P sychosis in epilepsy patients has long been studied as an organic model of endogenous or functional psychotic disorders. Among various epileptic syndromes, temporal lobe epilepsy (TLE), or psychomotor epilepsy in earlier literature, is believed to have the highest susceptibility to psychosis, both acute and chronic,
1 –
4 although some authors argued against this notion.
5 –
6 Apart from the dispute over the highest incidence of psychosis in TLE, various factors influencing the occurrence of psychosis in patients with TLE have been studied, including age, duration of the illness, seizure frequency, side of the focus, and pathology of the resected temporal lobe in operated patients.
2,
7 –
13 Results from these studies, however, are often contradictory and conflict with each other. Since various new technologies for morphological and functional brain imaging have come into use, this problem has been challenged by utilization of these technologies.
The present study aimed to identify magnetoencephalographic characteristics of psychosis in TLE patients. Specifically we tested the hypothesis that some particular patterns of magnetoencephalographic spike localization correlate with a history of psychosis. In order to gain deeper insight into the mechanism of generation of psychotic symptoms from the results, the discussion will refer also to previous studies on patients with other neuropsychiatric disorders.
METHODS
Patients
The participants were 57 TLE patients who were examined in our magnetoencephalographic laboratory from April to December 1994, the testing period of magnetoencephalographic examination of our institute. Diagnosis was based on electro-clinical findings of individual patients and was not influenced by the result of the magnetoencephalographic study. All patients gave informed consent to participate in the magnetoencephalographic study, which was provided free of charge, and they did not receive any payment. However, since our institution is a highly specialized center for epilepsy care, some selection bias was expected with this subject population. For example, the participants were likely to have more severe disease or higher economic status. After the testing period, the biases should have become much greater, because magnetoencephalographic study has been provided at a charge and gradually focused on potential surgical candidates.
The patients (26 males and 31 females) ranged in age from 14 to 46 years (mean=27 years). The average duration of illness was 16 years. Sixteen of the 57 patients had a history of either chronic or episodic psychosis. In this study, the criteria of psychosis were persistent delusion or auditory hallucination of psychotic nature (voices commenting on or talking to the patient), irrespective of the duration, as distinct from seizure-related confusional states. The ratio of having a history of psychosis in our study group was quite high compared to the previous studies, probably because all our patients had severe and intractable epilepsy and we included patients with only one episode of psychosis if it was definite.
The patients with psychosis (n=16) ranged in age from 20 to 46 years (mean=29), and the mean duration of the illness (epilepsy) was 19 years. Eight of the 16 patients had chronic psychosis, and the remaining eight had episodic psychosis. Ages of the patients in both groups ranged from 20 to 46 years old, although the mean ages differed slightly (30 years old in the chronic group and 29 years old in the episodic group). The duration of illness was 20 years in the chronic group and 19 years in the episodic group. Seven of the patients with psychosis were male and nine were female, with eight out of nine female patients belonging to the episodic group.
Forty-one of the 57 patients were operated on within 5 years of the magnetoencephalographic study. The epileptogenic lesions were identified histopathologically as mesial temporal sclerosis in 28 patients and cortical dysplasia in five patients, while no pathology was detected in the resected temporal lobe of seven patients. The remaining patient had a parietal tumor and underwent lesionectomy. MRI findings of the 16 patients who were not operated on revealed mesial temporal sclerosis in eight patients, ganglioglioma in the temporal lobe in one patient, atrophy of the temporal lobe only in two patients, and no abnormalities in five patients.
Magnetoencephalographic Measurements
Magnetoencephalographic measurements were performed using MSI (Biomagnetic Technologies Inc., San Diego, Calif.) which is a dual sensor system containing 37 channels of first order gradiometer with a baseline of 3 cm in each sensor. The sensors were positioned symmetrically on bilateral temporal regions of the patients. Scalp EEG was simultaneously recorded to facilitate detection of epileptiform discharges. Magnetoencephalography was recorded as epochs, each of which consisted of a 6-second segment including 5 seconds before and 1 second after the trigger was activated by pressing a button manually. The sampling rate was 200 Hz. Each recording session took 1.5–2 hours including the time needed to place the EEG scalp electrodes. After filtering all magnetoencephalographic epochs by a 3–30 Hz digital band-pass filter, equivalent current dipoles of the magnetic spikes (spike-dipoles) were calculated off-line by the software supplied with the machine and superimposed on MR images. Superimposition was done by fitting three-dimensional dotted images of each patient’s head, pivoted on five spatial points marked during the recordings, namely, nasion, inion, Cz point and preauricular points on both sides.
