A ccumulation of β-amyloid peptide in the brain parenchyma and vasculature is associated with Alzheimer’s disease.
1 Relative to healthy comparison subjects, plasma β-amyloid levels are elevated in dementia and in the sporadic Alzheimer’s disease risk factor e4 variant of apolipoprotein E (APOE).
2 However, the relationship between cognitive impairment and disease course is complex. Many researchers find no evidence for a link between β-amyloid and Alzheimer’s disease progression,
3,
4 though this may reflect the nonlinear relationship between cognitive function and β-amyloid levels. For example, recent longitudinal evidence suggests that elevated plasma β-amyloid levels are present in some individuals before and in the earliest stages of the Alzheimer’s disease process but decrease over time.
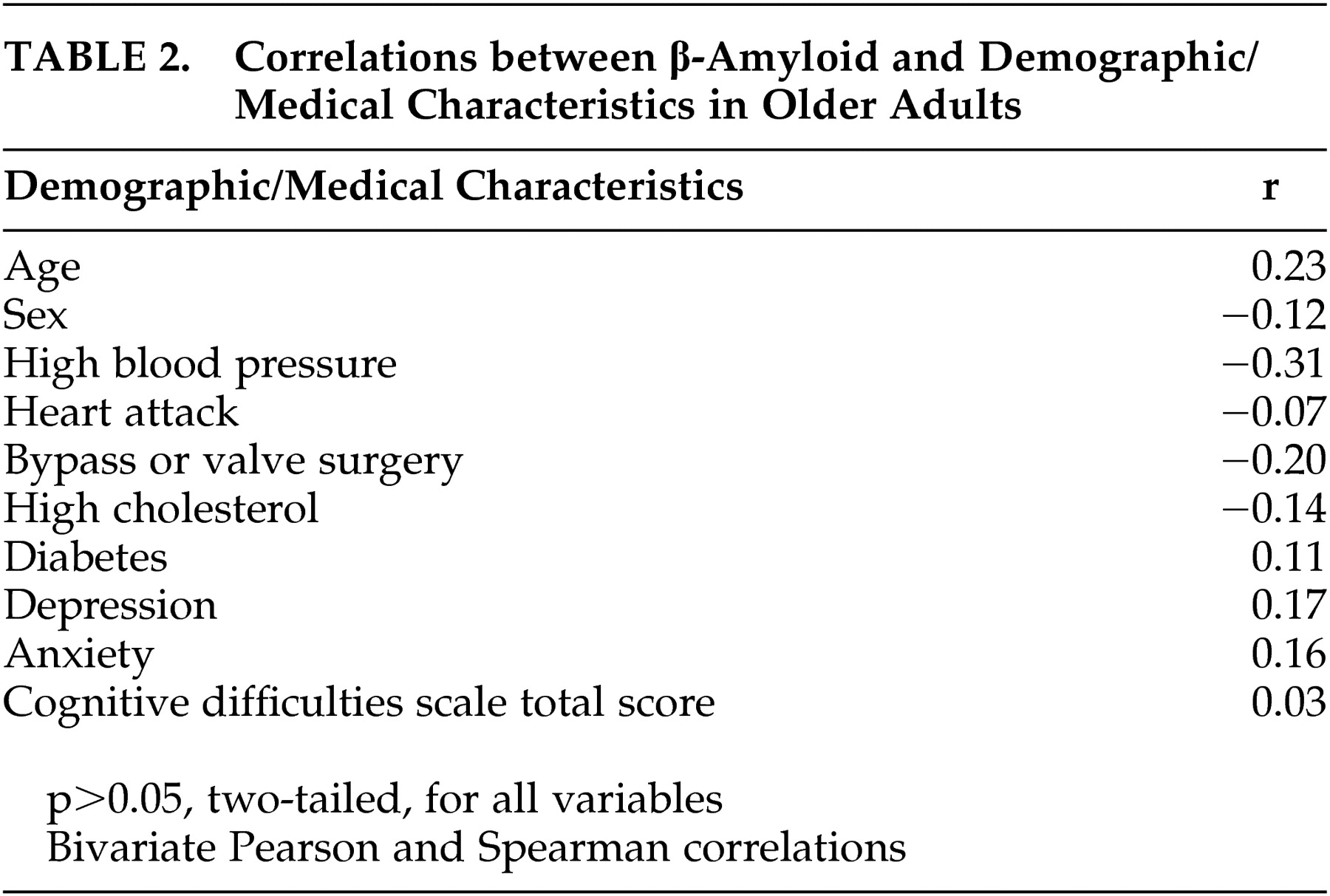
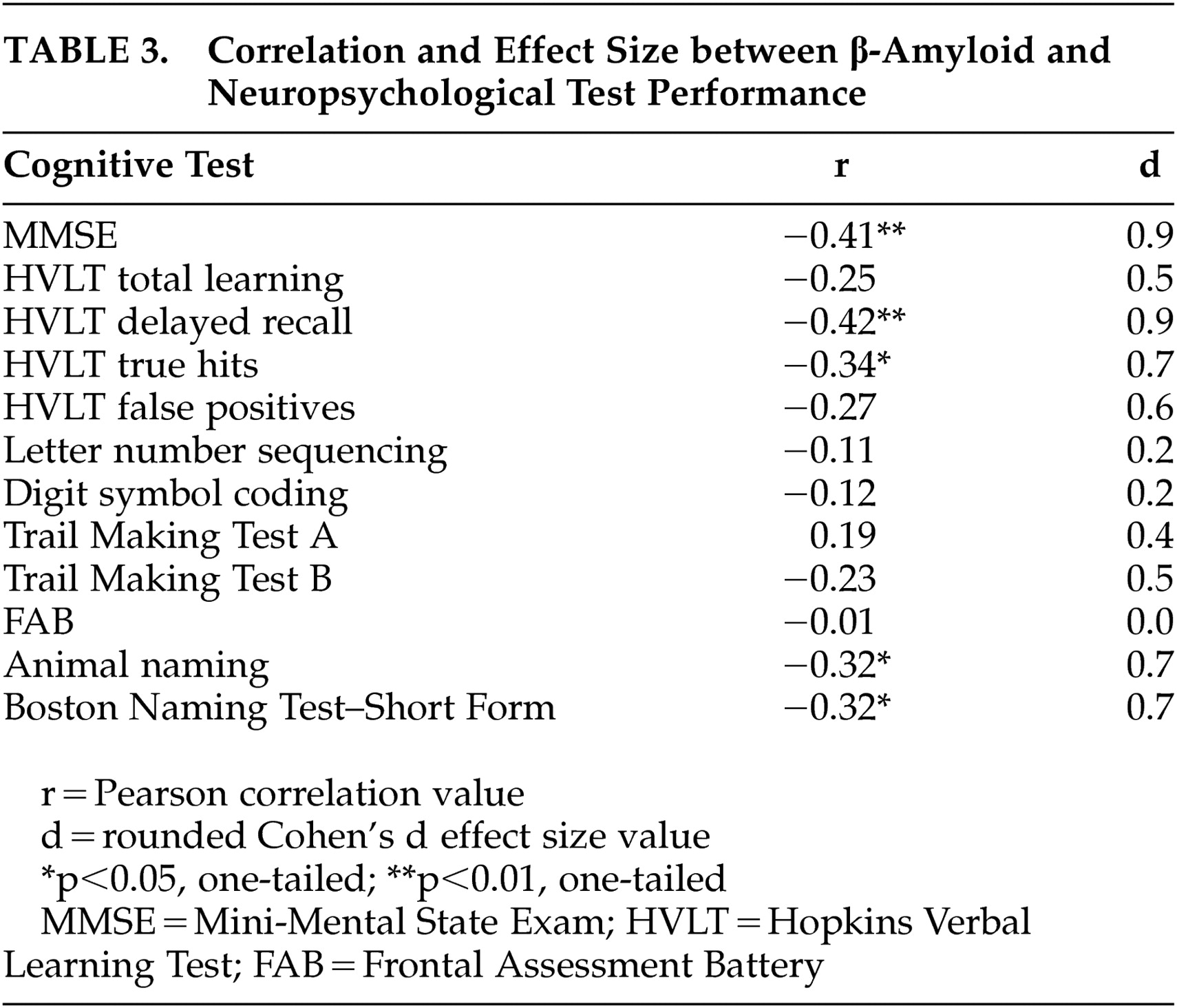
5 The relationship between cognitive function and β-amyloid elevation in older adults without neurological conditions is currently unknown. Greater understanding of this relationship may accord key insights into the mechanisms by which β-amyloid affects the brain in the early stages of Alzheimer’s disease. Based on the current literature suggesting that elevated plasma β-amyloid levels are associated with aging and are present prior to the early stages of Alzheimer’s disease, we hypothesized that there would be a negative relationship between cognitive performance and plasma β-amyloid levels.
