For the first time since the State Children's Health Insurance Program (SCHIP) was established in 1997, total national enrollment figures showed a decline during the six-month period that ended December 31, 2003 (see related story on
page 1).
Texas accounted for more than half of the decrease.
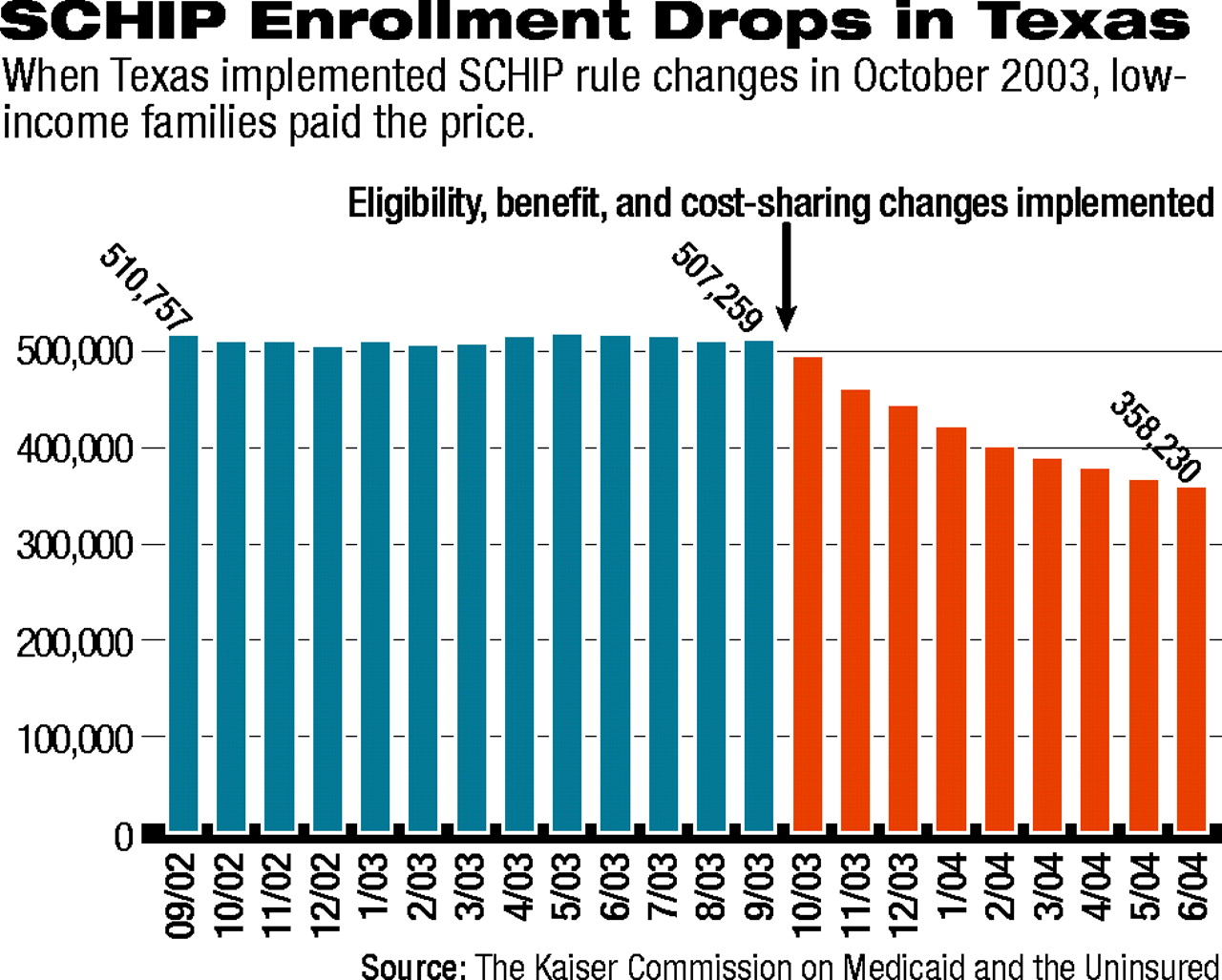
In Texas, enrollment in SCHIP declined by more than 149,000 children (29 percent) since the beginning of FY 2004, which began in July 2003.
The decrease was part of an effort by the Texas legislature to address a budget shortfall of “unprecedented magnitude,” according to a report prepared for the Kaiser Commission on Medicaid and the Uninsured.
Anne Dunkelberg, M.P.A., senior policy analyst with the Center for Public Policy Priorities, wrote in “Children's Medicaid and SCHIP in Texas: Tracking the Impact of Budget Cuts” that the estimated shortfall was between $9.9 billion and $16 billion for FY 2004-05.
Further reductions are projected for Texas by the state's Health and Human Services Commission. That agency projects that SCHIP enrollment in FY 2005 will be reduced 32 percent below the number enrolled in 2003.
Texas made the cuts by tightening eligibility requirements, increasing premiums and cost-sharing, and reducing benefits and payments to providers.
The state eliminated various income deductions so that gross, rather than net, income determines eligibility and added an asset test. Children will be covered only for six months, rather than a year, before parents must reapply. A 90-day waiting period for first-time enrollment has been instituted.
Premium costs have been increased at varying rates for all families above 100 percent of the federal poverty level (FPL). Families between 101 percent and 150 percent now have a $15 monthly charge, which replaces a $15 annual enrollment fee.
