T here is growing evidence that physical injury during deployment is associated with a higher prevalence of mental health issues post-deployment.
7 Military personnel are returning from combat with different levels and types of injury than in previous wars. This is partially due to more rapid and sophisticated medical response on the battlefield and to improved protective equipment such as Kevlar vests.
8,
9 These protect soldiers from mortal internal injuries but not from extremity trauma or concussive brain injuries. Recent studies detailing the most common injuries have found that approximately one-half involved the head or neck.
10,
11 The great majority of injuries were due to explosions, and many involve more than one area of the body (polytrauma).
9 Several studies from the Defense and Veterans Brain Injury Center (DVBIC) of soldiers returning from Afghanistan or Iraq document the occurrence of traumatic brain injury (TBI) in many soldiers.
12 –
15 A history of experiencing physical injury during deployment is associated with a higher prevalence of post traumatic stress disorder (PTSD) post-deployment.
7 A recent survey study of soldiers following return from deployment reported that ∼9% of military personnel who had not been injured while deployed screened positive for PTSD.
1 The rate was almost doubled (∼16%) in those reporting bodily injury during deployment. This rate is very similar to an earlier study assessing the increased risk for PTSD due to combat-related injury.
16 Another post-deployment survey study reported an increased incidence of PTSD with number of injury mechanisms: ∼14% for one, ∼29% for two, and ∼51% for three or more.
2 These results are consistent with the incidence of PTSD symptoms following significant orthopedic trauma in civilians.
17,
18Although at one time it was believed that the loss of consciousness and memory deficits that frequently result from TBI made it unlikely that PTSD would develop, recent studies have found that PTSD can develop even when the patient has no conscious memory of the traumatic event.
19 –
22 Studies in military personnel indicate that higher rates of PTSD are associated with having experienced potentially brain-injuring conditions (
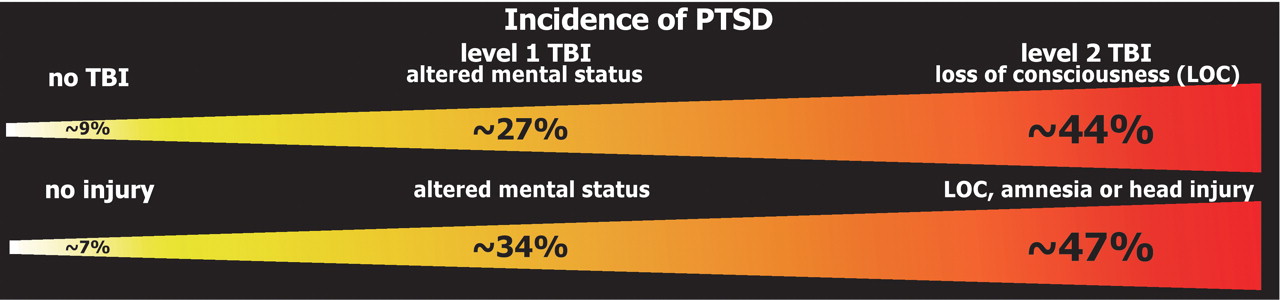
Figure 1 ).
7 In a group who reported experiencing a concussion while deployed (as indicated by altered mental status, n=260), ∼27% screened positive for PTSD.
1 The rate was ∼44% in those who reported a loss of consciousness (n=124). In another survey study the rate of PTSD was ∼7% in those without evidence of brain injury (n=1,960), ∼34% with level 1 mild TBI (altered mental status, n=163), and ∼47% with level 2 mild TBI (loss of consciousness, amnesia, or head injury, n=112).
2 Similarly, an inpatient study of service members who had experienced both a burn and blast injury (n=76) found that 32% were positive for PTSD.
23 The rate of PTSD was 22% in the group without and 45% in the group with mild TBI. A retrospective study in combat veterans found that head injury was associated with increased frequency of PTSD, and combat-related head injury was associated with increased severity of PTSD.
24 There is also evidence that veterans with combat-related PTSD have more severe symptoms than veterans with PTSD due to noncombat-related events.
25 Increased incidence of PTSD in military personnel experiencing TBI is consistent with research studies in other populations. These have concluded that development of psychiatric symptoms following TBI is relatively common, with 13%–27% exhibiting PTSD.
