the only conclusion the Committee can make is that reexperiencing symptoms does not exclude the presence of a TBI in patients with PTSD. No conclusions regarding the diagnostic validity of reexperiencing symptoms in the post-TBI PTSD syndrome can be made at this time. The clinical course of PTSD following TBI appears to be different from that experienced in non-TBI trauma survivors, particularly in the lower remission rates of acute distress disorder that eventually evolve into PTSD. The most consistent limitations in the literature are the absence of studies with larger sample sizes and the use of the same sample in several reported studies. Recommendations for future research include:
1.
Clarifying the nosology of post-TBI PTSD to address the validity and frequency of hyperarousal, avoidance, and intrusive memories in the diagnostic criteria. Approaches such as Turnbull’s methodology that incorporate symptom severity and symptom clusters may improve the specificity of diagnostic criteria.
2.
Identifying injury-related risk factors, such as severity of injury, duration of posttraumatic amnesia, recall of traumatic events, location of injury, persistent cognitive impairment. In addition, clarifying the neural mechanisms by which patients without recall of the event can experience intrusive memories will be an important step in the validation of diagnostic criteria and increasing understanding of traumatic memory formation.
Posttraumatic Aggression
Nosology
The nosology of aggression and “agitation” is particularly problematic, with a general lack of rigorous definition in the literature. For the purposes of this review, we excluded the literature on posttraumatic aggression that develops in patients emerging from coma. This syndrome has been conceptualized as a form of delirium.
71 The DSM-IV classification system provides the diagnosis of personality change secondary to a general medical condition (APA) with several subtypes to clarify the type of behavior changes manifested. The aggressive type is characterized by predominantly aggressive behavior, which may be directed towards self, others, or inanimate objects. The disinhibited type is characterized primarily by disinhibition and sexual indiscretions, but patients may become aggressive when redirected or frustrated. Patients with the labile type primarily demonstrate affective lability, which may include verbal outbursts with minimal provocation, but without substantial threatening or violent behaviors. To further complicate the diagnostic challenge, impulsive aggression may also occur in the context of a mixed bipolar syndrome. Bipolar symptoms secondary to TBI are frequently characterized by irritability and dysphoria.
39,
72 The appropriate diagnosis for this type of aggressive, dysphoric syndrome is mood disorder secondary to a general medical condition, mixed type (APA). The nosology of posttraumatic aggression may involve considerable overlap between the personality and mood syndromes associated with impulsive aggression. Certain distinguishing symptoms of mania, such as increased energy, reduced need for sleep, pressured speech and racing thoughts, may assist in distinguishing personality from mood symptoms. Rao and Lyketsos
73 propose a nosology that incorporates syndromal intensity and frequency. However, empirical data are lacking to validate the classification of various parameters of post-TBI aggression.
In summary, there is no consistent and validated nosology to characterize posttraumatic aggression in the available literature. The DSM-IV classification system has not been validated for this population and incorporates multiple behavioral domains not directly related to aggression, per se. Since aggression may occur in the context of multiple syndromes, there appears to be little evidence supporting any systematic nosology to characterize various domains of aggression, such as precipitants, impulsivity, and severity.
Epidemiology
Incidence of Posttraumatic Aggression
Tateno et al.
74 evaluated 89 consecutive TBI patients admitted to a hospital service. Using the Overt Aggression Scale (OAS),
75 30 (33.7%) patients were identified as having clinically significant aggression during the first 6 months postinjury. Max et al.
76 evaluated 46 children who were admitted to an acute care hospital following TBI and reevaluated them at 3-month intervals for 1 year. They also evaluated an additional 48 children ages 5 to 14 years who had previously been hospitalized for TBI. A standardized psychiatric interview, the Neuropsychiatric Rating Scale, was used to identify psychiatric symptoms. Thirty-eight percent of the sample developed aggressive behaviors, and nearly 49% developed affective lability and irritability. Onset of these behaviors usually occurred within the first 3 months. Nearly half of these patients had persistent symptoms at 12 months postinjury.
Prevalence of Posttraumatic Aggression
Andrews et al.
77 compared 27 children with TBI with 27 noninjured comparison subjects, all 6 to 17 years old, using the DeBlois Aggressive and Antisocial Behavior Scales. The head-injured children demonstrated greater aggresaggressive/antisocial behavior, though there was no correlation between severity of injury and aggressive behaviors among the patients with TBI. This correlation between TBI and higher aggressive scores is not a specific epidemiological finding but supports the concept of TBI increasing the likelihood of aggressive behavior.
Rosenbaum et al.
78 compared 53 men who physically abused their spouses with 77 men who did not abuse their spouses. A prior history of closed head injuries was present in 53% of the violent men, compared with 19% of the nonviolent men. In this point prevalence study, the members of the aggressive sample were more likely to have had a previous head injury. Though this does not indicate causality, it does support the association between prior TBI and aggression.
