O pioids may have an antidepressant effect in patients with affective disorders.
1 –
3 Opioids have been used successfully to treat refractory depression in monotherapy and as an augmenting agent when added to antidepressant medication. Specific opioids suggested to have this property include the mu-opioid agonists oxycodone, oxymorphone, tramadol, codeine, and the partial agonist buprenorphine.
4 –
7 The induction of hypomanic/manic symptoms, especially in patients with known bipolar disorder, would be evidence that an opioid has mood-elevating properties. A few case reports have noted hypomanic/manic symptoms associated with the use of opioids.
8 –
10 Externally administered endorphins, which are endogenous agonists at the same receptor site as exogenous opioids, have also been reported to induce manic reactions in psychiatric patients.
11No studies have investigated the affective response in a group of patients with bipolar disorder who have been prescribed opioids. One study investigated the antidepressant effect of an opioid, buprenorphine, in 10 patients with major depressive disorder.
7 Administration of opioid analgesics in patients with known bipolar disorder provides an opportunity to observe any opioid-related mood-elevating changes. Many patients with bipolar disorder are prescribed opioids for pain conditions. This naturalistic clinical setting provides useful preliminary information on this topic. In this study, we examined mood activation in a group of adult outpatients with known bipolar disorder in psychiatric treatment who had been prescribed an opioid analgesic for pain by another physician.
METHOD
We obtained informed consent from all patients and all healthy comparison subjects after the study had been fully explained. The patients in this study were 45 consecutive adult private outpatients under the care of two board-certified psychiatrists (C.B.S. and L.C.S.), who each had 25 years’ experience and specialized in the treatment of bipolar disorder. All of the patients were 18 years of age or older and had a DSM-IV diagnosed bipolar disorder and were currently being treated with psychotropic medicines. Patients were not excluded because of a concurrent medical condition. We took a history of opioid analgesic use in the past for pain for each subject, and recorded the name and pattern of use of the opioid. We also documented the psychotropic medicines used concurrently with the opioid analgesic, and noted the bipolar disorder classification for each patient. Gender and age of all subjects were obtained.
We retrospectively obtained the mood reactions of patients to opioids, and noted the preexisting mood state prior to opioid use. The change in the patients’ mood status associated with taking the opioid analgesic was rated on the Clinical Global Impression Scale–Bipolar Version (CGI-BP).
12 We identified a clinically significant mood-elevating response to the opioid for subjects who experienced a hypomanic/manic syndrome as defined by DSM-IV and whose change in symptoms was considered much worse or very much worse on the Change Item (IIa) of the CGI-BP. We also assessed the antidepressant effect in the patient group by using the CGI-BP. A clinically significant antidepressant response was noted in depressed patients who reported an antidepressant response from opioids considered much or very much improved on Change Item IIb.
The comparison group comprised adults who were significant others of patients with bipolar disorder in the general population of the patients we treated. They were not related to the patients and did not have a history of a DSM-IV diagnosed mood disorder. We asked members of the comparison group if they had ever taken opioid analgesics in the past, and assessed retrospectively the effect of the opioid on the mood status of the comparison group using the CGI-BP as described above for the patient group.
The activation data between comparison subjects and patients who had used opioids were compared utilizing Fisher’s exact test. We had a clear hypothesis of the direction of the results and literature supporting this direction. We tested our prediction that the bipolar disorder patients would have significantly more opioid-induced activation than the comparison subjects at the 0.05 level of significance.
RESULTS
The average age of the 33 bipolar patients who took opioid analgesics was 57.2 (SD=11.0), and the average age of the 21 comparison subjects who took opioid analgesics was 55.7 (SD=11.6). Twenty-two (67%) of the 33 bipolar subjects receiving opioids were female, and four (19%) of the comparison subjects receiving opioids were female.