“Clustering” of spike-dipoles was defined as a concentration of more than 10 dipoles within a volume of a 3 cm cube. Then spike-dipole clusters were classified according to anatomical localization and orientation of the dipoles. Dipoles localized at places distant from the clusters were neglected in subsequent analyses.
Classification of Spike-Dipoles
In a preliminary analysis, we initially examined 58 patients and classified them according to the pattern of “clustering” of magnetic spike-dipoles. We set a criterion to exclude patients who showed no magnetic spikes or no “clustering” of spike-dipoles. Eventually only one patient was excluded from the analysis. This patient never showed any magnetic spike or any spike on scalp EEG. Diagnosis was based on spike activity detected only by sphenoidal electrodes. This patient had no history of psychosis.
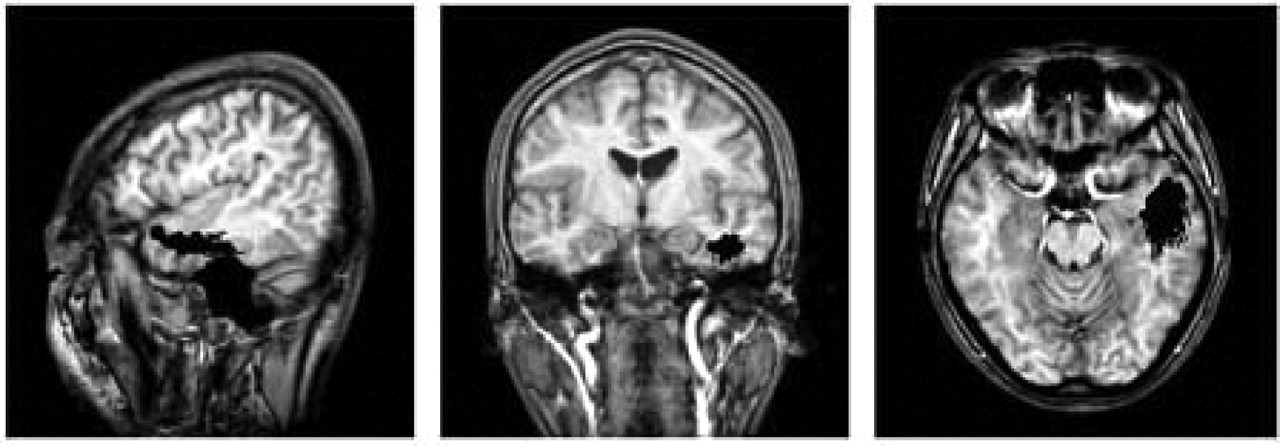
We found two major patterns of spike-dipole “clustering” in the 57 patients analyzed. When clustering was localized on the lower part of the temporal lobe showing an anteroposterior orientation (
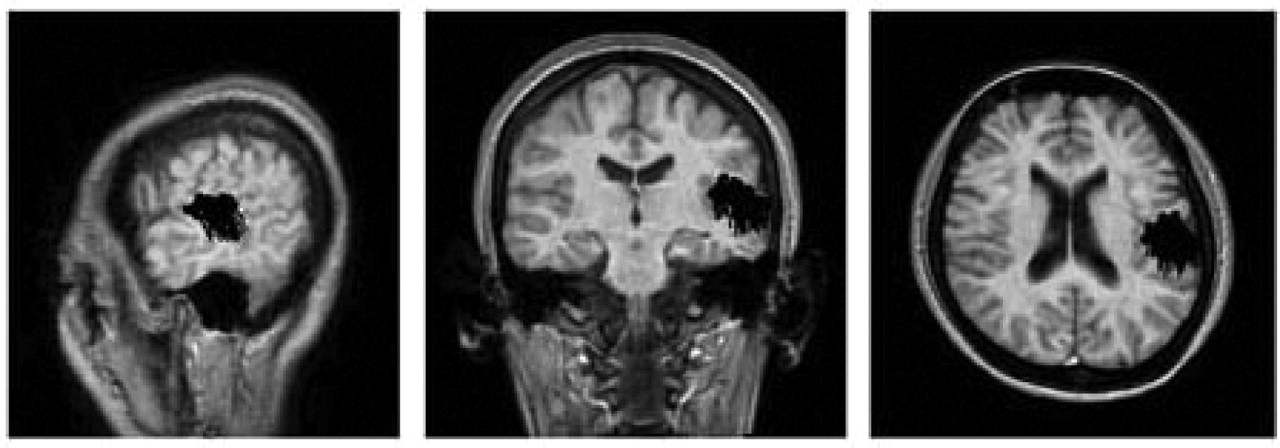
Figure 1 ), we designated this pattern the “inferotemporal-horizontal (IH) type.” When clustering was localized on the upper part of the temporal lobe showing a superoinferior orientation (
Figure 2 ), we designated this pattern the “superotemporal-vertical (SV) type.”
