By their first day at the University of Maryland School of Medicine in Baltimore this fall, students are expected to have completed computerized training in the Health Insurance Portability and Accountability Act. Their initial orientation will include a “do's and don'ts” fashion show.
On their second day, students will go to the hospital and meet patients, some quite ill. Afterward they will explore feelings about these encounters with house staff and faculty. Since students will start to dissect a cadaver right after orientation, instructors hope to sensitize them to the solemnity of that task.
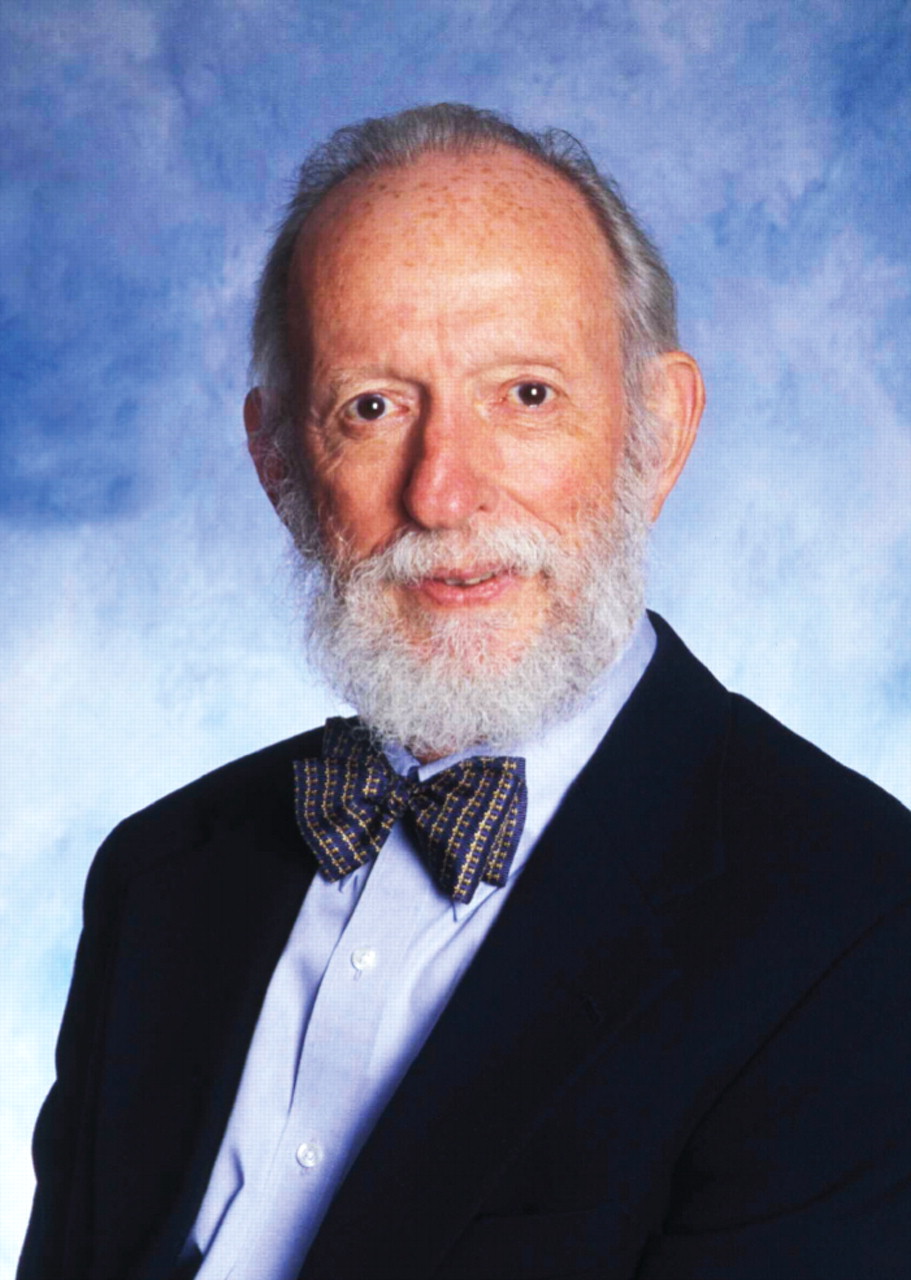
Although instilling high ethical and humanistic values has long been a central tenet of medical education, attaining this goal has become an explicit focus of today's medical school curriculum, reports John Talbott, M.D., a professor of psychiatry at Maryland, and key architect of Maryland's professionalism program.
