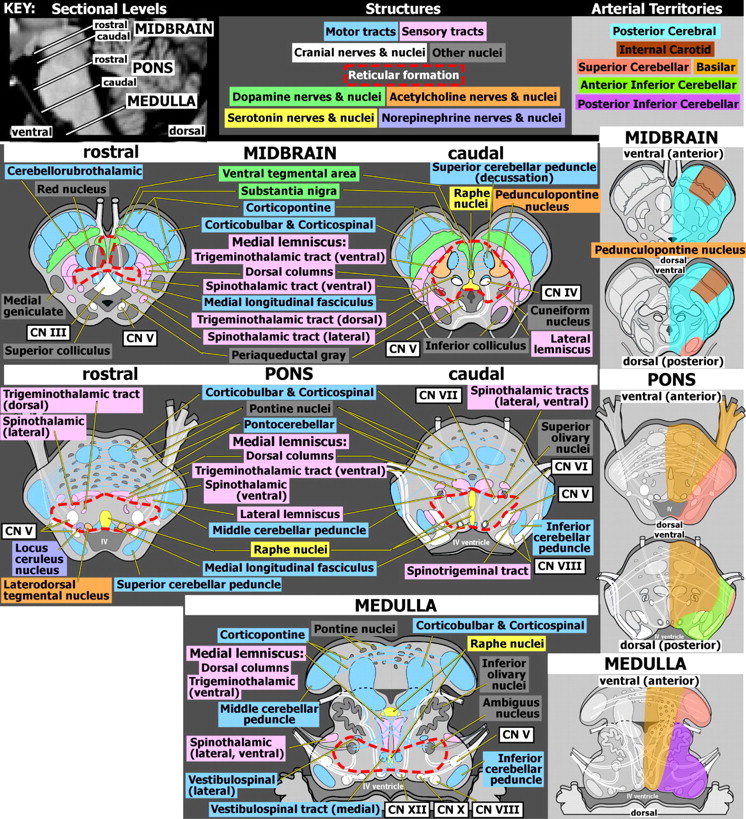
Overview of Anatomy
T he focus in neuropsychiatry is usually on the cortical areas that subserve behavior, cognition, and mood. It is essential to also understand the roles of the brainstem for these functions. Of particular importance, the brainstem is the source for the monoamine (norepinephrine [
Figure 1, purple], dopamine [
Figure 1, green], and serotonin [
Figure 1, yellow]) neurotransmitters that project widely to modulate these circuits. The major subdivisions of the brainstem (from rostral to caudal) are the midbrain, pons, and medulla (
Figure 1, left panel). The brainstem serves as a conduit for many ascending and descending pathways (
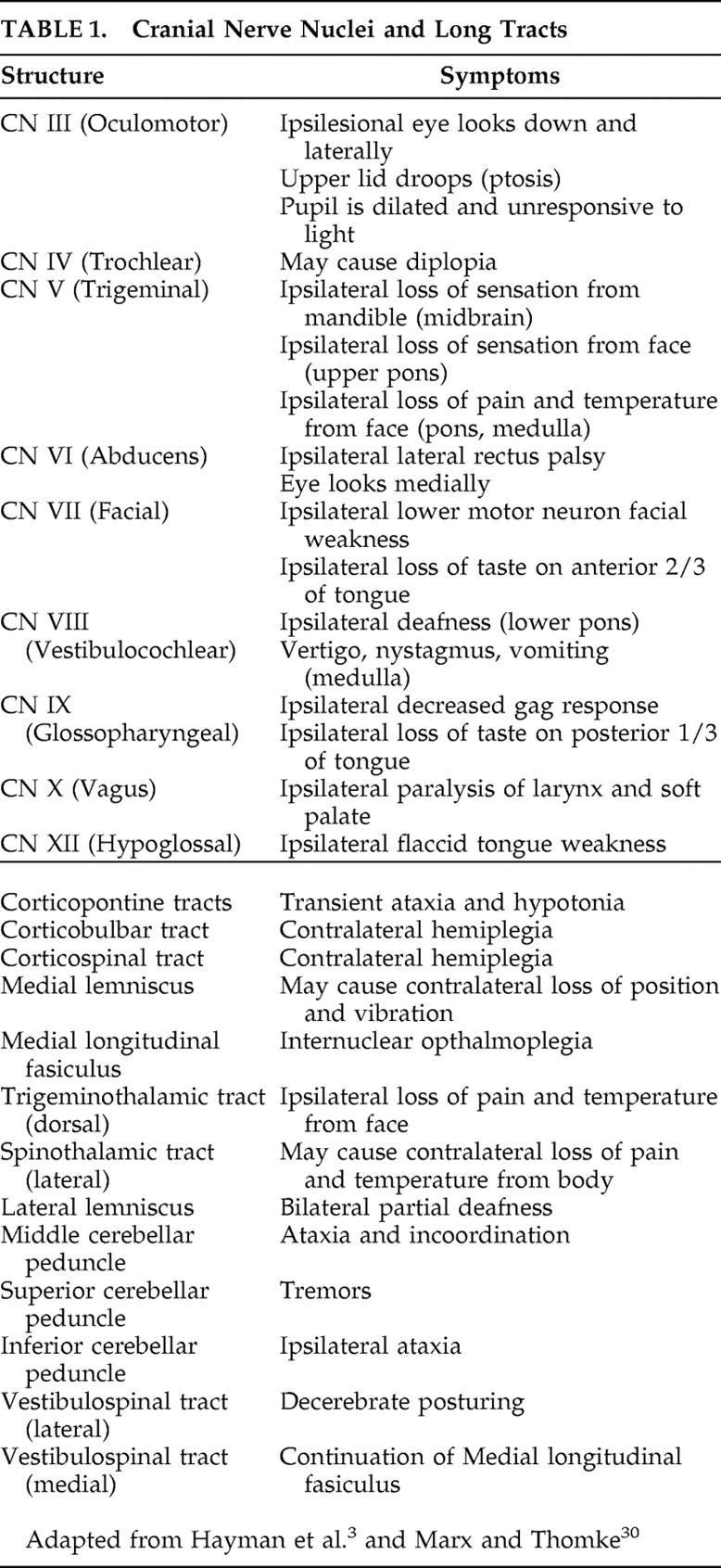
Table 1 ), contains most cranial nerve nuclei (
Figure 1, white, and
Table 1 ), and is important for many key integrative functions. It contains the lower motor neurons for the muscles of the head and does the initial processing of general afferent information concerning the head. The reticular formation forms the central core of the brainstem (
Figure 1, area approximated with dashed red lines).
1,
2 It participates in a wide range of functions including control of movement, modulation of pain, autonomic reflexes, arousal, and consciousness. The vascular supply to the brainstem is primarily from the posterior cerebral artery and the vertebral-basilar system (
Figure 1, right panel).
3 In general, the small arteries that penetrate and supply the brainstem arise directly from larger arteries.
3 These regions are at high risk for ischemia because there is little or no interconnecting surface network to provide collateral circulation.
The most rostral part of the brainstem is the midbrain. It is characterized by four bumps, the paired superior and inferior colliculi on its dorsal (posterior) surface, and by the large cerebral peduncles (containing the descending corticospinal and corticopontine tracts) on its ventral (anterior) surface. The nuclei for cranial nerves III, IV, and part of