Conditions related to agitation and aggression include disruptive behaviors observed in oppositional defiant disorder and interpersonal hostility. Max et al.
79 also followed 50 patients ages 6–14 years after a TBI, using the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Epidemiologic Version (K-SADS-E). This study specifically sought to identify the point prevalence of oppositional defiant disorder at various points before and after an identified TBI. In this sample, 6% of patients had a preinjury history of oppositional defiant disorder. By 12 months postinjury, 18.2% of the sample met criteria for oppositional defiant disorder. This decreased to 14% by 24 months. Loosening the threshold from formal diagnosis to oppositional defiant disorder symptoms, they found that 21.1% of patients developed at least one new oppositional defiant disorder symptom within 3 months postinjury, increasing to 40.9% by 12 months and then decreasing to 34.9% at 24 months. This finding indicates that 20% to 40% of children develop some disruptive behavioral symptoms shortly following TBI. In an attempt to clarify long-term neurobehavioral outcome following TBI, Marschark et al.
80 compared 79 college students with a history of mild TBI as children or adolescents with 93 noninjured students using the SCL-90 and neuropsychological testing. There were no group differences with respect to cognitive functioning, but the students with a history of TBI had higher scores on the symptoms of hostility and interpersonal sensitivity, as well as higher total SCL-90.
Risk Factors
Rapoport et al.
81 followed a cohort of 282 patients with TBI of various severities at 3 months postinjury using the Neurobehavioral Rating Scale–Revised (NBR-R). Severity of injury was defined using criteria from the Glasgow Coma Scale (GCS): a score of less than 12 for mild, 9 to 12 for moderate, and greater than 8 for severe. Subjects with severe injuries were more likely to have higher scores on the hyperarousal and cognitive factor scores on the NBR-R. The hyperarousal factor consisted of excitement, hyperactivity, disinhibition, and unusual thought content. Irritability, emotional lability, and hostility segregated to the emotional factor, which was not correlated with severity of injury.
The study by Tateno et al.
74 examined clinical correlates that predicted aggression following TBI. There were no socioeconomic or demographic differences between the aggressive and nonaggressive groups. Aggressive patients were more likely to have a preinjury history of a mood disorder, alcohol or substance abuse, and aggressive behaviors requiring legal intervention. Frontal lobe lesions were more common in the aggressive patients. There were no group differences in severity of injury, though nonaggressive patients were more likely to have diffuse injuries on neuroimaging. Greve et al.
82 compared aggressive and nonaggressive patients in a residential brain injury facility. A comparison group of 19 residents with no reported behavioral problems was compared with a group of 26 residents with “impulsive aggression” as defined by “persistent uncontrolled loss of temper… manifested by verbal outbursts, striking, throwing, or damaging property, or attacks on other persons within 3 months of evaluation.” The Lifetime History of Aggression questionnaire
83 was used to determine preinjury and postinjury behavioral disturbances, and a neuropsychological battery was administered. There were no group differences in neuropsychological performance. Preinjury impulsive aggression was reported in 75% of the impulsive aggression group versus 26% in the comparison group. In addition, the impulsive aggression group demonstrated higher levels of impulsivity on the Barratt Impulsiveness Scale.
84 These findings suggest that post-TBI impulsive aggression may be an extension of premorbid impulsivity and aggression.
The 2-year follow-up study of Max et al.
85 demonstrated that patients with more severe injuries, lower socioeconomic status, preinjury symptoms of oppositional defiant disorder and preinjury family dysfunction tended to develop more severe aggressive symptomatology. Moreover, these symptoms worsened to a greater degree over time following injury compared with patients without these characteristics.
Dunlop et al.
86 conducted a retrospective chart review study on 193 TBI subjects who had applied for federal disability. Of these, 34 consecutive cases were studied that had evidence of cognitive or emotional deterioration 6 months postinjury as demonstrated by an increase of at least two points on the Neurobehavioral Rating Scale (NBRS) relative to baseline. This sample was matched with a comparison group of TBI patients matched for severity of injury who improved as demonstrated by a decline in two or more points from baseline on the NBRS by 6 months postinjury. In the group that improved, agitation and hostility were noted in 44% of patients between 2 and 6 months, but only 6% of the group developed worsening of agitation after 6 months. By contrast, while 3% of the group that deteriorated had moderate to severe agitation and hostility, 41% of the group developed increasing agitation after 6 months. The group that deteriorated was more likely to have been injured in assaults and less likely to have been injured in motor vehicle accidents. In addition, risk factors for behavioral deterioration included a left parietal injury, skull fracture, and a prior history of alcohol abuse. This report is limited by its retrospective nature and the selection of a sample applying for disability benefits. Agitation and hostility emerged as major factors during follow-up that were associated with the group that had deteriorated.
