The idea for a robust public health system in England was born in 1942, when mass casualties were expected during World War II. When the war ended, the idea of a welfare state with cradle-to-grave social services for all became popular in the country.
The National Health Service (NHS) was envisioned to be tax supported, free to all, and based on community care, with general practitioners and community health centers at its core.
The NHS, which was fully established in England by 1948, has continued to grow, becoming the largest governmental organization in Europe with more than 1 million employees, according to the NHS Web site.
The government has run the NHS since 1948 without national standards, patient choice of health care providers or treatment, and adequate staffing or funding, according to a Department of Health (DoH) statement. The DoH is responsible for improving the health and well-being of England's population.
In his re-election campaign, Prime Minister Tony Blair promised to reform the NHS and increase its funding. His government made good on that promise and is implementing a detailed plan for reform combined with modest funding increases.
In 2002 a cabinet minister was appointed secretary for health and head of the DoH.
The health secretary works with five health ministers. Each minister is responsible for several, often diverse, areas. For example, the minister responsible for adult mental health services also oversees dentistry, emergency care, diabetes, and patient and public involvement, said Richard Beinecke, D.P.A., at last month's Mental Health Policy Roundtable meeting at APA headquarters (
see article above). He spent three months in the United Kingdom last spring to learn about the organization and delivery of general health, mental health, and social services.
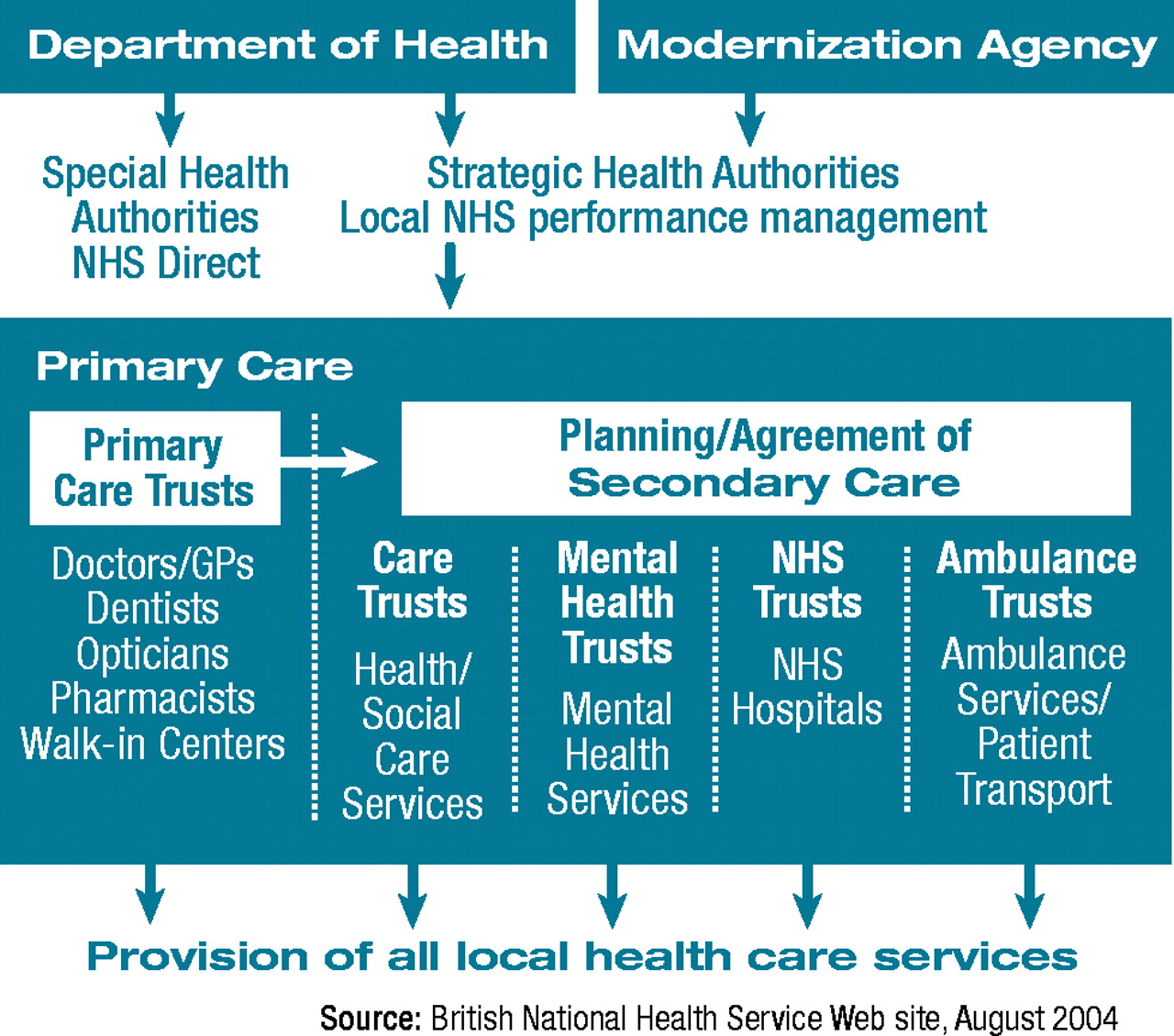
A major reform within the NHS is the transfer of service planning authority and funding from the central offices in London to locally based primary care trusts (organizations). “The goal is to design services around patients and put them first,” according to a report from the NHS.
Strategic planning for NHS was delegated to 28 new health authorities renamed Strategic Health Authorities (SHA). Each SHA covers about 1.5 million people and develops plans for improving local health services and ensuring that the quality of services is high and national priorities are integrated into local health service plans, according to Beinecke.
The government has promised that 75 percent of the NHS budget will be transferred to local health authorities, according to the NHS.
The primary care trusts also decide which secondary services to contract for. Secondary care is specialized and covers mental health, integrated care, NHS hospitals, and ambulance services, Beinecke explained.
People with severe mental illnesses including severe anxiety problems or psychotic illness usually are referred by their primary care physicians to specialists for mental health treatment, according to the NHS. For milder problems including marital and bereavement concerns, patients are generally advised to seek help from primary care professionals.
Mental health teams work in community settings. Specialized care is provided by crisis resolution teams, assertive outreach teams, early intervention teams, and prison-in-reach teams, which support the health staff in prisons, said Beinecke.
There has been a renewed emphasis on integrating general health, mental health, and social services funded by the NHS, Beinecke said. The 1999 Health Act allowed local authorities and the NHS to set up local integrated care organizations called “care trusts” and pool budgets, according to Beinecke.
A small number of these trusts have been established, but more are expected in the future.
A detailed description of the reorganized NHS is posted online at<www.nhs.uk/england/aboutTheNHS/default.cmsx>. The summary of the NHS plan is posted online at<www.publications.doh.gov.uk/deliveringthenhsplan.index.htm>.▪