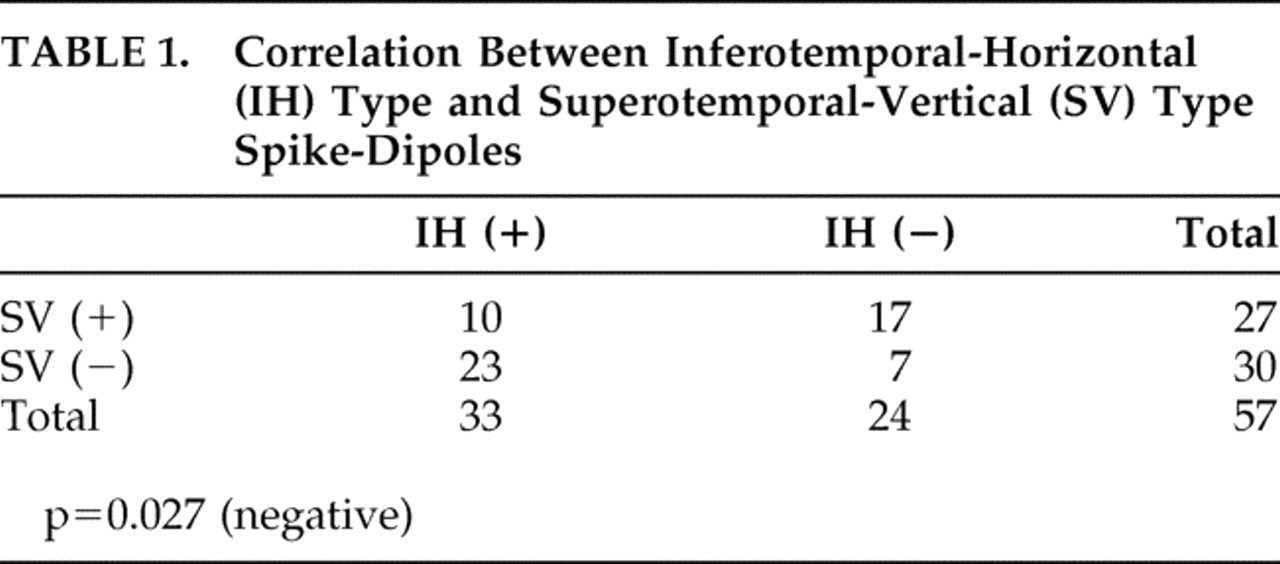
Of the 57 patients showing spike-dipole clusters, 33 had IH type spike-dipoles and 27 had SV type. Among them, 10 patients showed both types, ipsilaterally in eight and contralaterally in two. Three patients had bilateral SV type, and one had bilateral IH type. None had more than two spike-dipole clusters. Only seven patients showed spike-dipole clusters that do not belong to either IH type or SV type. Thus 88% of the patients had IH type and/or SV type spike-dipoles, and Fisher’s exact test showed that the two types of spike-dipoles are significantly exclusive of each other (
Table 1 ).
Having clarified the major patterns of spike-dipoles in all the patients analyzed as described above, we proceeded to examine the relationship between the type of spike-dipoles and psychosis. Our hypothesis was that psychosis in temporal lobe epilepsy is characterized by one or some specific patterns of spike-dipole distribution. In subsequent studies, we investigated the correlation of psychosis with the two patterns, IH and SV types, or four patterns when each was subdivided into left and right.
Although our classification of spike-dipoles is original and different from those of other investigators, it is virtually a simplified version of Ebersole’s classification.
14 Our IH type corresponds to Ebersole’s “anterior temporal A-P horizontal” and our SV type to “anterior temporal vertical tangential” and “posterior temporal vertical tangential” together.
