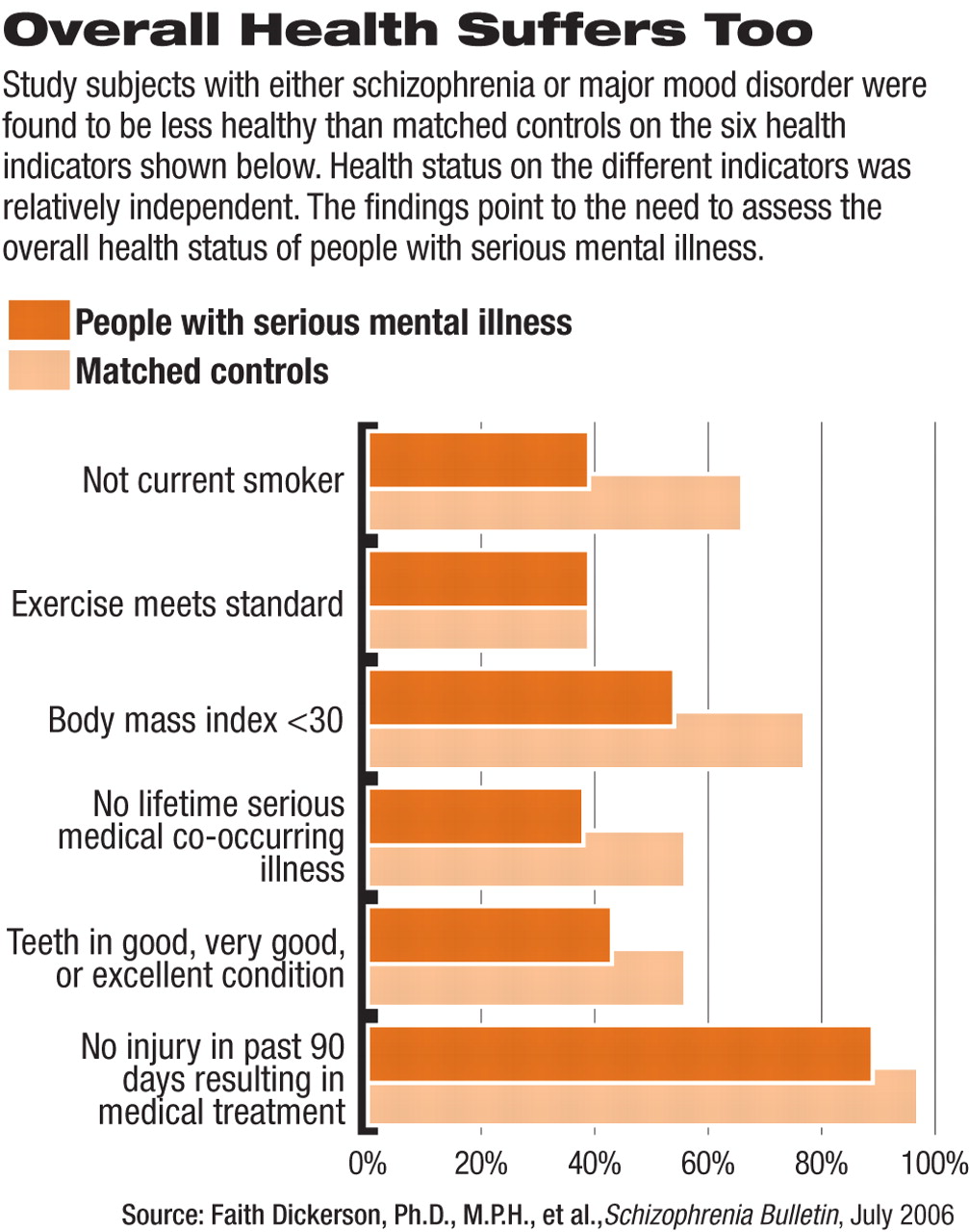
The overall health of people with serious mental illness is well below the suboptimal level found in the general population.
