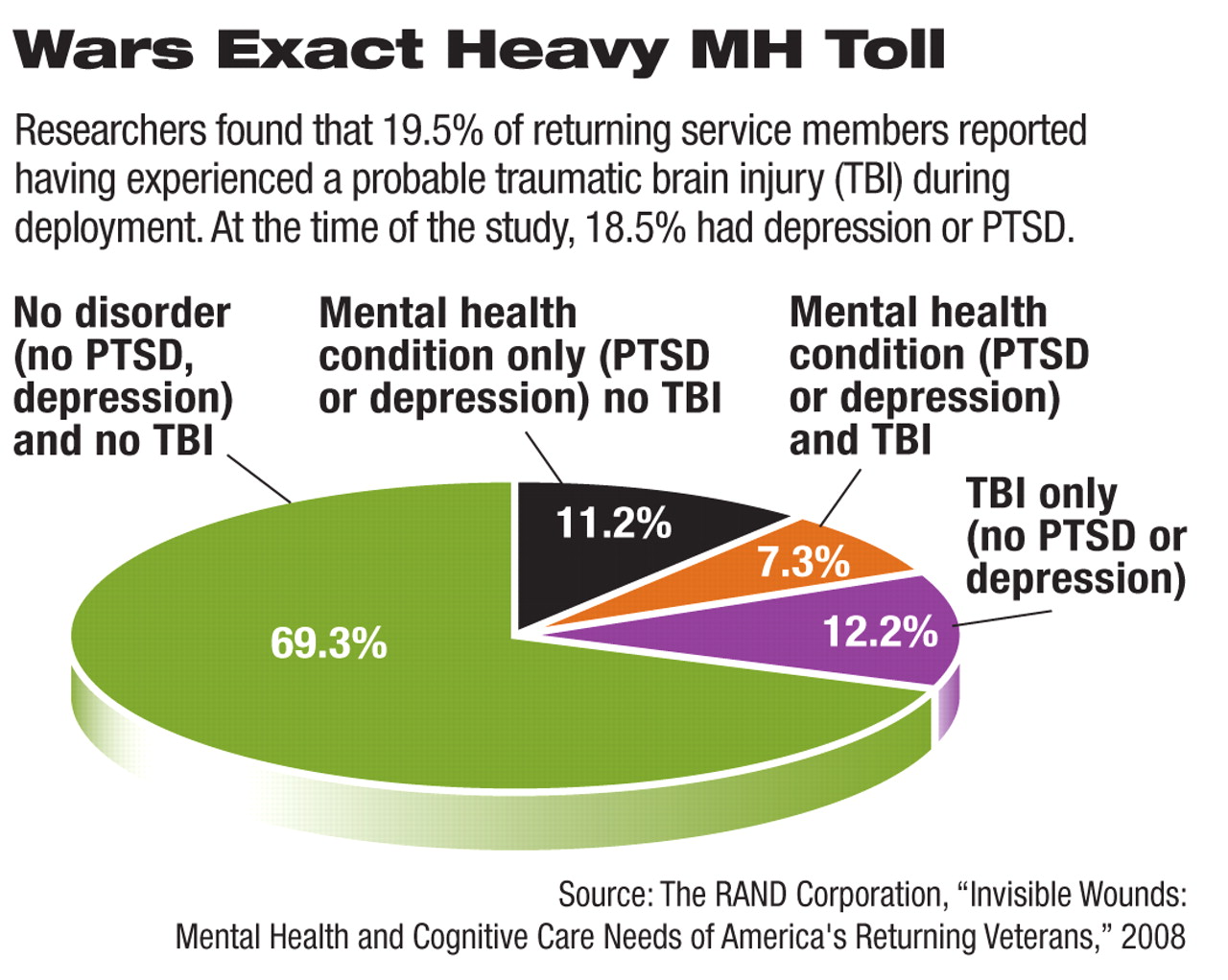
Approximately 18.5 percent of U.S. service members who have returned from Afghanistan and Iraq have posttraumatic stress disorder (PTSD) or depression. And about 19.5 percent report experiencing a traumatic brain injury (TBI) during deployment, according to a report by the RAND Corporation on the mental health and cognitive needs of service members returning from Iraq and Afghanistan.