It is noteworthy that whereas magnetoencephalographic spike localization is reliable at a level of several millimeters in cases with spike activities on the convexity of the cerebral cortex, it is not the case in TLE, because of the complex process of propagation of temporal discharges. While the spike-dipoles produced by the method of single dipole fit can be considered to represent the net intracellular current constituting the spike activities in simple cases, spike-dipoles from temporal discharges apparently cannot be considered as such, because they move and rotate in the course of time for each discharge. However, there are apparently few patterns of movement and rotation. That is why the “pattern” of distribution instead of “localization” of spike-dipoles is used in this study and other studies on TLE.
Statistical Analyses
First, the correlation between laterality of magnetoencephalographic foci and a history of psychosis was analyzed. Forty-four subjects were included in this analysis, because seven patients not showing either the IH or SV type spike-dipole and six showing bilateral magnetoencephalographic foci were excluded in order to clarify the effect of unilateral IH or SV type spike-dipole.
Then the correlation of a history of psychosis versus each of two types of spike-dipole, and versus each of four types when IH and SV types were subdivided into left and right, was analyzed. The subjects of the latter analysis comprised 44 patients for the same reason as above.
Next, the correlation between a history of psychosis and coexistence of plural (actually two out of the four) types of spike-dipole or bilateral magnetic spikes was analyzed. The subjects of this analysis comprised 50 patients, because seven patients who had spike-dipoles other than the four types were excluded in order not to confuse the effect of plurality with the effect of a special type of spike-dipole.
The correlation between four types of spike-dipoles and three types of aura (autonomic, elementary auditory and psychic seizures) has been demonstrated in our previous study (submitted for publication). In this study, we examined the correlation between three types of aura and a history of psychosis. The subjects of this analysis comprised 55 patients, because two patients who had auras not classified under the three types were excluded, since the number is too small to be analyzed statistically. These patients had olfactory and/or gustatory seizures.
Additionally, the correlation between the presence of mesial temporal sclerosis and IH type, SV type or psychosis was analyzed on the 57 patients. All correlations were analyzed using Fisher’s exact test.
RESULTS
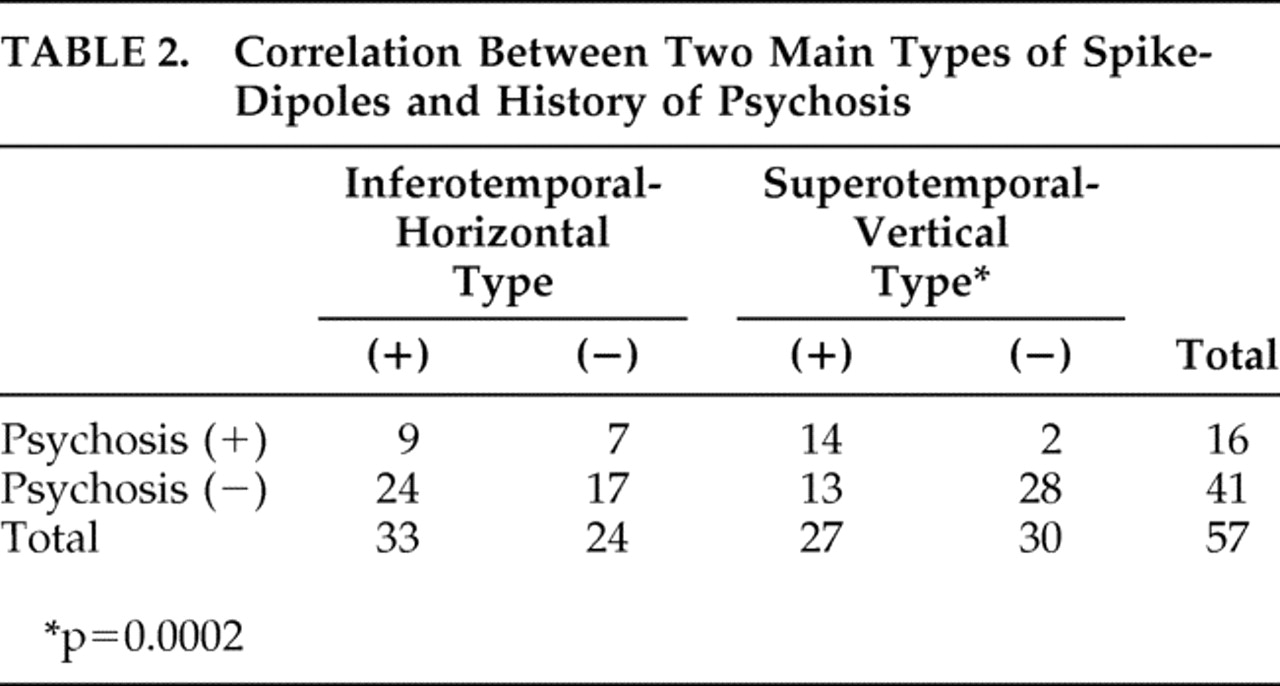
Laterality of magnetoencephalographic foci did not correlate with a history of psychosis (left:right =7:5 in 12 patients with psychosis). No correlation was observed between psychosis and IH type spike-dipoles regardless of laterality, whereas a strong correlation was found between psychosis and SV type (p=0.0002,
Table 2 ).
