“It’s everywhere—small towns, big towns, in the cities,” said Scott Beamon of the Indiana State Police Department. “A few years ago we came across two or three labs. Last year we had 681. This year, at the rate we’re going, we’ll absolutely blow that record away.”
An epidemic of methamphetamine abuse spreading across the United States from the West Coast to the Midwest and East is overburdening state law-enforcement systems and posing major problems for public health agencies. Substance abuse experts say it makes the need for developing effective treatments for stimulant addiction more important than ever. They are calling for federal law enforcement, prevention, research, and treatment agencies to prepare strategies to address the growing problem.
Over the past 10 years, the production of methamphetamine has passed from a few “biker-gang cookers” to two important new groups, methamphetamine expert Richard Rawson, Ph.D., associate director of UCLA’s Integrated Substance Abuse Programs, told Psychiatric News. He said that creative “kitchen chemists” can now download recipes for making methamphetamine from the Internet to supply their friends and associates; also, organized drug trafficking cartels have begun to manufacture the stimulant. With the addition of these two groups, the availability of methamphetamine is likely to increase as new markets are created.
The expansion is well documented by law enforcement officials. In Iowa illegal labs grew from only two in 1994 to a whopping 803 five years later. In 1999 in Des Moines, 14 percent of people arrested for any crime tested positive for methamphetamine. Last year 80 percent of drug cases under the jurisdiction of the U.S. attorney in Nebraska involved methamphetamine. The National Institute on Drug Abuse reports that in 2001 more than 8,000 clandestine labs were raided nationwide. Recently Michigan state police received a $250,000 federal grant to help beef up seizure of illegal drug labs.
“This is a worrisome trend, indeed,” David McDowell, M.D., medical director of the Substance Treatment and Research Service at Columbia University/New York State Psychiatric Institute, said in an interview. “Now it becomes important for clinicians to learn more about methamphetamine and addiction in general.”
Side Effects Dangerous but Alluring
Because the “high” that methamphetamine gives is intense and can last from eight to 24 hours, it has replaced cocaine, heroin, and marijuana as the drug of choice in many areas. Known on the street as “speed,” “meth,” “ice,” and “crystal,” it can be injected, smoked, snorted, or swallowed.
“The timing and intensity of the ‘rush’ are a result of the release of high levels of dopamine in the brain. Methods that cause methamphetamine to pass into the brain more quickly—smoking or injecting—are more reinforcing and more addicting,” said McDowell.
According to Rawson, neuroimaging studies have shown that methamphetamine appears to damage neurons in ways that are different from, and in some ways more severe than, damage caused by other drugs of abuse. While there are profound changes to the dopamine and serotonin systems, many of the changes appear to be reversible, but only after a prolonged period of abstinence.
Even in small doses, methamphetamine exerts a powerful action on the central nervous system, resulting in increased wakefulness, increased physical activity, decreased appetite, increased respiration, hyperthermia, and euphoria. Over time and with larger doses, these effects may morph into less desirable ones, such as irritability, insomnia, confusion, tremors, convulsions, anxiety, paranoia, and aggressiveness. In some instances, death may occur.
Other well-documented health effects include heart rate and blood pressure elevation that can irreversibly damage blood vessels in the brain and produce strokes, respiratory problems, irregular heartbeat, extreme anorexia, and cardiovascular collapse. Methamphetamine appears to cause reduced levels of dopamine, which can result in symptoms like those of Parkinson’s disease. In addition, abusers are more likely to engage in risky behavior such as sharing needles or practicing unsafe sex, resulting in increased risk of human immunodeficiency virus infections, detrimental effects to the unborn and newborn, as well as social, financial, and psychological problems.
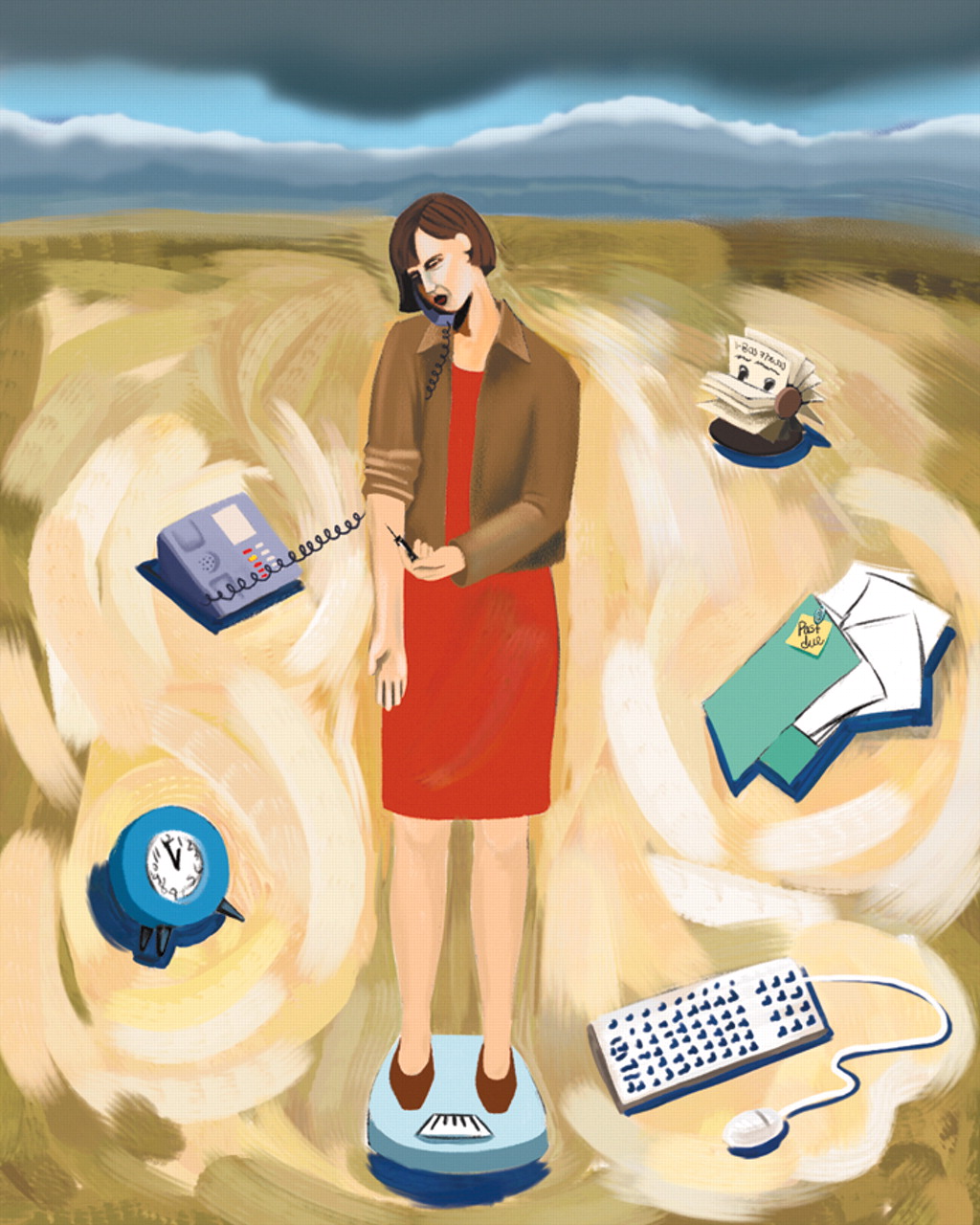
