Congress approved a federal budget in early February that included the first cuts to entitlement programs such as Medicare and Medicaid since 1997.
The delayed vote on the budget, projected to save $39 billion over five years and $99 billion over a decade, was forced after Senate Democrats made small changes to the bill the House passed in December before adjourning.
The measure cuts about 0.3 percent of federal spending over five years but will only slightly dent the federal budget deficit. The cuts sparked opposition from mental health advocates and others, who charged Republicans with slashing necessary spending on programs that help the poor and aged to partially offset tax cuts for the wealthy. Critics of the measure also will point to provisions they say give breaks to the pharmaceutical and insurance industries at the expense of Medicare and Medicaid beneficiaries
The measure cuts about $6.4 billion from Medicare and $4.8 billion from Medicaid.
Physicians Get Some Help
The law includes a one-year freeze on Medicare physician payment rates at the 2005 levels, which averted a scheduled 4.4 percent reduction and will cost $7.3 billion annually. APA lobbied to block the planned cut and instead provide a two-year 1 percent rate increase.
“We're delighted with the efforts of Congress to address the health professional payment issue because we saw that as a potential access barrier itself by creating a significant disincentive for Medicare patients,” said Nicholas Meyers, director of APA's Department of Government Relations (DGR).
The measure dropped provisions from the earlier Senate version to establish new Medicare value-based purchasing programs, which track and reward good clinical performance for physicians and other Medicare providers. Nonetheless, the Centers for Medicare and Medicaid Services (CMS) will continue implementation of its Physician Voluntary Reporting Program (PVRP), under which physicians voluntarily send information to CMS about the quality of care they provide to beneficiaries, which APA leaders worry may later develop into a mandatory quality-reporting program. APA strongly opposes the CMS program.
The measure also dropped earlier language allowing marriage and family therapists and mental health counselors to bill Medicare independently for their services. The APA-led opposition to expanded coverage for these providers argued that “scarce resources should be spent first on addressing the discriminatory 50 percent coinsurance requirement for all mental health services,” according to Meyers.
Medicaid Beneficiaries to Pay More
The measure allows states to impose new copayments on Medicaid beneficiaries with incomes above the federal poverty line and provides states with considerable flexibility in redesigning their Medicaid programs. Copayments could apply to both services and medications. APA opposed these changes along with the rest of the mental health community.
“We are extremely cognizant of the impact of this, particularly on the poor and disabled, and we are deeply concerned,” said Meyers.
It includes controversial Medicaid “asset transfer” language that would make it harder for seniors to qualify for Medicaid coverage of their nursing home care if they have transferred any assets to children or grandchildren.
The law includes an APA-supported provision to allow low-income working parents of disabled children to buy into Medicaid, even if their income exceeds the federal poverty level.
The bill dropped an APA-supported provision for oversight requirements for states that seek to use restrictive formulary policies for atypical antipsychotic and antidepressant drugs.
The cost-sharing provisions could save about $1.9 billion over five years, a figure that jumps to $9.7 billion when projected 10 years out, according to Congressional Budget Office estimates.
Substantial Medicare Savings Projected
The Medicare cuts came from a wide variety of sources, although significant savings came from lower payments for some imaging services, spending on which has grown faster than any other service in recent years.
Lawmakers also found $6.5 billion in savings through a Bush administration plan to give higher Medicare payments to insurers that cover sicker patients and lower payments to plans that enroll healthier beneficiaries.
The measure kept alive a fund included in the 2003 prescription drug law designed to encourage preferred provider organizations to participate in Medicare. An earlier version aimed to eliminate the fund, and save $5.4 billion over five years.
The measure also provides medical relief to hurricane victims and expands some programs, including one for disabled children.