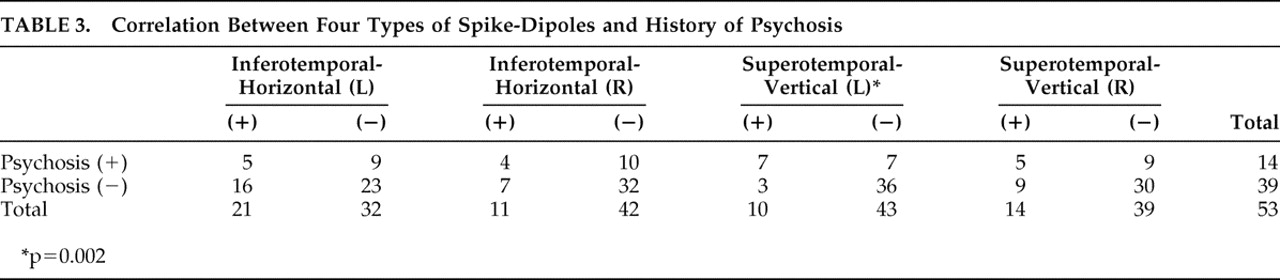
Of four types of spike-dipoles (left and right IH and SV types), only the left SV type showed a highly significant correlation with psychosis (p=0.002,
Table 3 ).
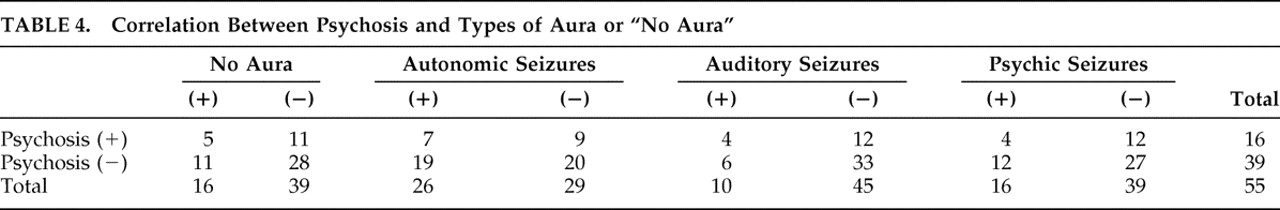
A history of psychosis also correlated with the coexistence of plural types of spike-dipoles (p=0.001). Bilateral magnetic spikes also showed a weak correlation with psychosis (p=0.046). No correlation was found between psychosis and the presence or absence of aura for all three types of aura (
Table 4 ).
A highly significant correlation was observed between IH type and mesial temporal sclerosis (p=0.006), but no correlation was found between SV type and mesial temporal sclerosis. No correlation was found between the existence of mesial temporal sclerosis and psychosis.
DISCUSSION
Episodic and Chronic Psychoses in TLE Patients
Our subjects with psychosis comprised patients with acute or episodic and chronic psychoses. We did not further subgroup these patients but analyzed them as one group so as to obtain a large enough number of patients for statistical analyses. The mean age was slightly higher and the duration of illness slightly longer in the chronic group, although there were no significant differences.
The distinction between episodic psychosis (such as postictal psychosis) and chronic (so-called schizophrenia-like) psychosis in TLE patients has recently been emphasized, apparently due to the increased attention to postictal psychosis.