26,
27Recent reviews provide an excellent summary of what is presently known about the functional neuroanatomy of PTSD.
28 –
31 In brief, symptom provocation studies have implicated anterior limbic-related areas in PTSD including regions in the medial prefrontal, anterior cingulate, orbitofrontal, insular, and medial temporal cortices as well as the amygdala. Cognitive activation studies indicate increased amygdalar and decreased medial prefrontal cortical responding to threat, and impaired responding in rostral anterior cingulate cortex to emotional tasks. Some morphometric studies have reported decreased volume in several limbic-related areas, including hippocampus, rostral anterior cingulate, dorsal anterior cingulate, and subcallosal cortices.
A critical issue is determining whether particular anatomic or functional differences that have been associated with PTSD preexisted the trauma exposure or arose afterward.
32 Preexisting differences may indicate risk or vulnerability factors, whereas differences that arise after exposure are more likely to be consequences of the traumatic event and/or the development of PTSD. A series of case-control studies utilizing Vietnam Era veterans and their identical twins have shed light on this key question.
3,
33,
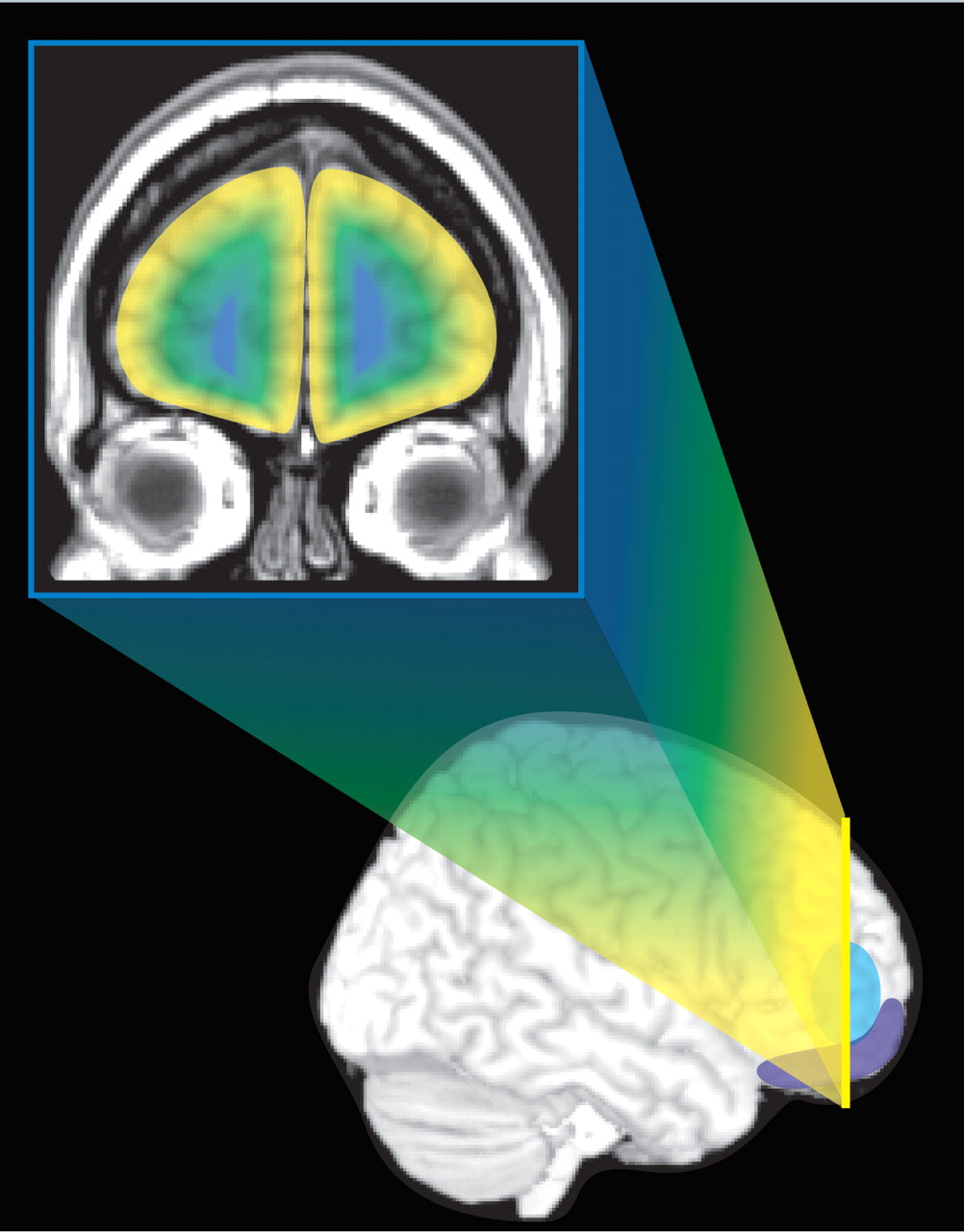
