Nearly 40 percent of Colorado Medicaid recipients had a psychiatric diagnosis, and they incurred twice as much in total health care costs than those without a psychiatric diagnosis between January and December 2000, according to a recent study.
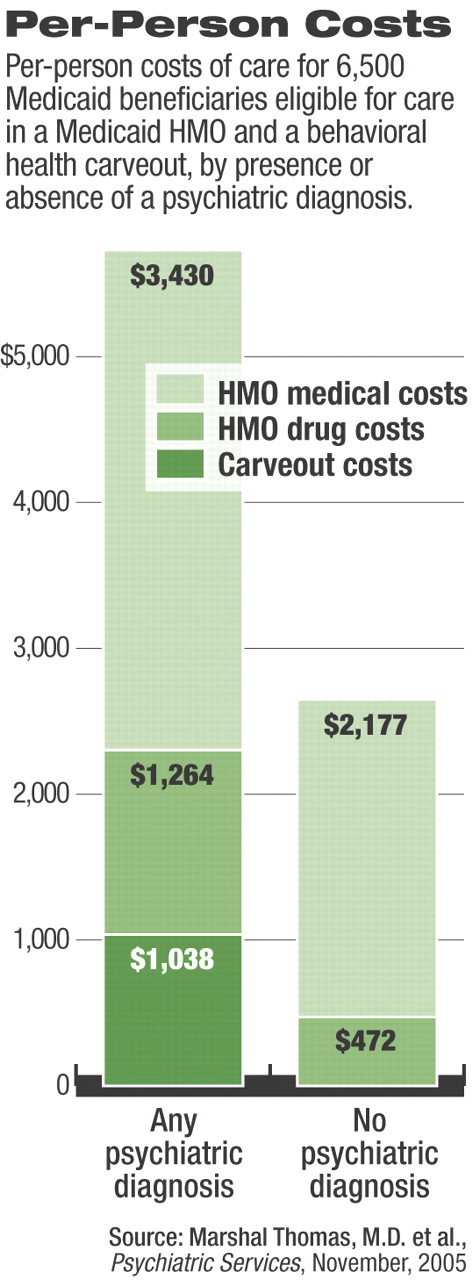
The cross-sectional observational analysis of adult beneficiaries in a Colorado Medicaid health maintenance organization (HMO) looked at claims data of 6,500 Medicaid beneficiaries eligible for services in both the HMO and a behavioral health carveout program.
The study was published in the November Psychiatric Services. It echoed the findings of previous research that found patterns of elevated general health costs in people with a range of mental disorders, but this study extended those findings to a Medicaid program.
“Most people are struck by how big of an impact mental health has on Medicaid and how prevalent mental health disorders are and how costly they are,” said Marshall Thomas M.D., the study's lead author and vice chair of the Department of Psychiatry and Health Science at the Health Science Center of the University of Colorado at Denver.
In the last 10 to 15 years, Marshall said, medical professionals and public-policy experts have become increasingly aware of the importance of mental health issues in general medical and primary care populations. But even with that increased awareness, many continued to underestimate the importance of mental health issues within Medicaid and uninsured populations, where these issues play an even more significant role than in commercially insured populations, he said.
The study found that 40 percent (2,597) of the 6,500 patient claims studied included a psychiatric diagnosis.
Patients with psychiatric diagnoses had 2.24 times higher overall health care costs than patients without such a diagnosis ($6,995 vs. $3,121). The overall health care costs included medical and pharmaceutical costs. The psychiatric disorder costs ranged from $7,284 in overall health care costs for patients with a depressive disorder to $8,567 for patients with bipolar disorder.
More serious psychiatric disorders, such as bipolar and psychotic disorders, incurred higher costs through psychiatric treatment, while those with more common conditions, such as anxiety, substance use, or depressive disorders, incurred most of their costs through increased general medical care.
The practical impact of a Medicaid system such as Colorado's, which uses a separate carveout program for mental health services, is greater support to those with serious and persistent mental illness, according to the study authors. But the same system tends to keep less severe conditions, such as anxiety and substance abuse, in the general medical setting. Only a third of patients with a diagnosis of a mental health disorder on a claim form had specialized mental health treatment within the study period.
Other conditions that may contribute to the lack of mental health care for many patients who need it, according to the researchers, are the HMOs' lack of mental health services and the behavioral health carveout organizations' exclusive focus on mental health services.
“So in order to address the mental health needs of the two-thirds that don't go to mental health providers, you have to develop ways that focus on taking care of those issues in general medical settings,” said Thomas, who is also vice president for medical services and chief medical officer at Colorado Access, a nonprofit Colorado Medicaid health plan.
Benjamin Druss, M.D., author of another study on costs of depression care in Medicaid, and Rosalynn Carter Chair in Mental Health in the Rollins School of Public Health at Emory University, said the study indicated that accountability for the patient's overall health is urgently needed in Medicaid systems. Overall accountability may help control the costs that mental health care patients place on Medicaid, even while greatly improving the patients' health.
“If you have certain interventions that might incur higher costs in the behavioral treatment setting but improve care or improve efficiencies of services in other kinds of settings, like medical care, it is very hard to get those implemented in systems where there is no higher level of accountability across the whole patient,” Druss said.
The study is important, Druss said, because its finding that Medicaid patients with mental illness incur higher costs comes as Medicaid is seen as an increasingly important provider of mental health services, and states are cutting Medicaid budgets. The study shows better control of the mental health conditions of Medicaid recipients may make a major financial impact.
In Medicaid systems that use carveouts, such as Colorado's, the system allows most mental health conditions to go un-treated because there is no examination of the overall health of patients, Druss said.
“If we are going to be carving out certain elements of their care we need at the end of the day to put the pieces together and understand how these patients as a whole are obtaining their care,” he said.
Thomas said the study may underestimate the true extent of mental illness within Medicaid populations because there is little incentive in systems like Colorado's to seek out those with mental illness within general health care settings.
Psychiatr. Serv. 2005 56 1394