Although cigarette smoking is declining in the general population, this is not the case among individuals with schizophrenia, among whom the smoking rate is 70 percent to 88 percent.
Despite these extremely high rates of smoking, little research has been conducted on ways to get schizophrenia patients to quit. In a study by Amanda Baker, Ph.D., an associate professor at the Center for Mental Health Studies at the University of Newcastle in Australia, and coworkers, motivational/cognitive behavioral therapy (CBT) sessions combined with nicotine replacement therapy were found to be “encouraging” and modestly effective.
The team reported their findings in the November American Journal of Psychiatry.
Baker and her colleagues recruited 298 individuals with a psychotic disorder who were smoking at least 15 cigarettes a day and wanted to stop smoking. Half were assigned to routine care and half to a smoking-cessation program. Those allocated to the program were counseled in eight individual weekly sessions about how to stop smoking and were given cognitive strategies to assist them in doing so. In the last four of the eight sessions, subjects were given nicotine patches to wear as well. The researchers then tracked the subjects' smoking outcomes during the following year.
There were no significant differences between the treatment group and the control group in continuous-abstinence rates or in point-prevalence-abstinence rates, measured at three, six, and 12 months. However, a significantly higher proportion of smokers who completed all treatment sessions were found to have stopped smoking at three, six, and 12 months. (At three months, the difference was 30 percent versus 6 percent for the control group; at six months, 19 percent versus 4 percent; and at 12 months, 19 percent versus 7 percent.)
Moreover, 44 percent of intervention participants who completed all treatment sessions had reduced their smoking by at least 50 percent at 12 months, compared with only 17 percent of controls—a highly significant difference that particularly impressed her, Baker told Psychiatric News.
“This is a neglected area,” Jose de Leon, M.D., a University of Kentucky psychiatrist with a special interest in smoking and schizophrenia, said in an interview. “The authors should be complimented for completing this large study.... [However,] the important outcome in this study was the smoking-cessation rate, defined as continuous abstinence after 12 months. In the intervention group it was 3.4 percent. This is a very low number, better than the 0.7 percent rate in controls, but not significantly better. [Thus,] we need new and better interventions for smoking cessation in severely mentally ill patients.”
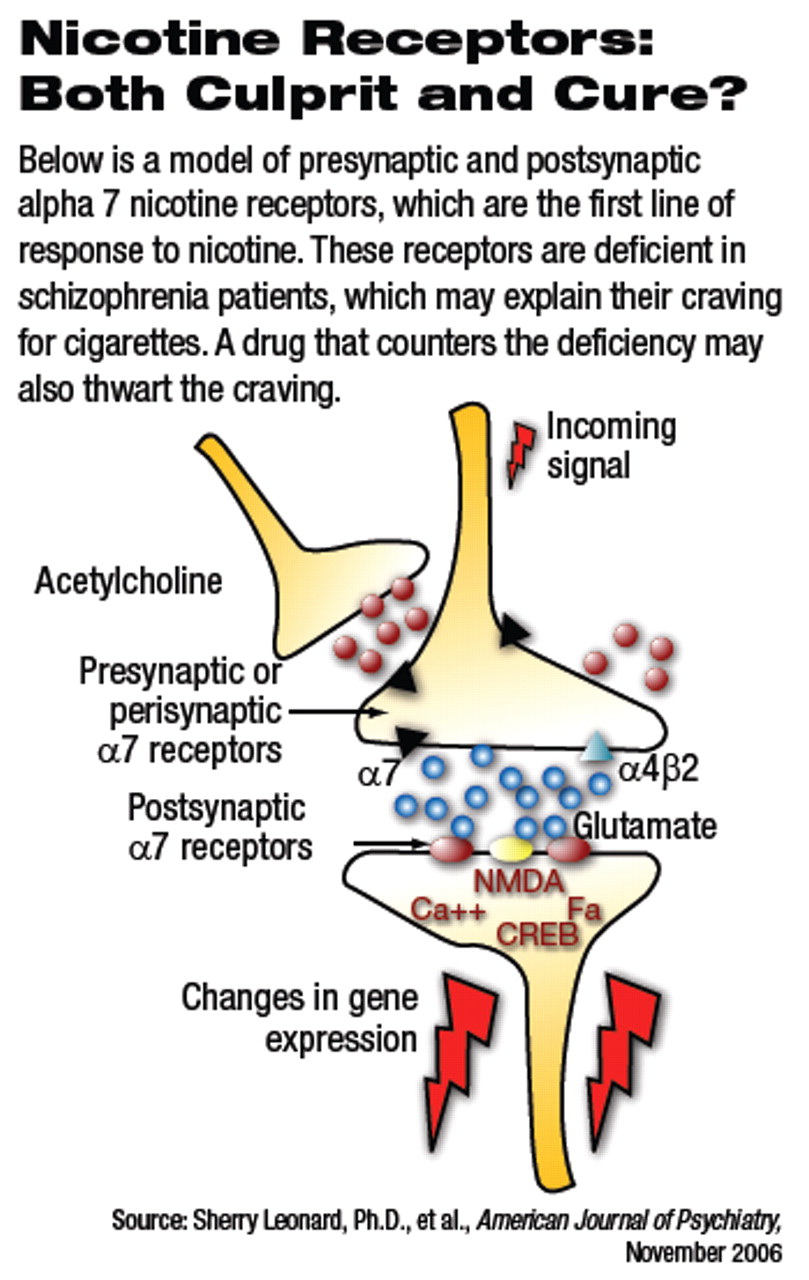
In an editorial accompanying the study report, Sherry Leonard, Ph.D., and Catherine Adams, Ph.D., professors of psychiatry at the University of Colorado, agreed. Indeed, a nicotinic receptor agonist such as DMXB-A [3-2,4 dimethoxybenzylidene anabaseine] might “provide a better adjuvant treatment for smoking cessation than the nicotine patch,” they asserted.
They explained that for schizophrenia patients, smoking may represent a form of self-medication—an attempt to treat an underlying biological deficit. Schizophrenia patients are known to have a fewer-than-normal number of nicotinic receptors, the brain's first line of response to nicotine in cigarettes. This inadequate number of nicotinic receptors may be the biological deficit that patients try to correct by smoking. Thus, if schizophrenia patients were given a drug, such as DMXB-A, that enhances the activity of nicotinic receptors, they might not feel a need to smoke, the researchers suggested.
Leonard and Adams, in fact, conjectured that giving DMXB-A to schizophrenia patients might fill two purposes—not just reduce patients' urge to smoke, but also lessen their sensory deficits and improve their cognition. The reason is that in a recent phase 1 trial in which Leonard participated, DMXB-A was found to both improve cognition and decrease symptoms in schizophrenia subjects (Psychiatric News, July 21).
A phase-2 trial testing the value of DMXB-A to schizophrenia subjects' mental well-being is now under way, Leonard told Psychiatric News.“ We will then begin a study [of DMXB-A] in schizophrenia smokers,” she said.
The study was funded by Australia's National Health and Medical Research Council, Rotary, and Community Health and Tuberculosis Australia. Nicotine replacement therapy was provided free by GlaxoSmithKline.