Another risk factor for posttraumatic aggression appears to be prior episodes of head injuries. Carlsson et al.
87 compared 1,112 men ages 30, 50, and 60 years from a general population. Though age at time of injury did not affect the presence of irritability, the presence of two or more injuries with loss of consciousness was significantly associated with irritability. The symptom of irritability was not clearly defined or associated with verbal or physical aggression.
Summary and Recommendations
The current literature is severely limited by a lack of consistent methodology for identifying aggression and agitation. Moreover, there is a tremendous lack of clarity and consistency of terminology, rendering comparisons of studies difficult. There are a number of instruments, such as the Overt Aggression Scale
75 and Neurobehavioral Rating Scale,
88 that may be used effectively to identify and monitor change across time. However, these instruments are dimensional in nature, measuring the severity and frequency of aggressive behaviors. Establishing specific thresholds for mild, moderate, and severe aggression would further refine their utility. Other epidemiological studies make use of symptom domains or DSM diagnoses of personality disorders. However, there has been little use of the diagnosis of personality change due to a general medical condition, aggressive type, in studies using DSM diagnoses. As a result, existing epidemiological studies of DSM diagnoses offer little insight into the prevalence and incidence of posttraumatic aggression. The challenge of assessing and monitoring post-TBI aggression is complicated by the fact that this symptom may present in a variety of clinical syndromes, such as personality changes, delirium, and mania. Clearly, more research is needed to establish a consistent operational definition of posttraumatic aggression for the purposes of epidemiological and treatment research.
Of the three prospective studies reviewed, agitation and aggression developed in 20% to 49% of child patients and approximately 33% of adult patients, with onset usually within the first year postinjury. Patients with frontal lobe lesions, a preinjury history of substance abuse, or impulsive aggression appear to be at higher risk for developing post-TBI aggression. However, it is difficult to differentiate posttraumatic aggression from preinjury aggression, and no published studies definitely demonstrate that head trauma increases aggressive behavior in premorbidly aggressive individuals. There is inconclusive evidence regarding a relationship between cognitive functioning and the development of post-TBI aggression, though it is possible that the neuropsychological batteries were unable to detect subtle executive functions mediated by the frontal lobes.
89 As a result, the connection between dysexecutive symptoms and aggression may not be identified. Likewise, there is inconsistent evidence defining the impact of socioeconomic status and severity of injury on development of posttraumatic aggression. Future research is necessary to accomplish several goals:
1.
To operationally define posttraumatic aggression using both categorical and dimensional terms. The Overt Aggression Scale provides a framework for addressing frequency and severity variables within the construct of aggression, as well as differentiating between aggression toward self, others, and property. Other factors to be considered are precipitants and interepisode mood and affective states.
2.
To clarify and validate a systematic nosology for posttraumatic aggression using DSM-IV diagnosis of personality change due to a general medical condition as a reference point.
3.
To clarify the incidence, prevalence, and natural time course of posttraumatic aggression in large prospective studies of TBI survivors.
4.
To identify neuropsychological and clinical correlates that are predictive of the development of posttraumatic aggression.
5.
To elucidate the neural substrates of posttraumatic aggression through functional neuroimaging studies.
6.
To clarify the relationship between posttraumatic aggression and psychosocial functioning with respect to family and social relationships, vocational functioning, and costs of care (direct and indirect). This would require the development of appropriate quality of life and functional assessments related specifically to psychiatric symptomatology.
CONCLUSIONS
The literature on post-TBI psychiatric disorders is laden with limitations related to sample size, diagnostic criteria, and overall study design. As the field has evolved, however, there appears to be a trend toward rigorously designed studies that employ gold-standard assessment tools in a prospective manner, though the validation of these gold-standard tools in this special population is ongoing and currently incomplete. Sample size and selection, use of validated nosologies with appropriate inclusion and exclusion criteria, uniform ascertainment methodologies, and defined surveillance periods remain fairly consistent limitations, though studies are emerging in the literature that will address these concerns. There remain significant opportunities to systematically assess the nosology, epidemiology, and risk factors of these disorders. The TBI Model Systems network, with 16 sites within the United States, is a favorable setting in which to incorporate such systematic prospective studies, which will lay the foundation for rigorous treatment studies designed to reduce the impact of these disorders on postinjury recovery and functioning. Because of the capacity of each site to study the natural course of TBI treatment and rehabilitation from acute intervention through community reentry using standardized enrollment and outcome measurement procedures, the TBI Model Systems is capable of providing adequate size and scope to provide answers to many of the nosological and epidemiological questions that have thus far eluded single center studies. The incorporation of a prospective, systematic effort to classify and characterize the clinical course of neuropsychiatric sequelae of TBI within this existing framework would greatly expedite progress toward greater understanding of the etiology and treatment of these disorders.