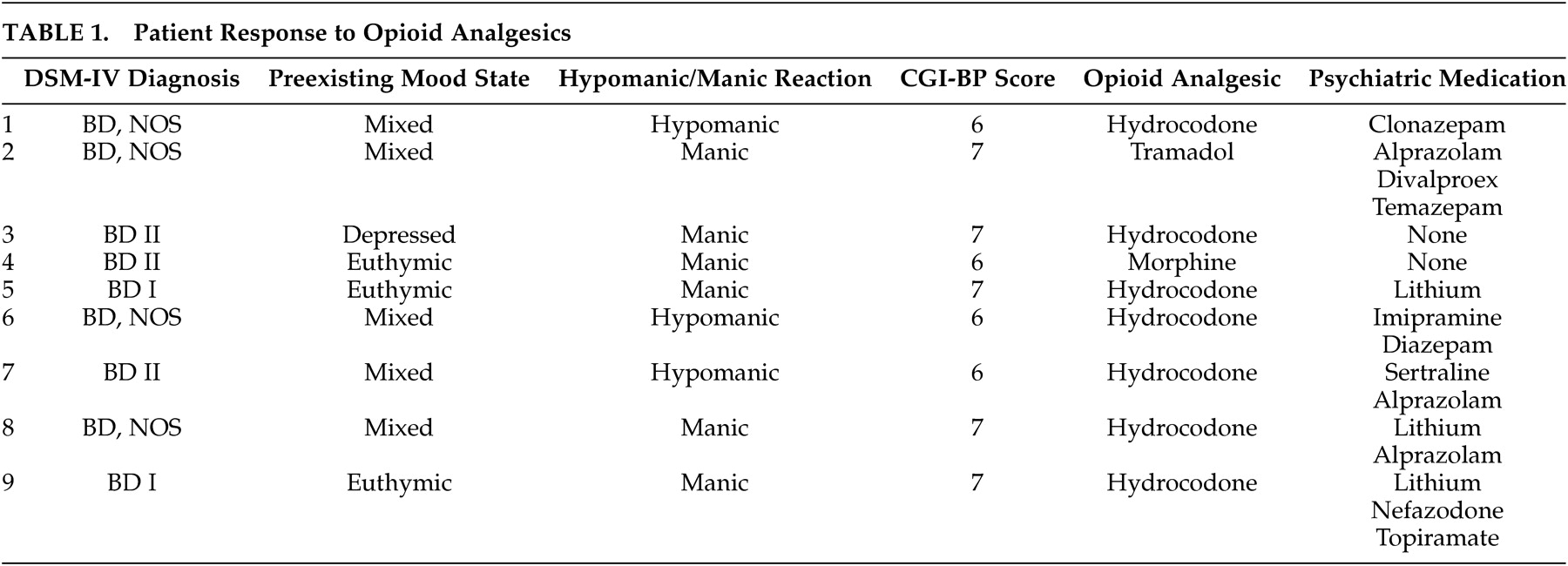
Twelve of the 45 subject patients with known bipolar disorder had never taken an opioid analgesic. Of the remaining 33 patients, nine (27%) experienced a significant hypomanic/manic reaction which was severe enough to obtain a score of 6 (much worse) or 7 (very much worse) on Item IIa (mania change) of the CGI-BP Scale (
Table 1 ). The preexisting mood state and other clinical variables also can be found in
Table 1 .
The hypomanic/manic reaction was associated with the use of hydrocodone in seven of the nine patients who experienced this reaction. Four of these patients were taking a medicine with antimanic properties at the time of the reaction (
Table 1 ).
Two of the 24 patients who did not experience a hypomanic/manic reaction instead reported a much or very much improved antidepressant effect (Item IIb of the CGI-BP scale) during a depressive episode. Both patients acknowledged that they took the opioid analgesics for mood-elevating properties when they were depressed because of this effect.
Twenty-three comparison subjects were investigated. Twenty-one of these 23 recalled receiving opioid analgesics. None of these 21 subjects receiving opioid analgesics experienced a hypomanic/manic reaction as measured by Item IIa of the CGI-BP Scale. Some controls reported euphoria, but no reaction approaching hypomanic or manic syndrome. We compared activation in patients and comparison subjects who received opioid analgesics using Fisher’s exact test and found a significant difference (p<0.01).
As there were clear gender differences between the patients and comparison subjects, we examined the gender pattern of activation in the bipolar subjects. Six (67%) of the nine subjects who were activated were female, and 22 (67%) of the 33 opioid-receiving bipolar subjects were female.
DISCUSSION
The results of this study indicate that opioid analgesics, especially hydrocodone, can precipitate a hypomanic/manic reaction in a significant percentage of patients with bipolar disorder and have an antidepressant effect in others. The occurrence of a hypomanic/manic episode in patients receiving opioid analgesics may be a clue to an underlying bipolar disorder in patients who have not been previously so diagnosed. Moreover, patients with a known bipolar disorder should be alerted to the risk of an exacerbation of hypomanic/manic symptoms when they take opioids. Bipolar patients taking maintenance opioids for chronic pain should be periodically assessed to determine whether they are misusing the opioid to self-medicate their depressive symptoms. Four of the nine bipolar subjects who had a hypomanic/manic reaction to opioid analgesics reported that they were faithfully taking prescribed antimanic medication at the time, indicating that antimanic agents might not be protective against this opioid-induced reaction.
As indicated in the table, three of the nine patients who experienced a hypomanic/manic reaction were on a maintenance schedule of antidepressant medications at the time of the activation. The occurrence of this reaction was associated with the introduction of opioids and not the initiation of an antidepressant.
As noted earlier, investigators have found that opioid receptor agonists may have antidepressant properties. Therapeutic medications can affect multiple neurotransmitter systems. One theory proposed for the mood-elevating effects of opioids involves interactions between opioid and dopamine systems. Relevant literature links dopaminergic function with depression and motoric/cognitive hyperactivity.
13,
14 Further, some opioids, such as meperidine
15 and tramadol,
16 have serotonin reuptake properties which might account for mood-altering effects.
This study has limitations. Data were collected retrospectively, and blind assessments were not performed. The course of the bipolar illness may change unrelated to the use of opioids. However, some subjects in this study could often identify multiple occasions in which activation occurred in conjunction with opioid use. Furthermore, the data should be interpreted with some caution as the sample size was relatively small and the gender distribution between groups was different. One should not assume that female bipolar patients are necessarily more at risk for hypomanic/manic activation due to opioids than male patients; the gender ratio for the activated group is identical with the gender ratio of the bipolar subjects receiving opioids. Our findings invite future prospective clinical studies.