34 Overall, these studies support increased incidence of neurological soft signs, presence of cavum septum pellucidum and perhaps smaller hippocampal volume as preexisting factors. Interestingly, average neurological soft signs score correlated with total gray matter but not with total white matter volume. As noted by the authors of these studies, the findings may be indicative of subtle neurological compromise as a risk factor for PTSD. Increased reactivity to sudden loud sounds (as indicated by heart rate) and decreased gray matter volume in the hippocampus and several limbic-related areas of the cortex (
Figure 2 ), on the other hand, were more likely to have arisen subsequent to trauma exposure and the development of PTSD. These findings indicate that longitudinal changes may occur, supporting the concept that early intervention has the potential to change the trajectory of the illness.
Achieving a better understanding of the possible interactions between TBI and PTSD is of great clinical importance. If areas implicated in PTSD or their interconnecting pathways have been injured, symptom severity and/or response to treatment may be altered. A recent series of studies of pediatric (ages 4–19 years) severe (Glasgow Coma Scale 3–8) closed head injury provides some insight into the interaction between focal brain injury and the development of psychiatric symptoms (
Figure 3 ).
5,
6,
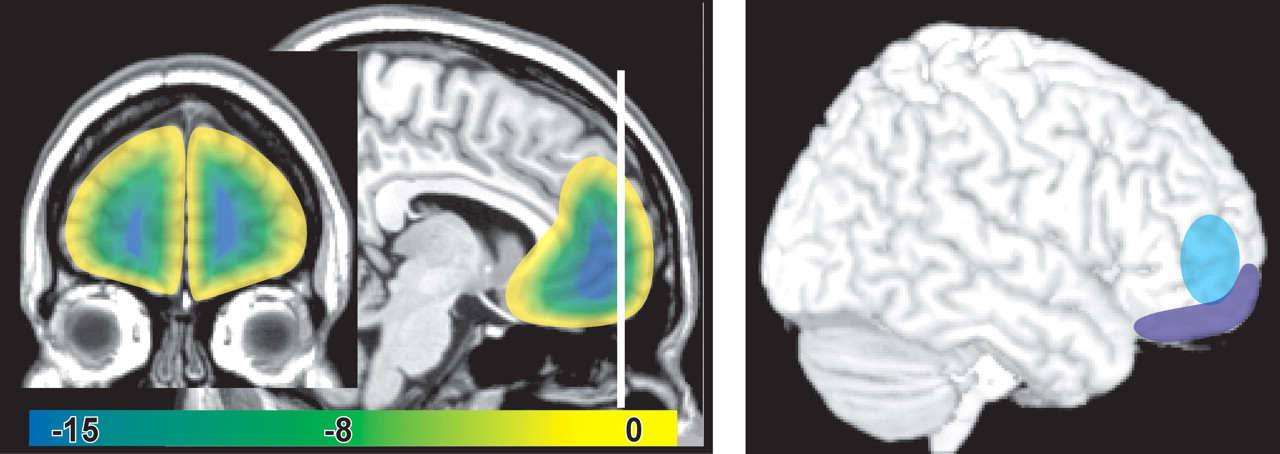
35 One study examined the correlations between injury locations and both the formal diagnosis of PTSD and probability of satisfying the specific diagnostic criteria (reexperiencing, hyperarousal, avoidance).
