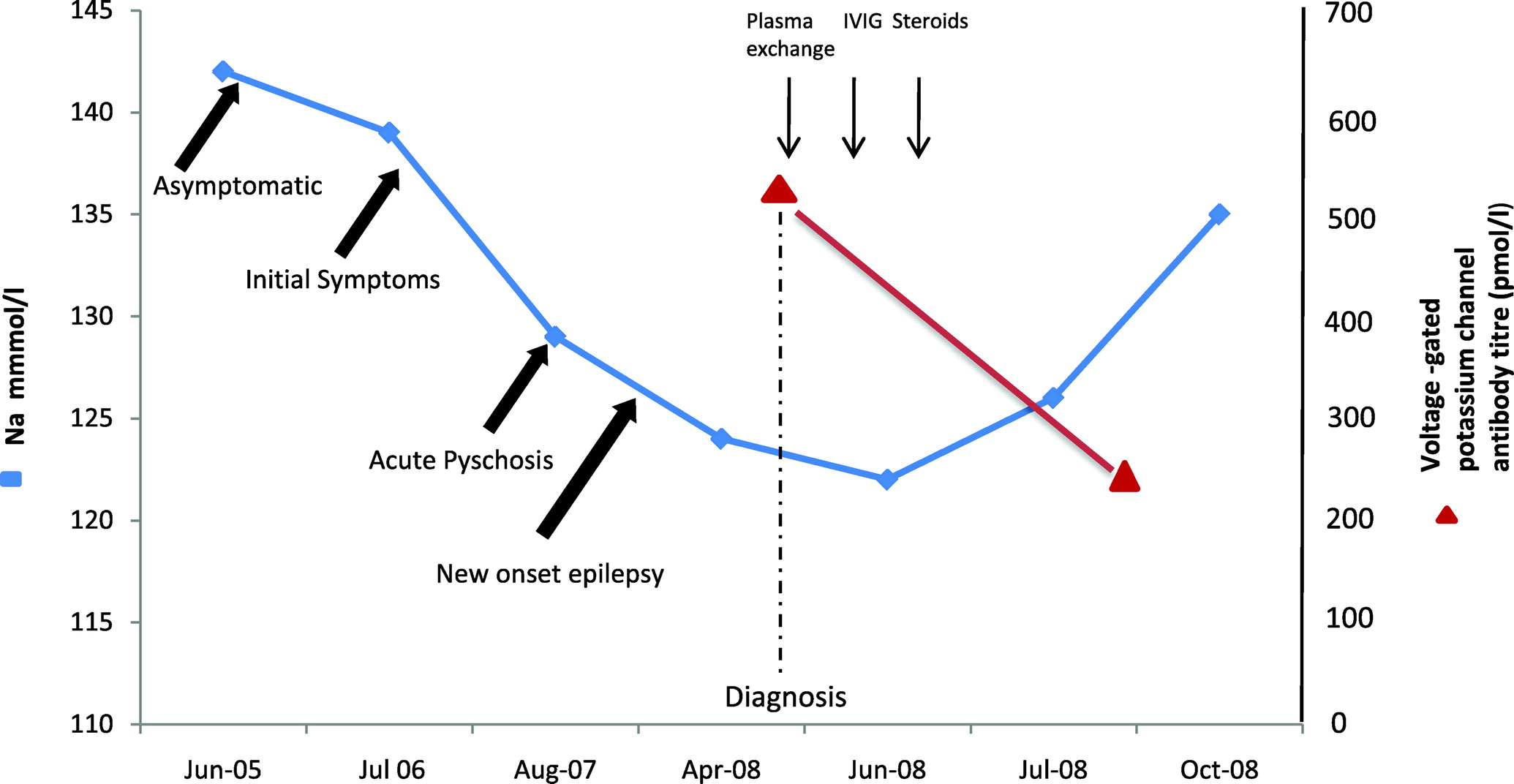
A 58-year-old man was admitted to the hospital in April 2008 with increasing frequency of seizures, confusion, slurred speech, ataxia, and falls. He had a previous history of excess alcohol consumption, depression, and deliberate self-harm. The patient's depressive symptoms began in August 2006 and were associated with episodes of amnesia and confusion. A year later (August 2007) the patient was admitted with an episode of severe self-harm. This was particularly disturbing, as the patient had self-inflicted multiple stab wounds with a knife to his neck, chest, abdomen, and upper limbs. Computed tomography (CT) scan of the chest and abdomen revealed a left pneumothorax, left pleural effusion, and free gas in the peritoneal cavity. Urgent laparotomy showed multiple anterior abdominal wall lacerations but no intra-abdominal organ injury. A chest drain was inserted to drain the left hemo-pneumothorax. Upper limb injuries included multiple right flexor tendon injuries and a deep laceration to the left biceps tendon, all of which required surgical repair. A psychiatric assessment at this stage concluded that the patient was suffering with paranoid delusions and auditory and visual hallucinations; he was subsequently diagnosed with paranoid schizophrenia. He was started on olanzapine, which resulted in some improvement of his psychotic symptoms. Over the next 2 months, his cognitive functioning deteriorated significantly, with progressive amnesia, personality change in the form of aggression, and new-onset epilepsy. Comparison of his previous Mini-Mental State Exam scores showed a rapid decline, from 26/30 to 8/30 in 2 months. His epilepsy worsened, and the seizures became both bizarre and resistant to multiple anticonvulsants. On this admission, blood investigations were all normal, apart from low serum sodium. The hyponatremia (ranging from 122 mmol/liter to 126 mmol/liter) in retrospect had persisted over 10 months (
Figure 1). Plasma and urine osmolality suggested this to be due to the syndrome of inappropriate ADH secretion (SIADH). A brain MRI showed nonspecific areas of high signal. CSF analysis and an EEG were normal. Investigations for neurological infections, malignancy (CT scans of the chest, abdomen, and pelvis, and tumor markers), onco-neuronal, autoimmune, and thyroid antibodies were all negative, but serum voltage-gated, potassium-channel antibodies (VGKC-Abs) were elevated, at 506 pmol/liter (normal range: 0–100 pmol/liter). A diagnosis of limbic encephalitis (LE) was made on the basis of these findings. The patient was treated with plasma exchange, followed by intravenous immunoglobulins and corticosteroids. A repeat VGKC antibody titer 3 months later showed a reduction to 253 pmol/liter, which coincided with improvement in serum sodium levels, as well as improvement in the patient's seizure frequency and aggressive behavior. There was minor improvement in his cognitive functioning, although it is likely that the patient had suffered with autoimmune (VGKC antibody-associated) LE for nearly 2 years, which may have caused permanent neuronal damage irreversible by immunotherapy.