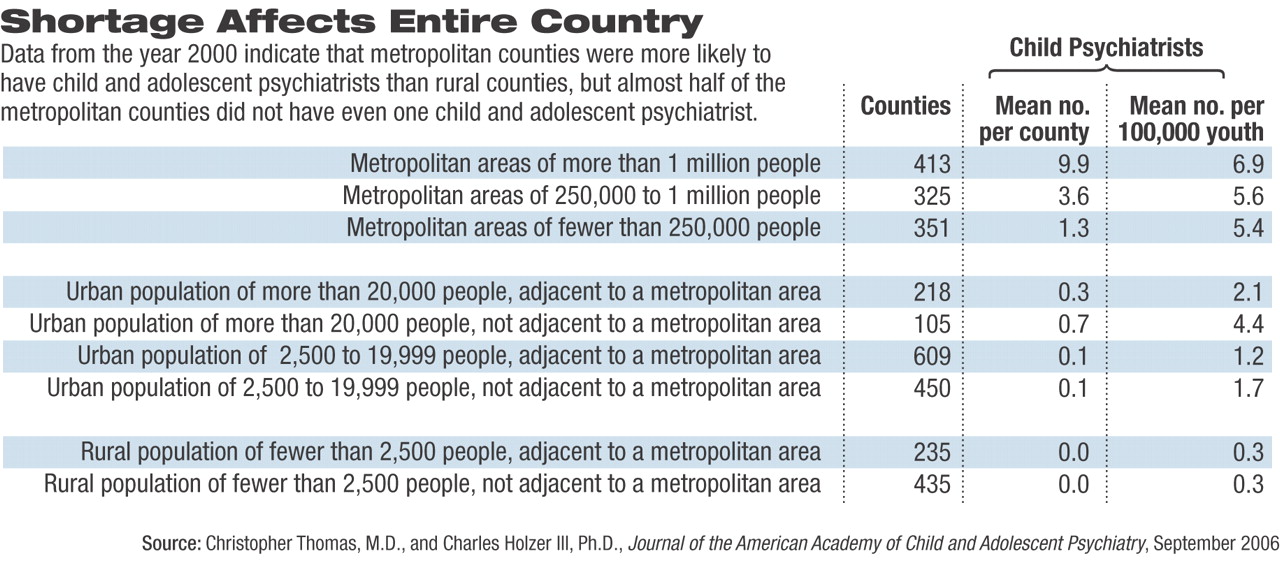
The number of child and adolescent psychiatrists per capita rose from 1990 to 2001, but still fell short of the need, a shortage compounded by an unequal distribution of practitioners, according to a recent report by Christopher Thomas, M.D., and Charles Holzer III, Ph.D., of the Department of Psychiatry and Behavioral Sciences at the University of Texas Medical Branch at Galveston.
Rural counties and those with high poverty rates, regardless of population, had few or no child psychiatrists.
“Wealthier counties have not reached saturation in service, and incentives for practice in underserved areas are insufficient,” wrote Thomas and Holzer. The study was published online in the American Journal of Child and Adolescent Psychiatry on May 17 and will appear in the September print edition.
Thomas and Holzer tracked the number and distribution of child and adolescent psychiatrists from a list compiled by the Department of Health and Human Services, comparing data from 1990, 1995, 2000, and 2001. The total of 6,256 child psychiatrists is probably an overestimate, said Thompson in an interview, because not all are in active, full-time practice. Some are retired, while others are administrators, teachers, or researchers.
Data were broken down by state and county and showed a slight general increase from 1990 to 2001 in proportion to the number of young people. There was an average of 6.73 child and adolescent psychiatrists per 100,000 youth in the United States in 1990 and 8.67 in 2001. However, other studies have estimated that 14.38 child and adolescent psychiatrists would be needed per 100,000 youth in ideal circumstances, and only six states (Connecticut, Hawaii, Maryland, Massachusetts, New York, and Rhode Island) met that standard in 2001.
Often any increase in the number of child psychiatrists was outpaced by added numbers of young people. Maryland, for instance, had 64 more clinicians in 2001 than in 1990, but because there were more youngsters, the rate per 100,000 children remained nearly the same: 18.0 in 2001 versus 18.6 in 1990.