5 Meeting all three diagnostic criteria (9/94, 10%) was associated with a higher lesion burden in the middle temporal gyrus and a lower lesion burden in the medial frontal gyrus. Satisfying the reexperiencing criterion (41/94, 44%) was associated with a lower lesion burden in the cingulum, medial frontal gyrus, and hippocampus. Satisfying the hyperarousal criterion (55/94, 59%) was associated with a lower lesion burden in the subcallosal gyrus. Satisfying the avoidance criterion (12/94, 13%) was associated with a higher lesion burden in the middle temporal gyrus and a lower lesion burden in the medial frontal and inferior temporal gyri. A later analysis reported a higher lesion burden in the orbitofrontal cortex was associated with a lower probability of developing PTSD (
Figure 3 ), whereas a higher lesion burden in the temporal lobe was associated with a higher probability of developing PTSD.
6 Higher lesion burden in orbitofrontal cortex was also associated with decreased probability of developing obsessive-compulsive disorder.
35 Similarly, a study of Vietnam veterans with combat-related penetrating head injuries reported that injury to ventromedial prefrontal and anterior temporal cortices was associated with a lower probability of developing PTSD (
Figure 3 ).
4 PTSD was present in 40% of veterans with TBI, but without injury to either of these areas (n=133). This was similar to the incidence of PTSD in veterans without TBI (48%, n=52). Only 18% of veterans with injury to the ventromedial prefrontal cortex had PTSD (n=40). Of particular importance, PTSD was not found in any veteran with injuries that included the amygdala (n=15). This was a very specific association, as 32% of veterans with injury to anterior temporal and/or medial temporal areas, but no injury to the amygdala (n=28), had PTSD, as did 44% of veterans with injury to the hippocampus but not the amygdala (n=9).
Another factor that complicates both diagnosis and clinical management is the widely acknowledged overlap between the symptoms common following TBI and those of PTSD.
7 This is likely a contributing factor to the underrecognition of mild TBI, as has been reported in a study of combat veterans diagnosed with PTSD.
36 The need for measures that can reliably differentiate these conditions was recognized more than a decade ago.
37 The overlap of symptoms also suggests the possibilities of symptom aggravation due to additive effects and/or alterations in resilience/coping. Several studies support the idea that presence of TBI can influence the expression of symptoms in PTSD.
6,
38 –
40 At minimum, presence of TBI requires alterations of PTSD treatment approaches to adjust for common cognitive and emotional deficits (e.g., concentration, memory, emotional control).
41,
42Recent studies have begun to provide insight into the influence of specific symptoms or cognitive/emotional deficits on response to particular treatment approaches. Exposure therapy presumably works by promoting habituation/extinction of the overly fearful response to a stimulus that is no longer threatening.
43 This is an effective approach for many, but not all, patients with PTSD. A study utilizing a group of patients with PTSD who had not responded to prolonged exposure therapy found that most (18/23) achieved recovery following imagery rescripting and reprocessing therapy (a form of cognitive restructuring therapy).
44 The authors of the study suggest that cognitive restructuring therapy may be more efficacious in patients whose predominant PTSD-related emotions are guilt, shame, or anger rather than fear. Another study measured multiple aspects of memory and attention in a group of female patients with PTSD prior to initiation of cognitive behavior therapy (CBT).
45 PTSD symptom severity was assessed prior to and following eight sessions of CBT. Seventy percent of the group (16/22) had symptom reduction sufficient to no longer meet DSM-IV criteria for PTSD. Response to treatment, as measured by the Clinician Administered PTSD Scale (CAPS), was not related to measures of attention or digit span. Response to treatment was predicted by performance on story recall (immediate) even after controlling for differences in initial symptom severity and attention performance.
Other neuropsychiatric issues may also arise following TBI, including depression, personality changes, substance use disorders, aggression, and impulsivity.
27,
46,
47 These conditions complicate clinical management and can impair recovery and psychosocial outcome. To date, when patients have both diagnoses, there is no clearly defined way to distinguish which condition is responsible for symptoms that cross both domains (e.g., decreased focus and concentration, decreased sleep, agitation, irritability, inability to maintain employment or schooling). Therefore, establishing a clear symptom delineation, prognosis, and long-term treatment planning is extremely challenging.
46 There are no currently FDA-approved medications for the long term treatment of psychiatric symptoms due to brain injury.
48 –
51 The few studies on rehabilitative approaches are promising but inconclusive.
52 –
54