The figures are based on a survey of 1,965 returning members of the military conducted from August 2007 through January 2008.
Assuming the prevalence of mental illness found in the study is representative of the 1.64 million service members who had been deployed in Iraq or Afghanistan as of October 2007, it means that approximately 300,000 individuals currently suffer from PTSD or major depression and that 320,000 individuals experienced a probable TBI during deployment.
About one-third of those previously deployed had at least one of these three conditions, and about 5 percent reported symptoms of all three, according to the report, “Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery.”
The 499-page report addresses a vast range of issues related to mental health in returning service members: illness prevalence; barriers to care, including military cultural barriers and structural barriers such as a shortage of clinicians and lack of availability of evidence-based treatments; cost to society; prevention of homelessness; unemployment; special issues related to women veterans and to families and children; and others.
The RAND study confirms findings of studies by the Army and Department of Defense revealing the enormous toll the wars are taking on the mental health of service members and their families, as well as the considerable barriers to treatment.
A report in the November 14, 2007, Journal of the American Medical Association found that Reserve and active-duty soldiers reported similar rates of potentially traumatic combat experiences (69.6 percent versus 66.5 percent), hospitalization during deployment (6.0 percent versus 5.3 percent), and overall mental health concerns on the Post-Deployment Health Assessment (17.5 percent versus 17.0 percent).
That assessment is given to all soldiers returning from deployment. However, by the time of the Post-Deployment Health Re-Assessment—which is given three to six months later—reserve soldiers reported substantially higher rates of interpersonal conflict, PTSD, depression, and overall mental health risk than did active-duty soldiers—35.5 percent versus 27.1 percent, respectively (Psychiatric News, December 7, 2007).
That JAMA report was a longitudinal descriptive study of 88,235 U.S. soldiers returning from Iraq who completed both the assessment and reassement with a median time of six months between the two. The study looked at soldiers returning between June 1, 2005, and December 31, 2006. It was conducted by researchers at the Division of Psychiatry and Neuroscience at Walter Reed Army Institute of Research and was funded by the U.S. Army Medical Research and Materiel Command.
Also, a survey by the U.S. Army's Fifth Mental Health Advisory Team (MHAT-V) of 2,295 soldiers in Iraq and 699 in Afghanistan found that about 18 percent of U.S. Army soldiers serving in Iraq screened positive for mental health problems; that figure rose to 27 percent for those on their third tour.
The data were collected in October and November 2007 (Psychiatric News, April 4).
Study Not Conducted by Military
Terri Tanielian, M.A., a co-author of the RAND report and co-director of RAND's Center for Military Health Policy Research, told Psychiatric News that it is the first study of mental illness among returning Iraq and Afghanistan service members conducted independently of the military. And whereas the JAMA study surveyed Army Reserve and National Guard soldiers, the RAND study looked at all service components, she said.
Moreover, the RAND survey offers a current picture of the mental health status of returning service members, Tenielian said.
“Yet even given that we have a different methodology and a broader scope, we have come up with rates that are generally consistent with other reports,” she said. “This is really a challenge for the entire U.S. health care system.”
Military psychiatrists agree that the RAND report confirms, and adds to, a body of literature testifying to a large burden of mental illness (see
Army Wants APIRE's Help on MH Care).
“The RAND data are very consistent with data we have found,” psychiatrist Col. Elspeth Cameron Ritchie, M.C., director of behavioral health for the U.S. Army Medical Command, told Psychiatric News.“ That's surprising because the way they gathered their data was different. One difference that is critically important is that the RAND study looked at costs to society of mental illness among service members. Those data support everything we have been saying about early intervention.”
The RAND report estimates that the cost of PTSD and major depression for two years after deployment ranges from $5,900 to $25,760 per case.“ Applying these percase estimates to the proportion of the entire population of 1.64 million deployed service members who are currently suffering from PTSD or depression, we estimate that the total societal costs of these conditions range from $4.0 to $6.2 billion, depending on whether the costs of lives lost to suicide are included,” according to the report.