V (sensory) are found in the midbrain. The ascending superior cerebellar peduncles cross (decussate) in the caudal midbrain. Fibers enter the red nucleus and also continue on to the thalamus. Other key midbrain structures include the substantia nigra and ventral tegmental area (both dopamine-containing [green]), the pedunculopontine nucleus (acetylcholine-containing [orange]) and the first of the raphe nuclei (serotonin-containing [yellow]).
Caudal to the midbrain is the pons. The nuclei for cranial nerves VI, VII, VIII, and part of V (motor) are found in the pons. Here the corticopontine fibers (blue) terminate in the pontine nuclei (gray). These nuclei give rise to the pontocerebellar fibers that cross the midline to form the middle cerebellar peduncle (blue). This area is particularly vulnerable to injury in malnourished individuals, especially if there has been a rapid correction of electrotype abnormalities.
8 The classic symmetric areas of myelin disruption that characterize central pontine myelinolysis are thought to result from osmotically active factors expelled by the cells within gray matter that are toxic to myelin. White matter adjacent to edematous gray matter (like the crossing pontocerebellar fibers intermingled with the pontine nuclei) is therefore the most exposed. The ascending and descending fiber tracts are compact white matter bundles and much less affected. Lesions are also found in other gray matter regions containing heavily myelinated fibers, such as thalamus, basal ganglia, and cerebellum.
Caudal to the pons is the medulla, containing the nuclei for cranial nerves IX, X, XI, XII and a portion of V. Ascending spinocerebellar tracts form the inferior cerebellar peduncle at this level. The ascending sensory tracts from the body (posterior columns) terminate in the posterior column nuclei (gracilis, cuneatus) in the lower medulla. These nuclei are the origin of the spinothalamic tracts that cross (sensory decussation) in the lower medulla and ascend to form the medial lemniscus (pink).