A comparison of patients with either schizophrenia or major mood disorder with a sample matched for age, gender, and race in the general population found that only 1 percent of those with serious mental illness met the criteria for five selected health indicators. The study appeared in the July Schizophrenia Bulletin.
Those indicators included smoking status, exercise, good dentition, absence of obesity, and absence of serious medical co-occurring illness. A sixth item, absence of injury requiring medical treatment in the previous 90 days, was also compared but was not included in the composite, according to researchers at Sheppard Pratt Health System, the University of Maryland School of Medicine, and Johns Hopkins University School of Medicine.
At the same time, only 10 percent of those in the general population met criteria for all five health indictors.
“The general population in the U.S. is hampered by health problems, but our patients are even more so,” co-author Faith Dickerson, Ph.D., M.P.H., told Psychiatric News. “We found that a very small percentage of our patient group actually met the healthy criteria for each of the items.”
She is director of psychology at Sheppard Pratt Health System in Baltimore. The study was funded by the National Alliance for Research on Schizophrenia and Depression, and the principal investigator was Lisa Dixon, M.D., of the University of Maryland.
In the study, a sample of 100 adults with schizophrenia and 100 with major mood disorder were recruited from randomly selected outpatients receiving community-based psychiatric treatment. Participants were surveyed about health indicators using items from the National Health and Nutrition Examination Study III (NHANES III) and the National Health Interview Survey (NHIS). Their responses were compared with those of matched samples from the general population surveys.
The researchers focused on survey items consistent with the leading health indicators for the U.S. population as identified by the Healthy People 2010 program of the Centers for Disease Control and Prevention. Specifically, they included being a nonsmoker (not smoking a cigarette in the previous 30 days); engaging in exercise meeting recommended standards (defined as at least 20 times a month); not being obese (a body mass index with a score of less than 30); being free of a co-occurring lifetime serious medical illness defined as arthritis, asthma, chronic bronchitis, emphysema, diabetes, congestive heart failure, hypertension, stroke, and cancer; having teeth in good, very good, or excellent condition; and not requiring medical treatment for an injury in the previous 90 days.