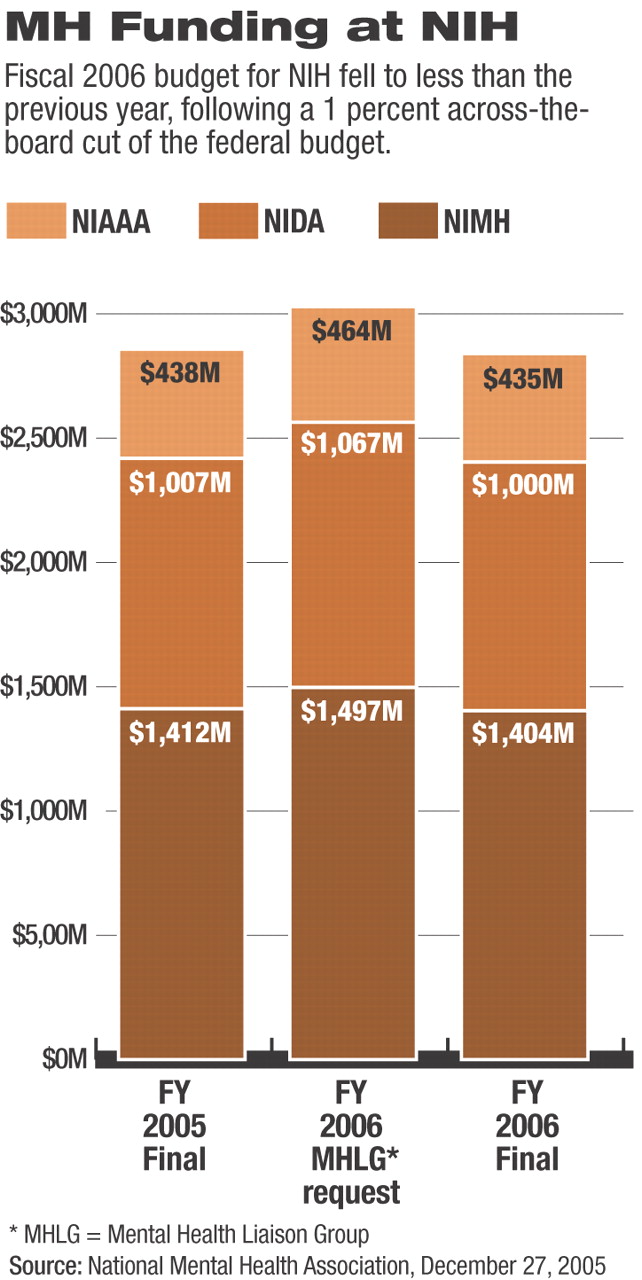
Congress approved a Department of Health and Human Services budget in December 2005 that includes a 1 percent across-the-board cut, except for veterans programs, from Fiscal 2005 levels. The measure included an additional $30 million from the earlier version of the spending bill toward implementation of the new Medicare prescription drug program.
The National Institutes of Health (NIH) received its smallest percentage increase since 1970. The Center for Mental Health Services (CMHS) was cut by $8 million.
“We knew that was coming, and Congress had to use that to trim the budget and trim spending,” said Lizbet Boroughs, deputy director of APA's DGR. “However, when you are talking about cutting $220 million out of an agency like NIH, that is significant.”
Among the practical implications of such cuts is the decision of the Substance Abuse and Mental Health Services Administration (SAMHSA) to reduce the amount it can offer its grant recipients. For instance, instead of funding 85 percent of a grant application, the agency might be able to pay only 82 percent or 83 percent of an application.
There have been no specific agency statements about what trade-offs they will make to meet the lower budget limit. The cut is also expected to trim the rate at which the NIH approves new research grants from the 2005 rate of 22 percent to an expected rate of 19.5 percent. Similar impacts are expected at SAMHSA and CMS.
Congress also moved to shore up mental health services for veterans by designating $2.2 billion of the $22.5 billion Department of Veterans Affairs medical services budget for mental health care.
“The language is very clear, and Congress was very emphatic, but now it is up to advocacy groups to hold the VA accountable,” Boroughs said about the mental health funding designation.
The measure also instructs the VA to come up with a plan to establish Posttraumatic Stress Disorder Clinical Teams at every medical center in part because of concern that large numbers of soldiers returning from Iraq and Afghanistan are suffering from the disorder. ▪