Neuropsychological Deficits
The common perception has long been that brainstem injury results primarily in motor and cranial nerve deficits. More recent work has focused on the transient and permanent cognitive deficits that can occur in conjunction with brainstem lesions. Individuals have been described as being unable to return to their baseline levels of functioning in daily life activities, even after physical and neurological deficits have resolved.
9 Although the literature is somewhat limited, there have been several case reports and case series examining cognitive functioning in small cohorts of individuals with brainstem insults.
9 –
13 The most frequently reported deficits following isolated brainstem lesions are impaired attention and executive functioning. These have been observed across a variety of tests, including letter fluency and category fluency, the Trail Making test, letter cancellation tests, various sorting tests (Weigl sorting test, Modified Card Sorting Test), the Test of Every Day Attention (visual elevator subtest), and the Stroop Color and Word Test. Impaired naming ability also occurs relatively frequently in individuals with brainstem injury. Memory impairment has been reported much less commonly, and sensory-perceptual deficits are not typically reported. Interestingly, one study noted declines in general intellectual ability in approximately 50% of children following resection of low-grade brainstem tumors.
14Injury to the ventral pons can result in locked-in syndrome, characterized by paralysis of all four limbs and mutism (paralytic).
15 Using testing based on eye-coded (yes/no) responding, several studies have examined cognitive abilities in individuals with this condition. A self-report survey study of patients (N=44) with chronic locked-in syndrome indicated that six patients (14%) reported impaired attention and 19% reported memory difficulties.
16 A recent study utilized neuropsychological testing in patients (N=9) with chronic locked-in syndrome due to isolated brainstem injury.
17 While cognitive functioning was generally preserved in the group, individual-specific deficits included mental calculation and problem solving, auditory and visual recognition, and receptive language. In contrast, a case report of two patients with chronic locked-in syndrome found no cognitive deficits on neuropsychological assessment.
18 Similarly, a case series (N=10) reported that locked-in patients can recover intact cognitive levels in cases of pure brainstem lesions.
19 Although the authors of that study concluded that injuries to additional areas of the brain were most likely responsible for reported deficits in this population, other studies (as noted above) have reported deficits in patients with isolated brainstem insults.
In summary, the literature indicates a variety of circumscribed cognitive deficits may occur after brainstem insults, and these do not always completely resolve. The profile of deficits seen in well-studied individuals implicates disruption of the frontal-subcortical system, with specific impact on regions involved in attentional and executive functioning. The brain areas that are primarily associated with the performance of executive functions are the prefrontal and the anterior cingulate cortices.
20,
21 These areas are reciprocally interconnected with the brainstem.
22,
23 The findings of pervasive attentional and executive impairment, with naming and receptive language deficits often present, serve to remind us that specific cognitive abilities can be disrupted by injury to areas remote from the cortical circuitry that is primarily associated with these domains. The implications of these cognitive deficits are important. Several studies examining functional outcome in rehabilitation following stroke have shown that cognition, particularly attention and executive abilities such as abstract thinking, judgment, problem solving, short-term verbal attention and memory, and comprehension can play an important role in determining length of hospital stay and in predicting functional status at time of discharge.
24 –
28 Higher-order cognitive skills such as awareness, accurate understanding of one’s impairments, and the capacity to learn and generalize functional skills also impact successful rehabilitation. Unfortunately, individuals who demonstrate significant physical improvement may not make concomitant gains in cognition and therefore may leave rehabilitation with less functional independence and a greater need for follow-up services.