The report estimates that the one-year cost for each case of mild TBI ranges from $27,260 to $32,760; estimates for the cost of each case of moderate to severe TBI range from $268,900 to $408,520.
Stigma Is Prominent
In addition to the survey of returning service members, the RAND study included a critical review of literature on the prevalence of PTSD, major depression, and TBI and their short- and long-term consequences. They also reviewed research on focus groups with military service members and their spouses and the development of a microsimulation model to forecast the economic costs of these conditions over time.
Interviews with senior staff in the Office of the Secretary of Defense, each branch of the military, and the Veterans Health Administration also informed the report.
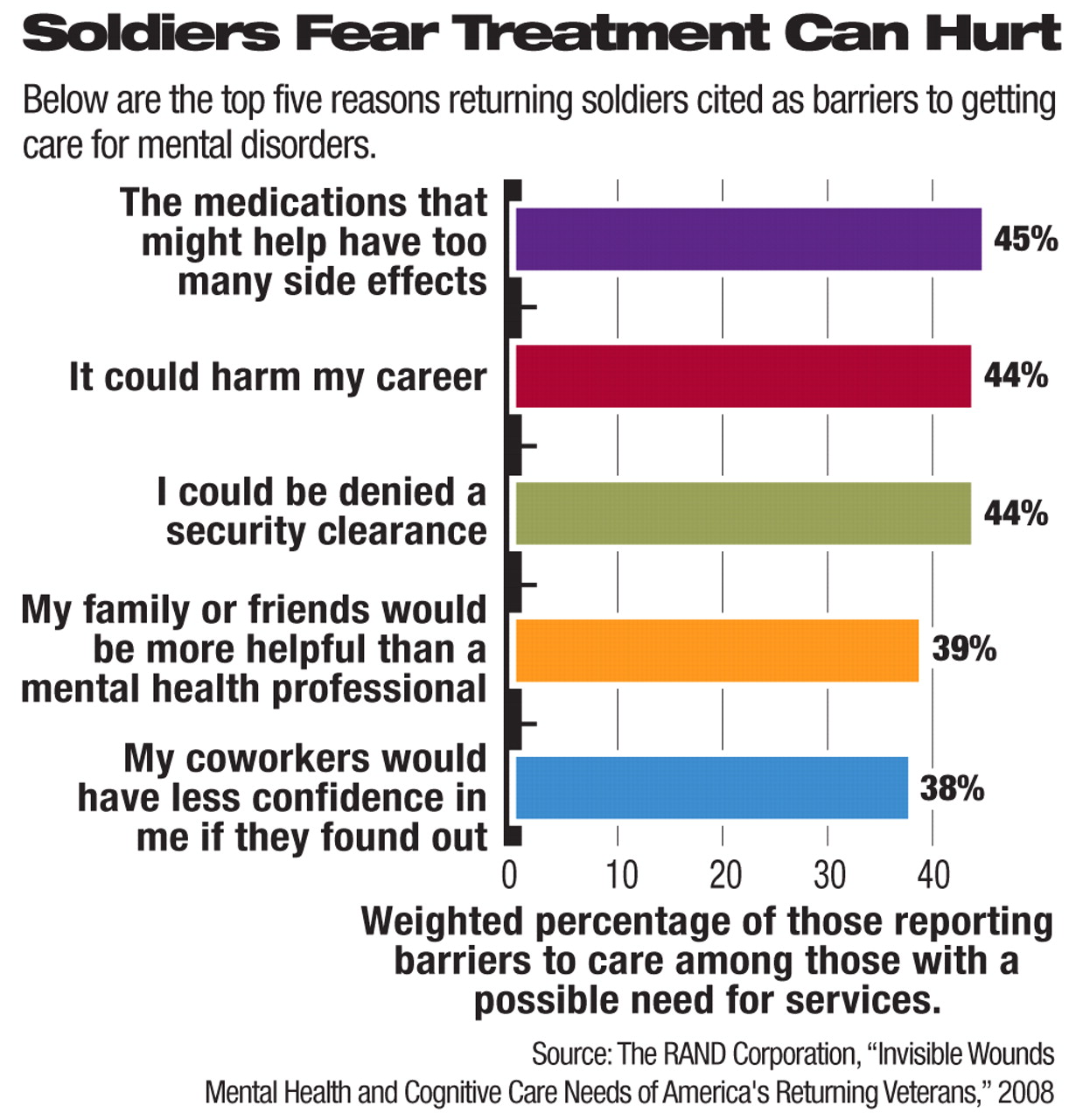
In addition to the wide prevalence of mental illness, the study found that stigma is a prominent barrier to seeking care, with many service members reporting fear about the negative consequences of using mental health services.