15 –
18 However, this distinction may not be as important as once believed. Some researchers investigating the differences and commonalities between TLE patients with postictal psychosis and those with chronic interictal psychosis suggest that postictal psychosis has a definite tendency to develop into chronic interictal psychosis during the clinical course.
17,
19 Therefore, combining the episodic and chronic groups into one “psychotic” group is justified from the standpoint of searching for the most relevant regions of the brain involved in the generation of psychotic symptoms.
Laterality Effect on Epileptic Psychosis
Laterality effect on psychiatric symptoms in patients with TLE is one of the most intriguing and also long disputed topics. Although Flor-Henry’s
20 well-known suggestion that schizophrenia or hallucinatory-delusional symptoms are related to the left temporal focus while affective symptoms to the right seems to harmonize with the currently well established lateralization of emotional functions to the right hemisphere, subsequent studies on psychoses in TLE patients verified only left lateralization of schizophrenia symptoms
8,
21 or no lateralization of both symptoms. A consensus on this topic has not been arrived at, because the methodologies of the studies are different and every study has its own limitations.
Our method of typing interictal magnetic spikes also has obvious limitations. First of all, interictal magnetic spikes are not necessarily the landmark of primary epileptogenic foci. Our statistical analysis on the laterality of magnetoencephalographic foci irrespective of type resulted in no significant lateralization. However, when subdivided into IH and SV types, left SV type showed a strong correlation with a history of psychosis. The strong association between IH type spike-dipoles and mesial temporal sclerosis which we have demonstrated suggests an association between IH type and mesial temporal dysfunction, while SV type should, by simple interpretation of spike localization, be related to dysfunction of neocortex around the supratemporal plane. Therefore, our classification of TLE patients by the two types of spike-dipoles and their laterality provides some clues to the relationship between dysfunction of the mesial and lateral portions of the temporal lobes and the generation of psychosis.
Left-sided laterality of psychosis in TLE and also schizophrenia has been supported by studies using new imaging technologies. Conlon et al.
22 reported in 1990 that TLE patients with hallucinations showed significantly high MRI T1 value in the left temporal lobe, although all TLE patients with schizophrenia symptoms did not. Since then, as MRI has become widely used in psychiatric practice, many studies have reported some morphological abnormalities, occasionally correlating with functional abnormalities, of the left temporal lobe in schizophrenia patients.
23 –
28 These reports seem concordant with our results of left-sided laterality of psychosis in TLE patients.
Significance of Bilateral Interictal Spikes
On the other hand, some investigators have suggested that bilateral interictal spikes are indicative of psychosis in TLE patients.
17,
29 This contention does not necessarily mean that bilateral epileptogenic foci or secondary epileptogenesis is essential for the generation of psychosis, but implies that psychosis tends to accompany epileptic involvement of a larger region of the brain. Our finding of a positive correlation between plural types of spike-dipoles and a history of psychosis is concordant with the above contention, because coexistence of plural types of spike-dipoles indicates multiple irritative zones, and consequently more extensive cortical involvement in the epileptic process. Regarding bilaterality of interictal spikes, our result also seems to support the contention, although statistical significance was barely reached, probably because of the small number (only six) of patients showing bilateral interictal spikes.
Mesial or Lateral Dysfunction of the Temporal Lobe
In connection with schizophrenia, the reports that suggest abnormalities in both the left hippocampus
23 and the left temporal neocortex, especially posterior superior temporal gyrus or planum temporale
24 –
29 in schizophrenia patients are relevant to the present study, because our classification of spike-dipoles into IH and SV types relates to the division of temporal lobe pathology or dysfunction into mesial or hippocampal and lateral or neocortical locations.
Using sphenoidal electrode recordings, Kristensen and Sindrup
10 suggested that psychosis was related to epileptic foci localized in mesial structures rather than lateral cortices of temporal lobes.
From pathological study of resected temporal lobes, Taylor
8 suggested a stronger association of psychosis with neocortical pathologies (“alien tissue” lesions) than mesial temporal sclerosis. However, reexamining the same series of the subjects, Roberts et al.
31 concluded that rather than neocortical pathologies such as cortical dysplasia, pathologies involving mesial temporal structures, notably ganglioglioma, are more associated with psychosis. Furthermore, Barr et al.