Schools hope this effort will prevent inappropriate behavior after students graduate, said Talbott, APA president in 1984-85. A retrospective study conducted by researchers at the University of California, San Francisco, he said, showed that students cited for poor attendance or patient care while in medical school were nearly nine times more likely than peers to be disciplined by a state medical board for acts of negligence or use of drugs and alcohol after they became practicing physicians. The study was reported in the December 22, 2005, New England Journal of Medicine.
The Medical School Objectives Project of the Association of American Medical Colleges (AAMC) now specifies that students demonstrate evidence of professionalism prior to graduation, Talbott noted. Professionalism also is assessed in four of the six core competencies evaluated in each resident in every specialty, according to guidelines of the American Committee for Graduate Medical Education and the American Board of Medical Specialties.
Talbott's involvement with Maryland's professionalism project began in 1999. Approaching his 65th birthday, Talbott stepped down after 15 years as Maryland's chair of psychiatry. The free time he had been anticipating evaporated when the medical school's dean, Donald Wilson, M.D., asked him to assess how well the school's recently revamped curriculum addressed professionalism issues.
This task called for an exploration of every aspect of becoming a physician, Talbott said, from the medical school admission process to assessment at graduation and beyond, into early years of postgraduate training.
“Starting in fall of 2000, I interviewed everyone who ran a course or clerkship, and I sat in on classes,” Talbott recalled.
He examined how the school taught students to subordinate their interests to those of their patients; to relate to people of different ages, genders, races, cultures, and socioeconomic status; and to discuss death and dying, sexuality, and other sensitive topics. He looked at the influence of faculty and house-staff role models and the impact of gifts from industry.
He also attended AAMC meetings that focused on professionalism and read widely in the burgeoning academic literature on this topic.
Other medical schools, including those of the University of Toronto, McGill University, University of Virginia, and Dartmouth, Talbott said, shared information about their professionalism programs.
'Do We Have a Problem Here?'
“Talbott spent a huge amount of time asking faculty, students, administrators, hospital staff, and others, 'Do we have a problem here? If so, what's the nature of it, and what can we do to fix it?'” attested David Mallott, M.D. associate dean for medical education and an associate professor of psychiatry at Maryland.
In his report to the dean, Mallott said, Talbott provided an anthropological study of how the institution addressed professionalism.
Talbott's report, readily accepted by Maryland's deans and faculty, urged establishment of a curriculum coordinating committee to shepherd its recommendations into practice.
“I suggested naming a nonpsychiatrist clinician to chair this committee,” Talbott said. “I didn't want professionalism to be seen as touchy-feely stuff.”
Wilson and others, however, urged Talbott to take on the job.
“Students need to understand what lifelong interaction with patients should be, as opposed to simply learning how to look at laboratory data and x-rays, said Wilson, who retired as dean in 2006 and now directs Maryland's program in minority health and health disparities education and research.
Physicians in every specialty need to listen to patients and try to see the patient's perspective, Wilson added. “Talbott had both expertise and interest in teaching that task.”
House Staff, Faculty Included
Talbott urged expanding the program to include house staff and faculty, Wilson said, so students also benefit from better mentoring.
“My instinct was wrong,” Talbott conceded. “Psychiatrists have a lot to offer in this arena. They are experts in communication, feelings, and the doctor/patient relationship.”
At Maryland, groups of about seven students and four faculty meet two hours a week for at least the first two years of school to discuss case vignettes that present multiple intellectual and ethical quandaries. Students also meet with patients, such as a woman with Down syndrome, and families, such as parents whose child died of Tay-Sachs disease, to gain insight into the patient and family perspective and appreciation for the value of narrative history.
Talbott encourages students to keep journals “to gain a deeper understanding of what they are doing and why they are doing it.”
When pondering ethical dilemmas, “students often know what they should do but not what they actually would do,” said Latricia Cook, a member of Maryland's student-run humanism interest group. “Just getting people to think about possible choices is useful,” said Cook, who received her M.D. degree in May.
Maryland has established a humanism honor society, part of the Arnold Gold Foundation's national humanism honor society, Talbott said. It annually inducts 10 to 15 seniors nominated by their peers and gives awards to faculty and residents. About half of the nation's medical schools have such societies.
Talbott and Mallott are writing a book on professionalism. Their article,“ Professionalism, Medical Humanism, and Clinical Bioethics: The New Wave. Does Psychiatry Have a Role?” appeared in the November 2006 Journal of Psychiatric Practice.
Information on the AAMC's Medical School Objectives Project is posted at<www.aamc.org/meded/msop>.▪