Clinical Brainstem Syndromes
The clinician needs to be familiar with how neuroanatomical functional units cluster in the brainstem. These can be summarized as cranial nerve nuclei; pigmented nuclei (red nucleus, substantia nigra [“black nucleus”], and locus ceruleus [“blue spot”]); and tracts (e.g., corticospinal, corticopontine, spinothalamic, spinocerebellar) that pass through. When any two of these three categories show impairment simultaneously, particularly when there are alternating signs, the lesion is likely to be within the brainstem. Thus, if the patient has cranial nerve deficits (
Table 1 ) accompanied by parkinsonism or cranial nerve deficits and a crossed corticospinal neurological sign, the first place to localize the lesion would be the brainstem. Lesion location can be approximated (
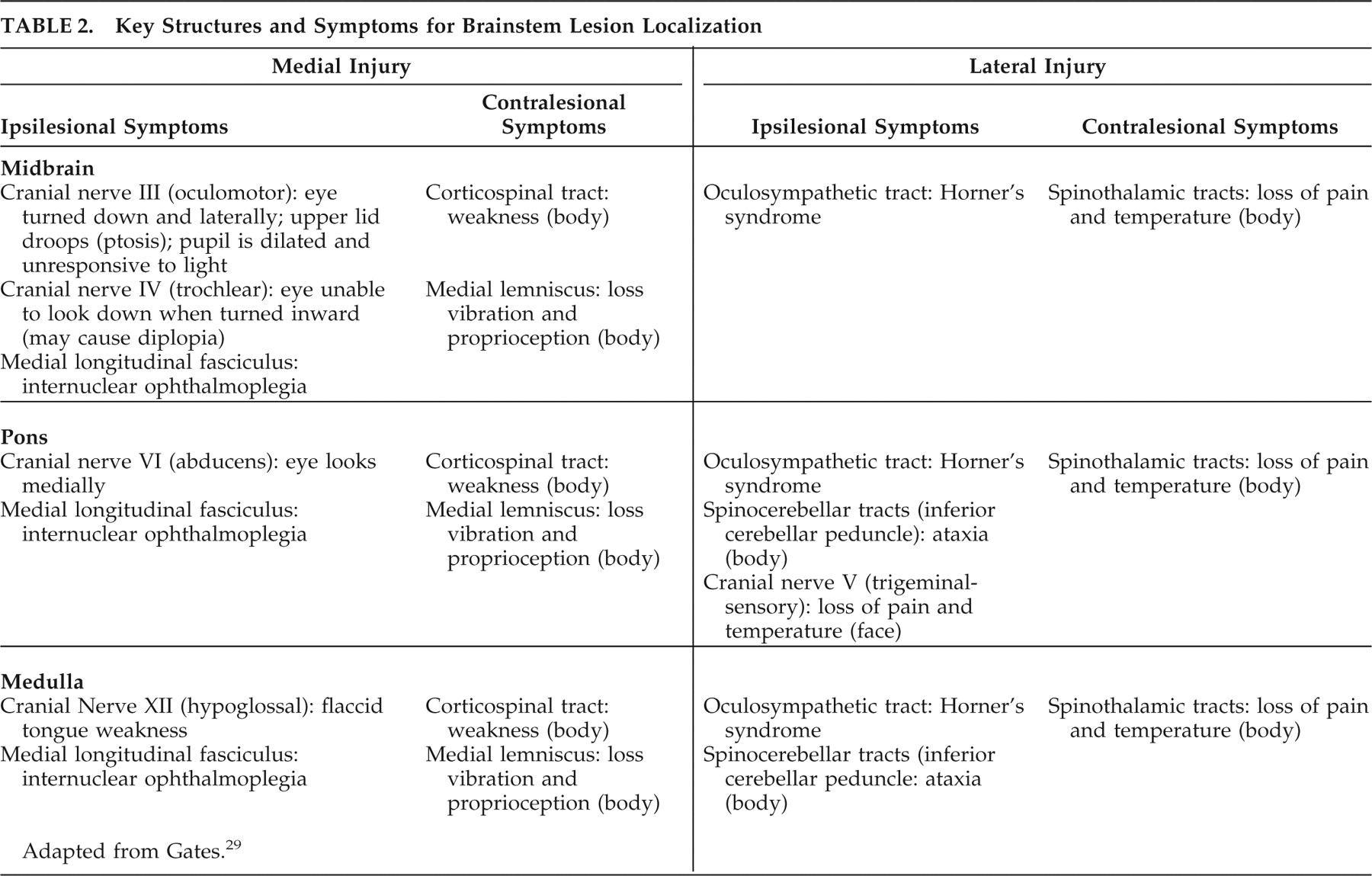
Table 2 ) by combining cranial nerve-related symptoms (which provide rostral-caudal localization) and long tract-related symptoms (which provide medial-lateral localization).
