Substance abuse treatment advocates in California have a new tool to gather support for increased funding, with the release of a recent study that found every dollar spent on substance abuse treatment generates more than $7 in monetary benefits for society.
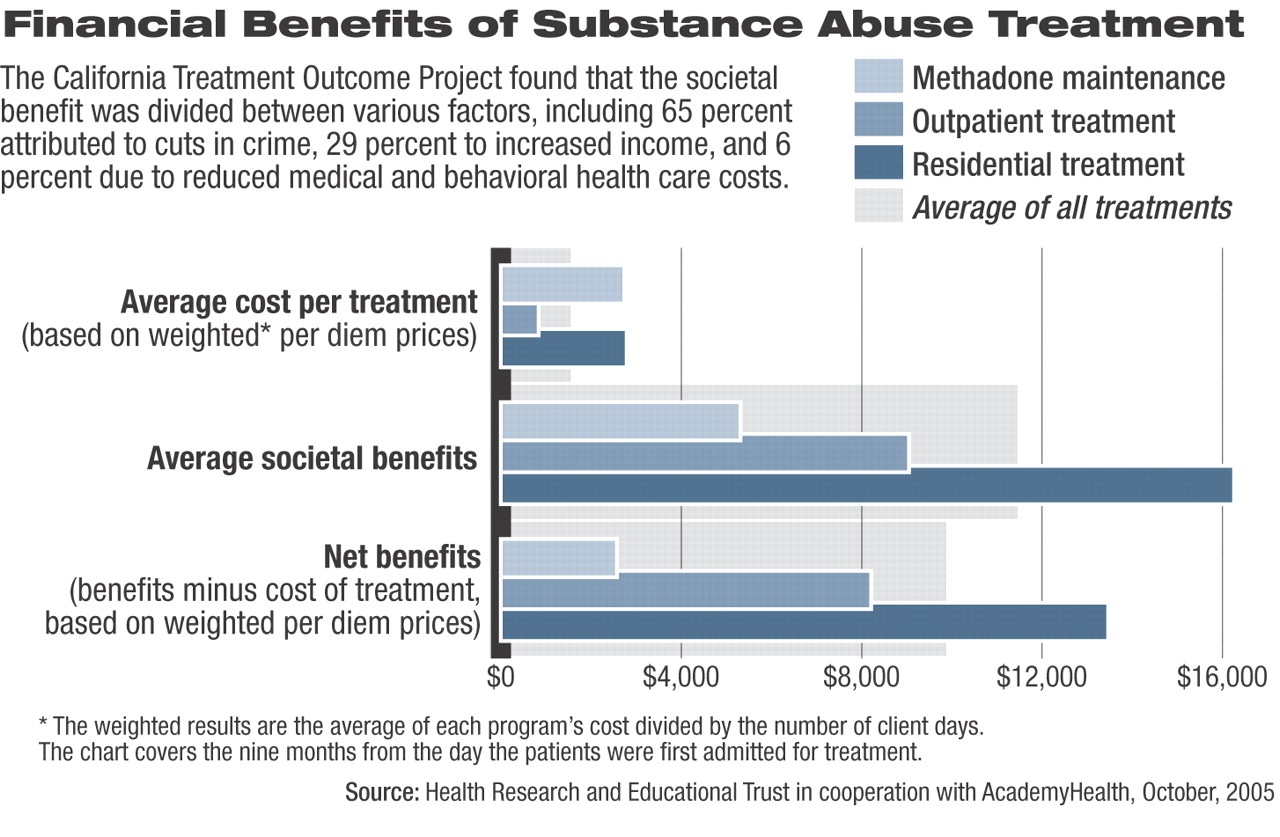
The study, published in the November Health Services Research, found that the average substance abuse treatment cost in California is $1,583 per patient and is associated with a societal benefit of $11,487 in return, which is more than a 7-to-1 ratio of benefit to costs. The ratio rose to 9-to-1 when the researchers inflated arrest data to approximate actual crimes committed. The ratio is based on weighted average treatment costs and benefit measures that demonstrated significant change. Weighted average is each program's cost divided by client days.