Co-pays for office visits have increased for all income levels above 101 percent of FPL.
The state eliminated dental, vision care and eyeglasses, skilled nursing, and tobacco-cessation services.
Dunkelberg told attendees at a briefing on SCHIP and Medicaid that state officials first planned to eliminate all mental health benefits except one psychiatric evaluation and five medication-management visits per coverage period, but that federal officials urged a “more viable mental health benefit.”
The final benefit package has yet to be determined.
As for the impact of these cuts, Dunkelberg wrote that “virtually all the net reduction in SCHIP enrollment has been among children in families with incomes below 150 percent of the FPL.”
The number of children between 101 percent and 150 percent of FPL with SCHIP insurance has dropped by more than one-third since September 2003.
The Institute for Child Health Policy of the University of Florida has a contract with Texas to evaluate the SCHIP program.
Initial survey results of parents in arrears on the new premium charges were that the great majority of the parents in the 100 percent to 150 percent of FPL category understood that their cost-sharing obligation had increased from an annual $15 fee to a monthly $15 premium.
Most parents, according to the survey, thought the premium was a reasonable price to pay for coverage, but an even greater percentage said they could not afford the new, higher premiums.
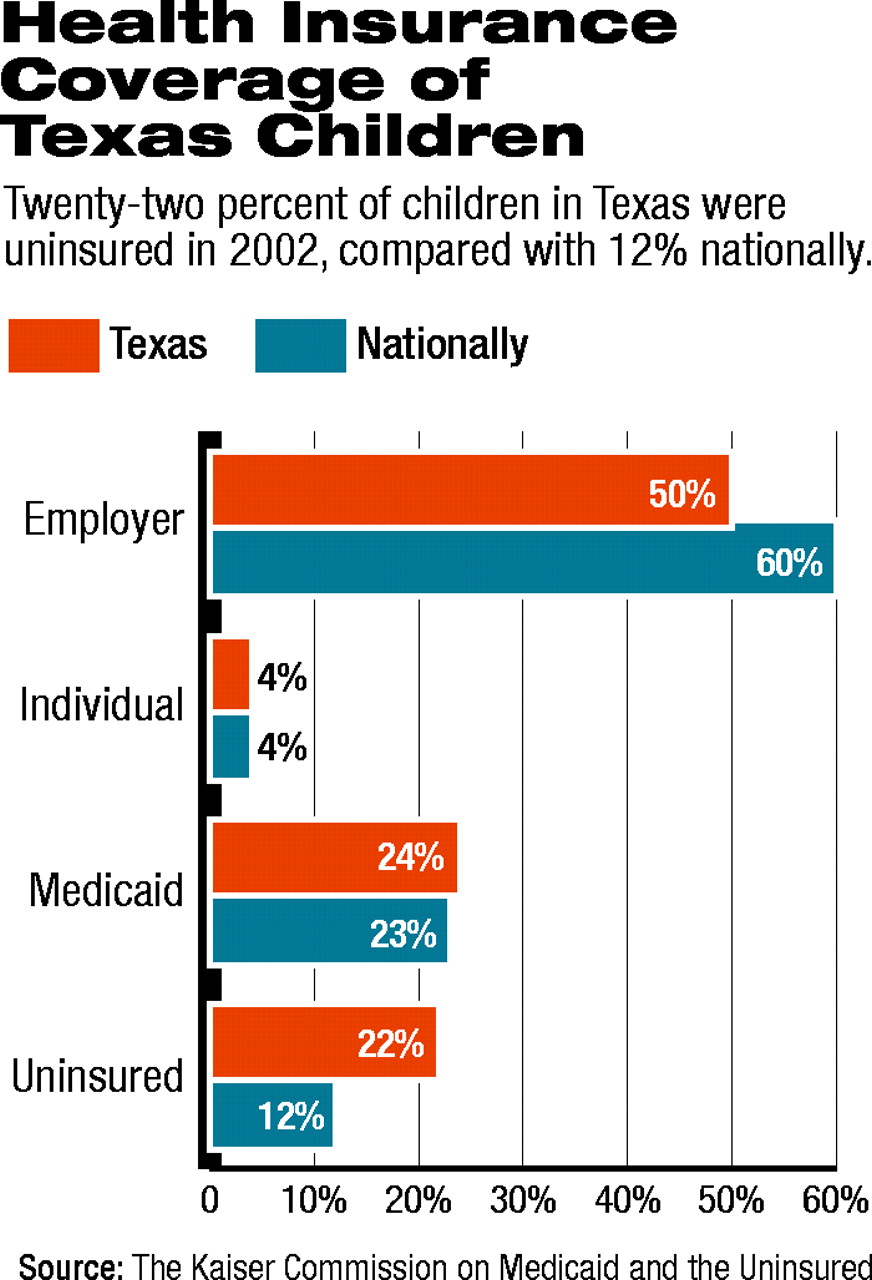
Dunkelberg pointed out that the decline in enrollment is particularly serious because Texas has one of the nation's lowest rates of employer-sponsored coverage and the highest rate of uninsured children in the country. Twenty-two percent of children in Texas are uninsured, compared with 12 percent for the country as a whole (see chart).
“Children's Medicaid and SCHIP in Texas: Tracking the Impact of Budget Cuts” is posted online at<www.kff.org/medicaid/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=44415>.▪