In 2001 the rate of child psychiatrists per 100,000 youth varied from 3.1 in Alaska to 21.3 in Massachusetts. Rates were also especially low in rural counties and in counties with higher percentages of youth living in poverty. Even that distribution wasn't uniform, wrote Thomas and Holzer.
“Although metropolitan counties were more likely to have child and adolescent psychiatrists than rural counties, almost half the metropolitan counties did not have even one child and adolescent psychiatrist,” they said.
Many psychiatrists in urban areas do not accept third-party reimbursement, which limits the number of psychiatrists available to provide services through managed care organizations.
Several factors may account for the slow growth in the numbers of child and adolescent psychiatrists, said Thomas in an interview. Child psychiatry is a subspecialty and requires three years of general psychiatry residency plus two years of child psychiatry.
Medical school debt, the bane of most new physicians, exerts its influence in their choice of specialty. Half of first-year residents who say they are interested in child psychiatry stay in adult psychiatry so they can begin earning income a year sooner, said Thomas Anders, M.D., of the Department of Psychiatry at the University of California, Davis, and the president of the American Academy of Child and Adolescent Psychiatry (AACAP).
Medical students may also have too little exposure to child psychiatry and thus fail to consider it as a career option, said Anders. Stigma plays a role, too, he said. “To go into child psychiatry takes courage and exposure.”
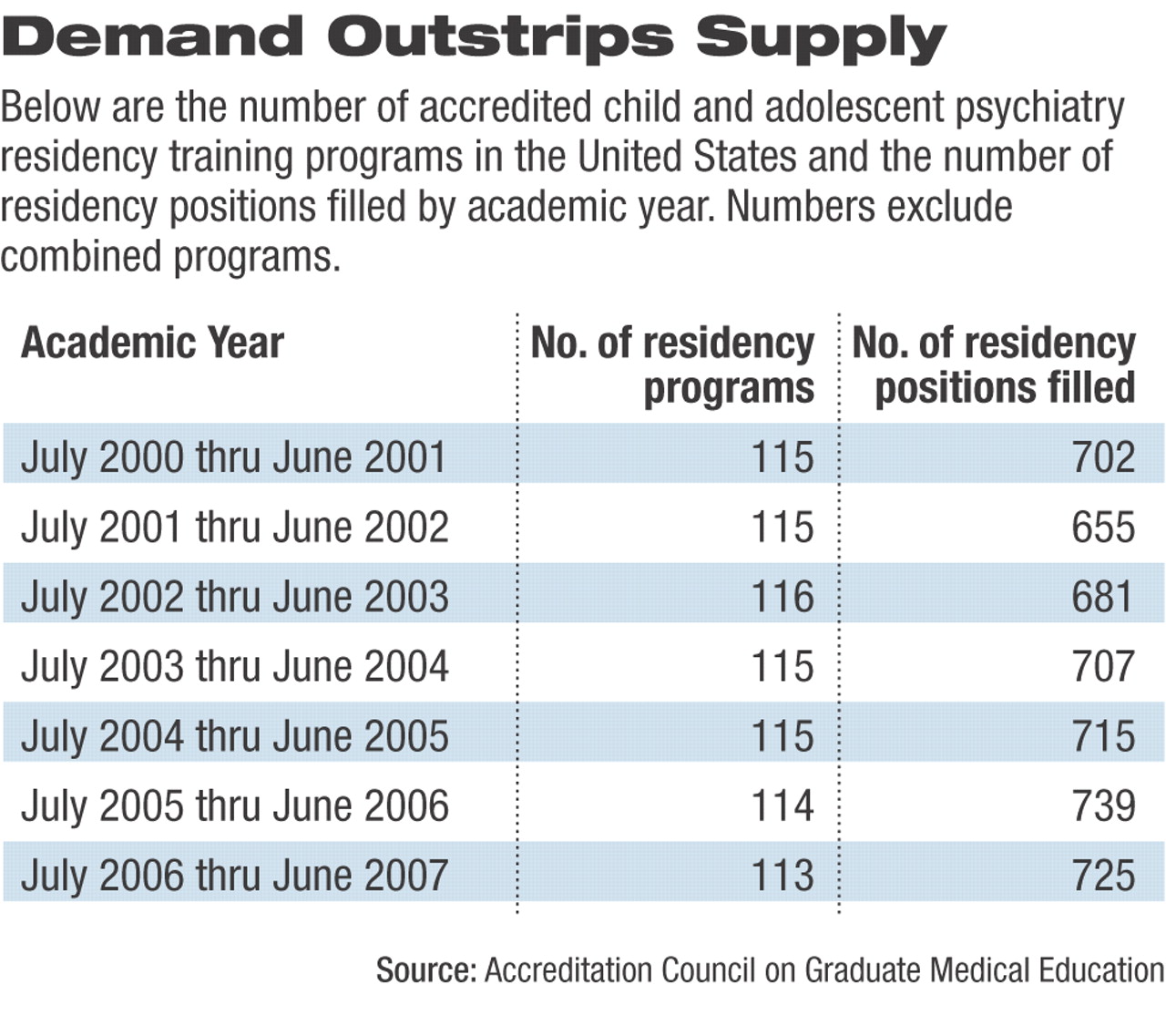
About 10 percent of child psychiatry residency slots go unfilled each year, so AACAP (in cooperation with APA) is trying to raise the visibility of the subspecialty among medical students and PGY-1 and PGY-2 psychiatry residents, said Anders. Increasing residency slots is difficult because it takes funding, approval from the institution and accrediting bodies, supervision, and additional patients who can afford such care or have insurance that covers it.
The organization has seen success with a triple-board program, developed jointly by AACAP, APA, the American Academy of Pediatrics, the American Board of Psychiatry and Neurology, and the American Board of Pediatrics, that now takes in 21 new residents each year at 10 institutions, said Anders. These residencies require two years of pediatrics, followed by three years of an integrated adult and child psychiatry curriculum (Psychiatric News, March 3).