Usefulness of the drug in reducing fatigue and its value in weight reduction are two factors that make it attractive to users, according to Rawson. It is popular among people who need to work long hours in tedious, physically demanding jobs. If they do not inject the drug, many people can take methamphetamine for years before negative consequences begin to occur.
A review of the current understanding of stimulant abuse is found in the third edition of the American Psychiatric Publishing Textbook of Substance Abuse Treatment, due out in spring 2004. In one chapter Thomas R. Kosten, M.D., professor and deputy chief of psychiatry of Yale University School of Medicine, and Mehmet Sofuoglu, M.D., Ph.D., also of Yale, describe how the rewarding effects of stimulants are mediated through the mesocorticolimbic dopamine system and that reinforcing properties of cocaine and methamphetamine are associated with their ability to increase synaptic DA levels. Cocaine increases dopamine by binding to the dopamine transporter and inhibiting its activity, whereas amphetamine increases synaptic dopamine concentrations. Cocaine and methamphetamine also act on norepinephrine and serotonin neurons. All of these sites become important targets for medication development, according to the authors.
Treatment Suggestions
Effective therapeutic pharmacological agents are desperately needed to quell the drug’s alarming symptoms and could help wean patients off stimulants, since many are unaware of or deny their addiction.
“Although a number of potentially therapeutic agents have been studied, at this point we do not have any established pharmacological treatment for these disorders,” Kosten told Psychiatric News.
In addition to methamphetamine users who experience persistent psychosis, Rawson said that treatments for methamphetamine-related problems are particularly critical for pregnant women and women with children, gay and bisexual men, and users involved in the criminal justice system. These populations may have unique issues that require specialized treatment approaches.
An ambitious program of pharmacotherapy development research is being sponsored by the National Institute on Drug Abuse via a network of new clinical trial sites located in geographic areas significantly impacted by methamphetamine use.
The most important component of stimulant treatment involves behavioral therapies. Psychosocial measures, such as contingency management, appear to hold promise, and several studies have found that more patients stayed with these forms of treatment, which can lead to abstinence. They also establish a platform for any pharmacotherapy, and by engaging the patient, they facilitate more long-term changes, including relapse prevention.
Incentives contingent on drug abstinence are a powerful intervention tool for facilitating abstinence in cocaine and methadone-maintained cocaine abusers. There is evidence that methamphetamine-dependent individuals respond similarly. The aim is to decrease behaviors maintained by drug reinforcers and increase behavior maintained by nondrug reinforcers by presenting rewards.
In a 24-week study, cocaine-dependent individuals who received an incentive, such as a $1 lottery ticket for every clean urine sample, showed significantly greater treatment retention and longer duration of continuous abstinence than those not receiving incentives. In a 12-week clinical trial among methadone-maintained cocaine abusers, the contingency group (the subjects whose reward was contingent upon their remaining clean) also achieved significantly longer duration of sustained cocaine abstinence than controls.
In a paper titled “Will the Problem of Methamphetamine Go Away?,” presented last year at the annual meeting of the American Association of Addiction Psychiatry in Amelia Island, Fla., Rawson noted that some believe methamphetamine use is a temporary problem, not a long-term one. Disagreeing, he gave a number of reasons why he believes that significant problems with methamphetamine may persist or even expand (
see box).
What is needed, he said, is for the federal government to devise a long-term plan that will reduce, if not completely eradicate, the problem.
“Recent research on methamphetamine clearly shows that a strategic program of research, prevention, and treatment must be developed, adequately funded, and coordinated with community agencies if we are to minimize the impact of this serious public health problem,” he told Psychiatric News. ▪