The following procedures were approved by the local institutional review board. All participants provided written informed consent prior to study involvement.
Procedure
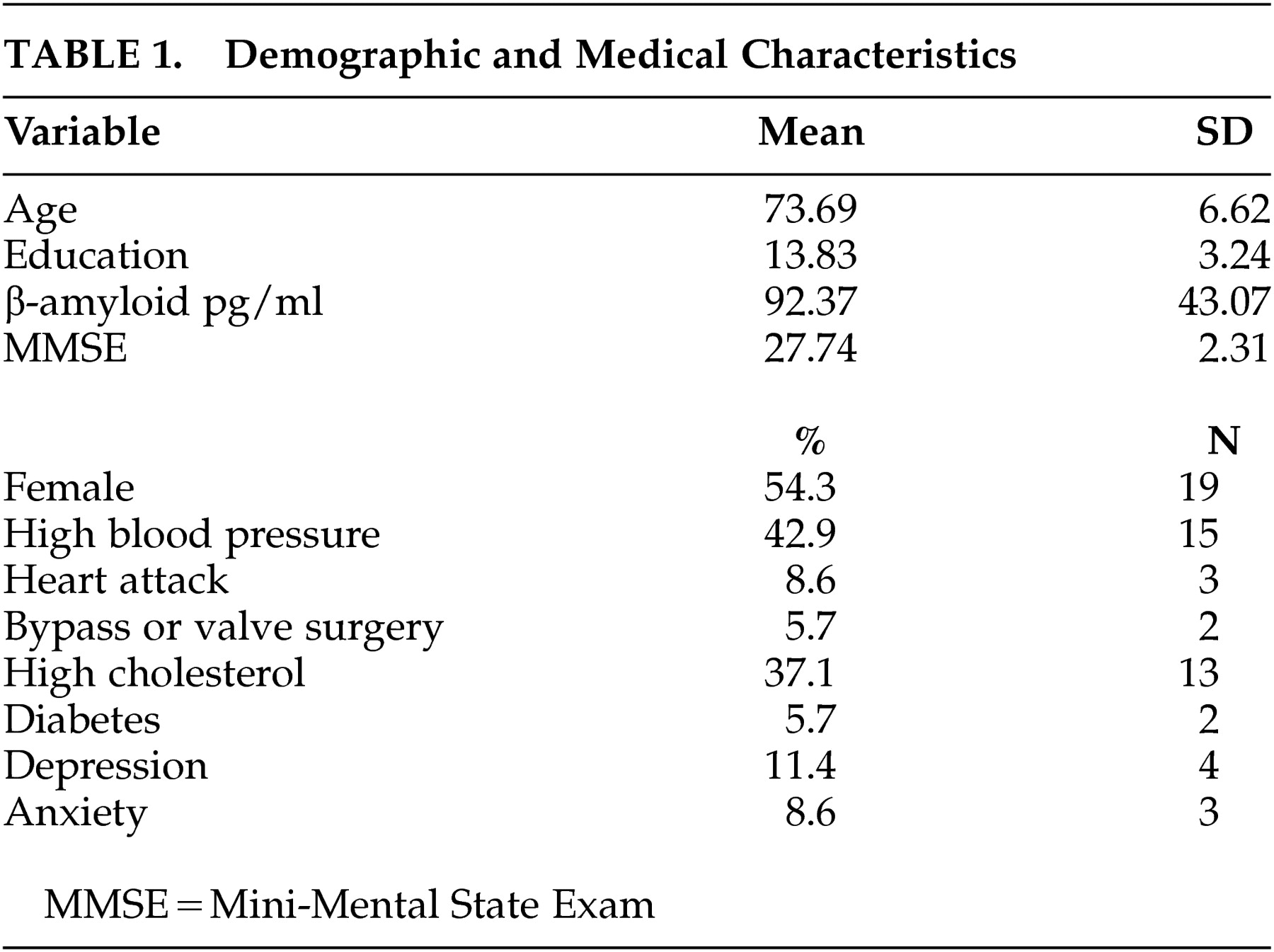
Participants provided written informed consent, underwent fasting blood draw, and were provided a small snack. Self-reported history of medical and psychological disorders was obtained from participants on a brief checklist. The neuropsychological test battery was then administered by trained research team members under the direction of a clinical neuropsychologist (JS, MBS). Specimens were collected by venipuncture in serum separator tubes and allowed to clot for 30 minutes at room temperature. After centrifugation for 15 minutes, the serum was aliquoted into 1.8 ml Nunc™ CryoTube vials and frozen at −80°C until the time of analysis. All variables showed expected distributions, and no transformations were performed.