32 conducted a brain morphometric comparison of patients with first-episode schizophrenia, patients with TLE and healthy comparison subjects and reported marked reduction of left hippocampal volume in first-episode schizophrenia patients comparable only to left TLE patients. Their result strongly suggests the crucial role of left hippocampus in the generation of schizophrenia symptoms. However, it should be noted that volume reduction of the hippocampus does not necessarily indicate mesial temporal sclerosis, and some other reports have suggested that a history of febrile convulsion and existence of mesial temporal sclerosis are less or even negatively associated with psychosis in TLE patients.
8,
17We found no correlation between psychosis and mesial temporal sclerosis in our subjects and also no correlation between psychosis and IH type spike-dipoles. The result that IH type is strongly associated with mesial temporal sclerosis appears to argue against the significance of mesial temporal sclerosis in the development of psychosis in TLE patients.
Magnetoencephalographic Studies on Patients with Other Neuropsychiatric Disorders: Convergence of Evidence of Abnormal Activities Within the Sylvian Fissure
Although magnetoencephalographic findings in patients with neuropsychiatric disorders are scarcely reported, some of them seem to support our results.
Reite et al.
33 suggested that the location of the generator of the later component of auditory magnetic field differed in the left hemisphere of schizophrenia patients. Our interpretation of their result is that some alterations in function and/or structure of temporal lobes are present in schizophrenia patients.
Canive et al.
34 reported that a subgroup of schizophrenia patients showed abnormal slow activities on magnetoencephalography, which were inhibited by antipsychotic medication. In two patients, these slow activities were localized on the superior temporal plane by dipole fitting, which agree with our results of spike localization.
Ishii et al.
35 reported a patient with schizophrenia who showed theta range rhythmic activity in the left temporal region on magnetoencephalography, corresponding to onset of auditory hallucination in time. They used the method of synthetic aperture magnetometry because the generator of the abnormal activity was supposed to be considerably extensive over the cortex and single dipole fitting was inadequate for its localization.
It is also interesting that patients with autistic spectrum disorder show magnetic spike-dipoles around the Sylvian fissure,
36 virtually identical to our SV type, because autistic disorder and schizophrenia psychosis are partially similar in symptomatology and supposed to be somehow related in etiology. It should be noted that if spike generators exist deep within the Sylvian fissure, regardless of frontal, parietal, or temporal operculum, these spikes will elude detection by scalp EEG. In contrast, magnetoencephalography can detect spike activities in considerably deep part of the cortex within the fissure, as far as the originating current is tangential to the scalp, or vertical to the fissure.
37 This may be a reason why scalp EEG frequently fails to detect spike activities on the temporal region in autistic patients. Moreover, the elusiveness of deep Sylvian discharges is also observed in EEG recordings using subdural electrodes, because usually the electrodes are not inserted into the Sylvian fissure but placed striding over it. In patients with deep Sylvian foci, therefore, magnetoencephalography is more powerful for spike detection than subdural electrodes.
Magnetoencephalographic studies on patients with Landau-Kleffner syndrome or acquired epileptiform aphasia are also worth mentioning. Based on the pathophysiological hypothesis that verbal auditory agnosia is caused by epileptic activities around the receptive speech area, spike-dipoles would be expected to be localized on the left posterior perisylvian region.
38 According to Sobel et al.,
39 however, the localization of spike-dipoles is more variable and often bilateral, although spikes on the left posterior perisylvian region are observed in the majority of the cases, in which case the pattern of spike-dipole distribution is similar to our SV type. Sobel et al. suggested that the heterogeneity of spike-dipole localization could be explained by inclusion of epileptic patients with not only aphasic but also autistic or other types of regression in their study. In contrast, Lewine et al.
36 suggested that a subtype of autistic spectrum disorder may be caused by epileptic activities deeply hidden within the Sylvian fissure.
Gibbs
1 in 1951 described the Sylvian fissure as “one of the chief boundaries between neurology and psychiatry” because EEG abnormality in relation to psychiatric disturbance is almost exclusively found on the temporal region. At around the same time, Penfield and Jasper
40 also wrote along the same line that “the relationship of epileptic discharge, in temporal cortex and in the gray matter that is hidden deep in the Sylvian fissure, to psychotic states deserves exhaustive study.” Half a century later, we have apparently reencountered a similar situation during the exploratory stage of magnetoencephalographic study on neuropsychiatric patients. In this context, we would like to reinterpret Gibbs’ expression as meaning that the Sylvian fissure is one of the major keys to bridge the gap between neurology and psychiatry.