Of those reporting a probable TBI, 57 percent had not been evaluated by a physician for brain injury. Service members with probable PTSD or major depression sought care at about the same rate as did the civilian population, and, just as in the civilian population, many of these individuals were not receiving treatment. About half (53 percent) of those who met the criteria for current PTSD or major depression had sought help from a physician or mental health professional for a mental health problem in the preceding year.
Career Worries a Deterrent
Among those with a possible need for services, 44 percent said seeking treatment could harm their career, and a similar percentage said they feared being denied a security clearance. In addition, 38 percent said they feared that co-workers would have less confidence in them if it were known they had sought care (see chart).
Interestingly, 45 percent said they also feared that medications they might be prescribed would have too many side effects.
“This is an area that represents a real opportunity for education by psychiatrists and other clinicians treating returning veterans,” Tanielian said.
Ritchie emphasized the urgent need to increase the number of mental health clinicians serving military personnel and said that the Department of Defense is trying to hire civilian contract practitioners to treat active-duty personnel and returning veterans.
“We also realize that many soldiers go through their primary care doctor and never go near mental health,” she said. “So we are trying to enhance the ability of our primary care physicians to screen for and treat PTSD and depression.”
Then-APA President Carolyn Robinowitz, M.D., said the RAND report confirms the extraordinary public health challenge posed by returning service members in need of mental health care.
“We at APA have recognized this need and have made it a focus of our advocacy this spring,” she told Psychiatric News. “APA has endorsed Give an Hour, which encourages volunteer efforts by psychiatrists throughout the nation to provide services to returning service personnel and their families, and we have encouraged our members to participate” (Psychiatric News, March 7).
Robinowitz said she herself signed on to volunteer and planned to become active after her presidential term was over.
She added that APA has surveyed members about the low reimbursements and heavy administrative burden associated with TRICARE. More information on the results of that survey will appear in the next issue.
“My sense is that psychiatrists are not so concerned about the reimbursement but about the administrative burden,” Robinowitz said.“ I am hoping that our leadership can speak with leadership in the Department of Defense to address these concerns.”
She also said APA is encouraging psychiatrists to become participants in TRICARE, as she is doing now. “These returning servicemen and servicewomen are suffering, as are many of their families; they deserve access to the care they need,” she said. “These young people put themselves in harm's way, and we owe it to them” to treat them and their families.
Finally, Robinowitz said that the RAND report echoes others on the topic in underscoring the impact of stigma—particularly that service personnel perceive that admitting to mental health problems may cause one's military career to stall in spite of efforts on the part of military leaders to encourage seeking care when needed.
“The military leadership is working so hard on this,” she said.“ But it's clear there is a prevailing negative mythology that has diminished in the general public but hasn't cleared up in the military.”
Robinowitz said that what may be necessary is public and personal endorsement of the value of mental health treatment by senior military leaders and veterans, similar to the kinds of public statements that have been made by civilian celebrities.
Documents related to the RAND report can be accessed at<www.rand.org/multi/military/veterans/>. An abstract of “Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning From the Iraq War” is posted at<http://jama.ama-assn.org/cgi/content/abstract/298/18/2141>. A redacted version of the “Mental Health Advisory Team V” report is posted at<www.armymedicine.army.mil/news/mhat/mhat_v/MHAT_V_OIFandOEF-Redacted.pdf>. The Department of Defense has posted resources for soldiers, veterans, and their families at<www.battlemind.org> and<www.behavioralhealth.army.mil>. APA has done so as well at<HealthyMinds.org>. Information about Give an Hour is posted at<www.giveanhour.org>.▪