DISCUSSION
Consistent with predictions, the current study demonstrates an inverse relationship between β-amyloid and performance in several cognitive domains, including global cognition, verbal learning and delayed recall, semantic verbal fluency, and confrontation naming. These relationships exist in the presence of intact global cognition, as the average MMSE score in the sample was above 27.
Although the mechanisms for the relationship between cognitive function and β-amyloid are not entirely clear, the cognitive domains negatively associated with β-amyloid level in the current study reflect those abilities that are frequently impaired in the early stages of Alzheimer’s disease.
15 Such findings suggest that a percentage of the participants in the current study, despite no history of dementia and current global cognition within normal ranges, may convert to pre-Alzheimer’s disease (i.e., mild cognitive impairment) in the near future. This would be expected, in fact, based on the prevalence of Alzheimer’s disease in older adults living in the community
16 and would be consistent with longitudinal evidence demonstrating elevated β-amyloid in some individuals prior to early stages of the Alzheimer’s disease process.
5A primary limitation of the current study includes its cross-sectional methodology, which does not permit examination of the relationship between β-amyloid and cognitive function over time. Given previous research indicating that β-amyloid level is elevated prior to developing Alzheimer’s disease,
5 and that base rates suggest that a proportion of the current study’s sample will develop Alzheimer’s disease in the future, longitudinal study is essential to the investigation of the relationship between β-amyloid and cognitive function in participants who develop Alzheimer’s disease in the future versus those who remain cognitively intact. Future studies would also benefit from the use of an expanded neuropsychological test battery (e.g., visual memory, specific aspects of attention and executive function) and a detailed assessment of family history of neurological conditions (e.g., Alzheimer’s disease, vascular dementia) to further clarify relationships. Similarly, studies employing large sample sizes are needed to help clarify the possible effects of different medications on both β-amyloid and cognitive function in healthy older adults. A growing number of medications have been suggested as having neuroprotective effects and may be implicated in β-amyloid-related processes.
Future research should also consider mediating variables between β-amyloid and cognition, particularly the possible moderating effects of various medical conditions. For example, recent research indicates that there are strong relationships between cardiovascular and physical health and both β-amyloid and cognition.
17 –
19 Such findings would suggest that improved cardiovascular fitness could suppress β-amyloid accumulation and thus influence its relation to cognitive function. Recent studies showing that exercise provides neuroprotection may be illustrating this possible effect.
20 Similarly, there is growing evidence that serum markers associated with cardiovascular dysfunction may be implicated in the development of Alzheimer’s disease. For example, a study by Irizarry et al.
21 links C-reactive protein to elevated risk of Alzheimer’s disease and suggests that homocysteine may interact with homocysteine to potentiate neurodegeneration in Alzheimer’s disease. Further work, particularly pathology studies, might determine the mechanisms by which β-amyloid is associated with cognitive function in healthy older adults and clarify their long-term outcome.
In summary, the current study extends previous work to show that cognitive function is inversely related to β-amyloid level in healthy older adults. Further work is needed to clarify possible mechanisms for these findings, particularly longitudinal and pathology studies that consider possible mediator variables.