APA is leading the campaign that recently led to the reintroduction of federal legislation to end the 50 percent copayment required for outpatient psychiatric services under the Medicare program.
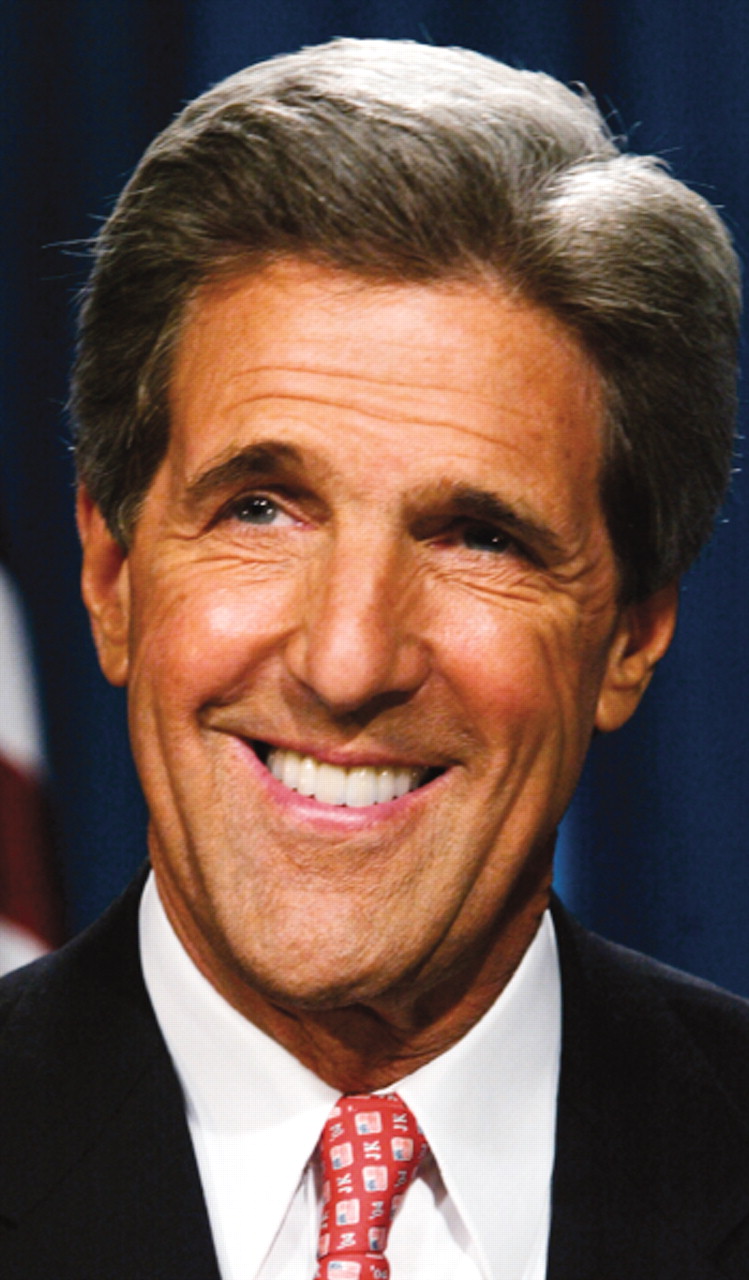
It is the second time the Medicare Copayment Equity Act has been introduced by Sens. Olympia Snowe (R-Maine) and John Kerry (D-Mass.). They first introduced it in April 2003.
“Medicare's current policy places an undue burden on individuals and families suffering from mental illness, and our society as a whole,” Snowe said in introducing the bill. “Not only will this legislation end an outdated distinction between physical and mental disorders and ensure Medicare beneficiaries have equal access to treatment for all health conditions, it will also begin to eliminate stigmas and misunderstandings associated with mental health disorders. I am proud to offer this legislation to provide more equitable treatment to those struggling with mental illness.”
The legislation, which APA's Department of Government Relations has been intensely involved in developing, is being hailed by more than 30 other professional and advocacy organizations under the umbrella of the Mental Health Liaison Group (MHLG).
A May 26 letter from the MHLG to Kerry and Snowe, initiated by APA, outlined the group's opposition to the 50 percent copayment requirement.“ We were fortunate to have all of those involved in advocacy for the mentally ill behind us on this issue,” said Nicholas Meyers, director of APA's Department of Government Relations.
In a separate letter to the senators, APA Medical Director James H. Scully Jr., M.D., expressed APA's longstanding interest in ending the 50 percent copay requirement, which applies to psychiatric care but not other types of medical treatment.
“We are of course cosigners of the MHLG letter, but I wanted to add my own personal thanks for your tireless efforts to end 40 years of discrimination against patients seeking outpatient mental health services under Medicare Part B,” Scully wrote. “It should be simply unacceptable to compel such patients to pay 50 percent of the cost of their care out of their own pockets. The real winners under your legislation are patients.”
The MHLG letter, sent the same day, echoes those sentiments.
“Simply put, current law discriminates against Medicare beneficiaries who seek treatment for mental illness,” the group stated. “This affects elderly and nonelderly Medicare beneficiaries alike when they seek mental health care. According to the 1999 U.S. surgeon general's report on mental health, almost 20 percent of elderly individuals have some type of mental disorder uncommon in typical aging. In addition, elderly individuals have the highest rate of suicide in the U.S., often the result of depression.”
The MHLG letter quoted the 1999 “Mental Health: A Report of the Surgeon General,” which noted that depression is particularly costly because of the excess disability that it causes and its deleterious interaction with physical health.
“The 50 percent coinsurance requirement also is unfair to the nonelderly disabled Medicare population,” the MHLG wrote to the senators. “Because many of these individuals have severe mental illnesses combined with low incomes and high medical expenses, a 50 percent coinsurance obligation is a serious patient burden. For elderly and nonelderly Medicare beneficiaries alike, Medicare is a critical source of care. Your legislation to ensure that Medicare beneficiaries needing mental health care incur only the same cost-sharing obligations as required of all other Medicare patients would end the statutory discrimination against Medicare beneficiaries seeking treatment for mental disorders.” ▪