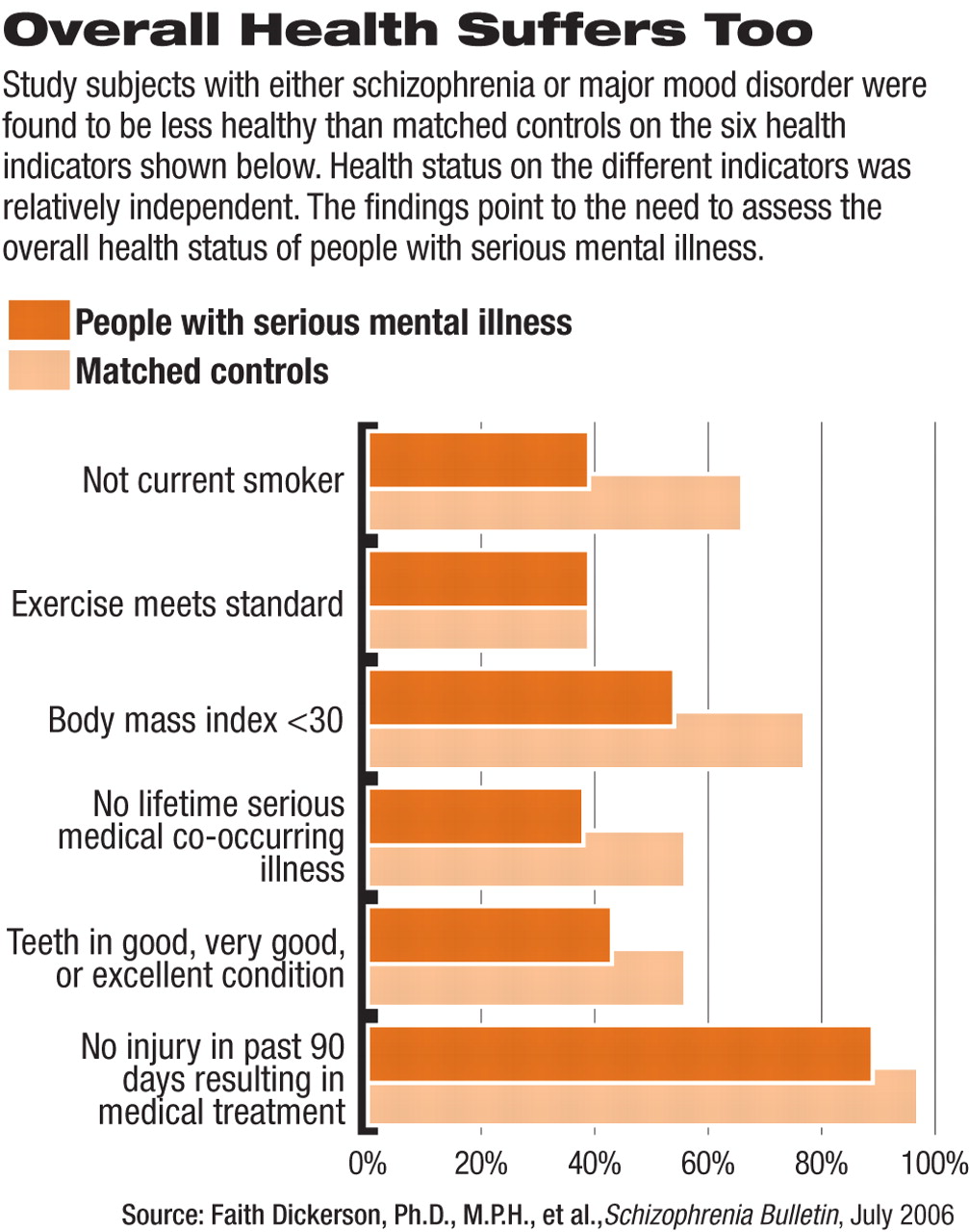
Items 1 to 5 were from the NHANES III, and item 6 from the NHIS. The differences between the two groups were statistically significant (with the mentally ill group reporting worse health) on all indicators except for exercise meeting recommended standards. On that score, 39 percent of both groups reported exercise that met recommended standards (see chart on page 21).
The researchers found that within the mentally ill group, educational level, but not diagnosis, was independently associated with a composite measure of health behaviors. There was a significant association between nonsmoking status and good dentition; between absence of obesity and absence of a co-occurring serious medical illness; and between good dentition and absence of a co-occurring medical illness. None of the other associations between individual health items was significant, nor was the association between the health behaviors and the health outcomes composites.
These findings indicate that individuals' health status on different indicators is relatively independent, Dickerson explained. The findings also argue, she said, for examining multiple health indicators to assess overall health status in persons with serious mental illness, as has been studied in the general population.
She said the study did not address whether the use of the composite indicators would be practical in everyday clinical practice, but noted that monitoring of general medical conditions in patients with serious psychiatric illness is fast becoming a major issue.
Wayne Fenton, M.D., director of adult translational research and treatment development at the National Institute of Mental Health (NIMH), has called the phenomenon of metabolic syndrome among patients with schizophrenia “an epidemic” and called for psychiatrists to be more actively involved in monitoring patients' weight and other health indicators (Psychiatric News, April 26, 2006).
Dickerson said that Sheppard Pratt Health System is looking at a more standardized way to collect health behavior and basic medical information, such as smoking, obesity, and lipid levels.
“There are increasing efforts to integrate routine health status checks into psychiatric care,” Dickerson said. “The interest in medical illness and health behaviors among people with primary psychiatric problems is fairly recent. There is a small but growing literature on the subject. With increasing interest in smoking and obesity among the general population, there has been a growing awareness that patients with serious mental illness are even more prone to these risk factors.”