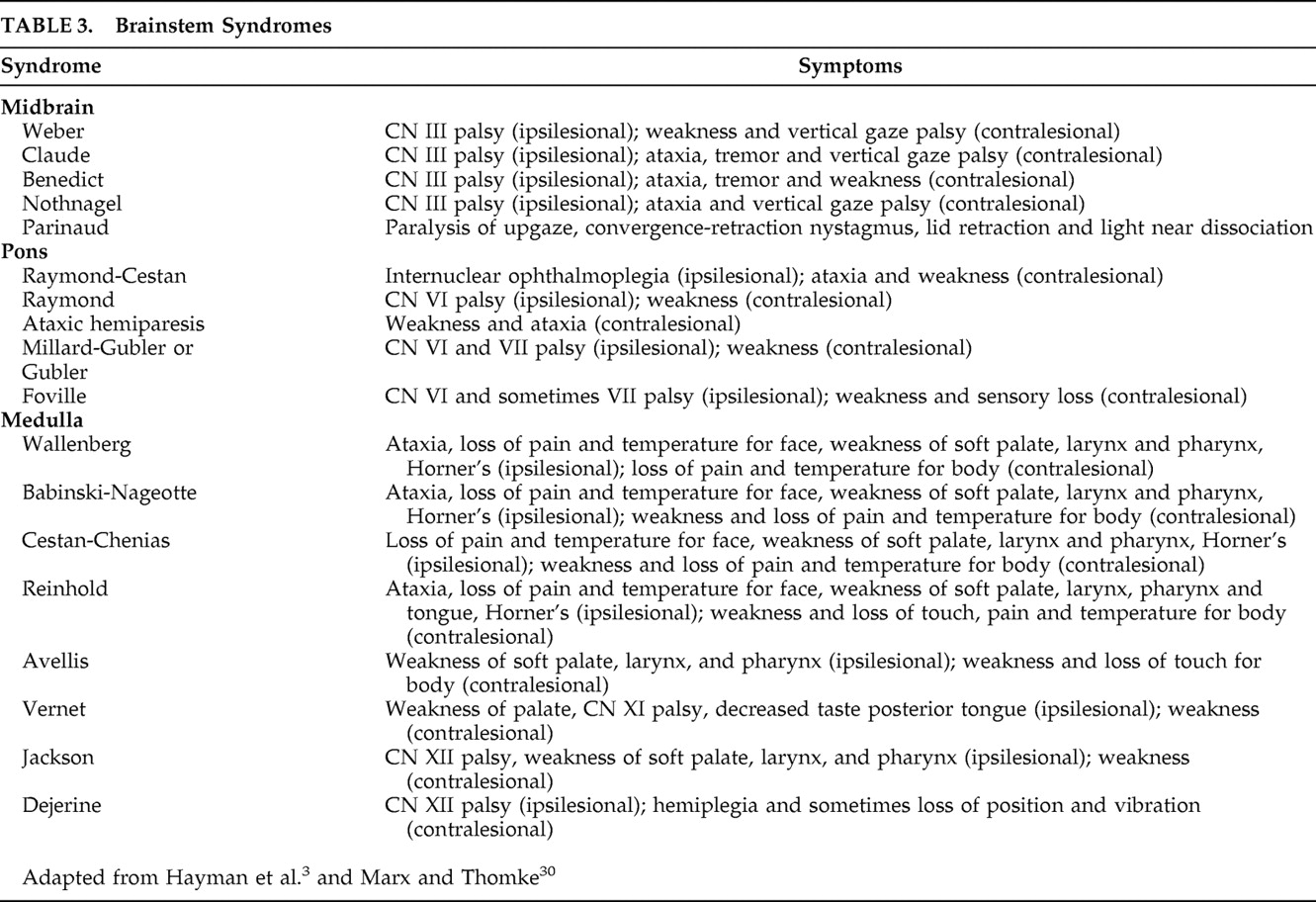
29 There are multiple named brainstem syndromes, most known by eponym (
Table 3 ).
3,
30 It has been noted that many of these are seldom encountered in clinical practice. The combination of symptoms is the critical factor. Thus, the Weber, Claude, Benedict, Nothnagel, and Parinaud syndromes, all resulting from midbrain lesions, have oculomotor nerve palsy (CN III) in common. This generally causes diplopia on lateral gaze, but there could also be disconjugate vertical gaze. Use of the Maddox Rod and a penlight can help the clinician disentangle the direction in which the eyes are disconjugate.
31 The Millard-Gubler syndrome localizes to the pons with its facial palsy (CN VII) and sometimes lateral rectus palsy (CN VI, another way to achieve diplopia). Avellis, Jackson, and Wallenberg syndromes arise from medullary lesions that cause oropharyngeal deficits (CN IX-XII).