All of society is already paying huge costs imposed by hard-core substance abusers, said Susan Ettner, Ph.D., lead author and a professor of general internal medicine and health services research at the David Geffen School of Medicine and School of Public Health at the University of California at Los Angeles.
Ettner said investments in substance abuse treatment make good business sense, without even considering the associated prevention of human suffering and victimization.
The societal benefit was divided between various factors, including 65 percent attributed to cuts in crime, 29 percent to increased income, and six percent due to reduced medical and behavioral health care costs.
The treatment costs were estimated based on the length and average daily cost of each type of substance abuse treatment.
The study was based on data from the California Treatment Outcome Project (CalTOP), which collected outcome data on persons admitted to 43 substance abuse treatment providers in 13 California counties, including three methadone maintenance programs, 19 drug-free outpatient programs, and nine residential programs. The study had a response rate of 72 percent. The patient findings were based on 2,567 patients entering substance abuse treatment between January 2000 and May 2001 who also completed a nine-month follow-up survey.
Cost reductions occurred in hospital inpatient use, emergency room visits, and mental health services. “Victimization costs” dropped by $3,019, and other costs associated with criminal activities were reduced by $2,657. Incarceration costs dropped by $1,788, and personal earnings increased by $3,352. The monetary benefit findings were based on the survey and administrative data, which included medical care, mental health services, criminal activity, earnings, and government payments. The monetary benefits were based on a comparison of the costs each patient incurred before treatment with costs after treatment, so each client served as their own“ control.”
The California Department of Drug and Alcohol Programs, the Center for Substance Abuses Treatment, and the Robert Wood Johnson Foundation provided funding for the study.
The research echoes similar findings in other studies over the past 11 years. The project is the successor to CalDATA, which presented similar but less comprehensive data in 1994. The CalDATA study found the same cost-benefit ratio of 1 to 7, which surprised and pleased the authors.
“We were surprised because there have been many changes in treatment approaches since those data were collected, but it's also comforting because we used a different methodology to reach the same conclusion,” Ettner said.
Other studies have identified cost-benefit returns for substance abuse treatment that range from 1-to-4 in federally funded programs to 1-to-23 in a Washington state clinic.
The authors said the study improves on previous research in this area in several ways, including the use of a larger sample and reviewing data at multiple facilities.
The authors pointed out that their findings should be interpreted with caution because of the study limitations. The results may not generalize to non-CalTOP providers in other states. One potential limitation was that compared with the statewide data, the CalTOP sample slightly under-represented methadone clients, although statewide methadone clients only account for 10 percent of the total treatment population.
The study authors said the stigma associated with substance abuse and underlying skepticism about the value of rehabilitation can lower the chances that substance abuse treatment will be funded. That reality puts pressure on advocates to show that the benefits of substance abuse treatment are monetary, as well as medical.
“The state funded this because they felt like the question of program cost versus benefit had not been definitively answered,” Ettner said.
Herbert Kleber, M.D., vice chair of APA's Council on Addiction Psychiatry, praised the study but warned that hopes for it to broadly impact public policy may be overly optimistic. Policymakers usually give their anecdotal experience with relapse among family and acquaintances more weight than carefully conducted research.
“The problem is that lawmakers and policymakers tend to be unimpressed by data showing the success of drug treatment because they know it doesn't work,” Kleber said about the confidence some leaders place in their personal observations of addiction.
Advocates of addiction treatment also need to overcome policymakers' conviction that addiction is not a true disease but is “a moral failing.”
The funding will only increase when the public is convinced it must increase and brings pressure on elected officials to approve increased funds, Kleber said.
“Benefit-Cost in the California Treatment Outcome Project: Does Substance Abuse Treatment `Pay for Itself'?” is posted at<www.blackwell-synergy.com/toc/hesr/0/0?>.▪