AACAP has also proposed a pilot project allowing board certified/eligible family physicians or pediatricians to enter the last three years of such programs and expects a decision from the Residency Review Committee in Psychiatry in October. A “radical” faction has even suggested making child psychiatry its own specialty (as opposed to the current designation as a subspecialty) to reduce the residency time spent on general psychiatry below certification levels, but that is a minority view, said Anders. “The predominant thinking is that you need adult psychiatry and that we are still a subspecialty.”
Both AACAP and APA are working on a policy level, too. Anders noted that bills have been introduced into Congress—although not yet passed—that would extend loan forgiveness programs for all mental health professions, remove the 50 percent cap on Medicare-funded training slots in hospitals for all subspecialties, and designate child psychiatry a shortage subspecialty. (Child psychiatry is already recognized as a shortage specialty by the federal Department of Health and Human Services Bureau of Health Professions and the Accreditation Council on Graduate Medical Education.)
Preliminary congressional budget proposals for Fiscal 2007 have slightly increased funding by $3 million to $300 million for the Children's Hospital Graduate Medical Education payment program, which pays for child and adolescent psychiatrists to train in hospitals. The Child Health Care Crisis Relief Act has been languishing in the House and Senate for several years. It proposes a loan-forgiveness program for child psychiatrists and mental health professionals who agree to work with seriously ill patients, are from racial or ethnic minority groups, or live in underserved areas. It is unlikely to pass soon, according to APA's Department of Government Relations.
In the meantime, AACAP is seeking to ease the shortage of child and adolescent psychiatrists by using telepsychiatry to reach rural areas, integrating services with psychologists and social workers, and increasing cooperation with pediatricians and other primary care physicians. AACAP will hold a four-day institute on child psychiatry for pediatricians at its annual meeting in San Diego in October, said Anders.
“We have to reconsider child mental health services overall,” said Thomas. “it will take time to increase our workforce, but we still have an obligation to provide the best services to our patients.”
“The Continuing Shortage of Child and Adolescent Psychiatrists” can be accessed at<www.jaacap.com> by clicking on “Online Advance Publication” and then the title of the study. ▪