32,
33The differential diagnosis for brainstem syndromes can be fairly easy to remember. These are typically focal lesions due to stroke, neoplasm, or multiple sclerosis. Less common etiologies for brainstem syndromes would include infectious diseases (especially some meningitides that center on the base of the brain like tuberculosis), vascular malformation, traumatic brain injury, hyponatremia causing a central pontine myelinolysis, and the neurodegenerative movement disorders progressive supranuclear palsy (PSP) and multisystem atrophy. Although not commonly considered a brainstem syndrome, Parkinson’s disease almost always extends beyond the cardinal signs of parkinsonism (resting tremor, postural instability, akinesia, gait changes) associated with degeneration of the substantia nigra.
34,
35 Depression is highly prevalent among patients with Parkinson’s disease, at times manifesting as a prodrome and certainly complicating disease management.
36,
37 Antidepressant effects of
L -dopa and lack of correlation of severities of depressive symptoms with motor disability imply that depression in the Parkinson’s disease context results from the dopaminergic deficit. Autonomic system impairments also impact heavily on Parkinson’s disease quality of life, possibly related to vagal neuropathy (lower pons).
38 Parkinson’s disease occurs in one of every 272 people in the population, whereas multiple sclerosis occurs in one of every 700.
While most clinicians are familiar with the cardinal signs of parkinsonism as described above, PSP is less frequently seen, with a prevalence of 1 to 6.5 per 100,000.
39 Most patients with PSP have an onset in the 7th decade of life. Reported male to female ratios range from 1:1 to 4:6.
40 Twenty percent of patients with PSP present with the behavioral criteria for frontotemporal dementia: insidious onset with gradual progression, early decline in social interpersonal conduct, early impairment in regulation of personal conduct, early emotional blunting, and early loss of insight.
41 The other 80% present with the motoric signs of PSP, most frequently referred to as absence of vertical gaze. Clinicians may or may not find it helpful to consider PSP as manifesting with a “leonine facies.” Some prefer to describe it as a surprised look, but this may be seen as an angry stare by others. This feature is not included in the diagnostic criteria for PSP. Instead, multiple unexplained falls and impairment of vertical gaze are required for probable PSP.
42 When examining for vertical oculomotor movements, the important features of the vertical gaze are the latency and speed of the saccadic movement.
43 Abnormality can also be detected if the patient needs to make corrections when they move the gaze from one target to a second target in a vertical direction. Patients with PSP may demonstrate increased latency of saccades, slower speed, or “past pointing.” In contrast, the patient who has normal changes to extraocular movements due to aging will have some decreased range of motion on vertical gaze, but the saccades should be intact. In addition, there is some abnormality of horizontal gaze in PSP, in that the square wave jerk can reflect decreased fixation. This is thought to be due to dysfunction of burst cells in the brainstem reticular formation.
43 Patients with PSP may show the atrophy of the midbrain in what is called a “hummingbird” or “penguin” sign.
44 A recent study by Borroni et al.
45 reports a correlation between an isoform of cerebral spinal fluid tau levels and not only the diagnosis of PSP but also the degree of atrophy in the brainstem.
Cranial nerve deficits can be easy to recognize on elemental neurological examination, but lesions to substantia nigra, locus ceruleus or dorsal raphe may be more insidious in their manifestations. As mentioned above, parkinsonism would be a clue that the substantia nigra has been affected. There is also evidence to support attention deficit/hyperactivity disorder arising from a lesion in the substantia nigra (as well as from norepinephrine disturbance, see below).
46 Deficits in serotonin production by the dorsal raphe have been associated with depression, suicidality, psychosis, and frontotemporal dementia.
47 –
49 Both serotonin and acetylcholine are important to the function of the reticular activating system. Therefore one might anticipate that sleep disturbances and delirium could be related to a brainstem lesion involving the dorsal raphe.
50 A lesion in the locus ceruleus will reduce the production of norepinephrine. This is associated with depressive symptoms, attention deficit/hyperactivity disorder, posttraumatic stress disorder, and hypotension.
51 –
54 Apathy has been related to all three of these neurotransmitters. Apathy has been reported after pallido-nigral lesions
55 and in a patient population with neuro-Behçet disease, affecting the brainstem and cranial nerves.
56In conclusion, a working knowledge of the brainstem anatomy and physiology is essential for the assessment of patients with symptoms of cranial nerve deficits, motor, sensory, or cognitive/behavioral changes. Summary charts, color-coded maps, and tables are available for clinicians who may not regularly assess patients with brainstem injury. The inclusion of the brainstem in discussions of the cognitive/emotion/behavior circuits is necessary for a thorough review of brain function.