Scientists have identified a single genetic variant that seems to contribute not only to smokers' nicotine addiction, but to their risk of developing lung cancer.
This is the first time that a single genetic variant has been identified that seems capable of doing both, Nora Volkow, M.D., director of the National Institute on Drug Abuse, said in a press statement.
The findings come from four scientific teams headed by laura Jean Bierut, M.D., a professor of psychiatry at Washington University in St. Louis; Kari Stefansson, Ph.D., chief executive officer of deCODE Genetics, a biopharmaceutical company in Reykjavik, Iceland; Christopher Amos, Ph.D., a professor of epidemiology at the M.D. Anderson Cancer Center in Houston; and Paul Brennan, Ph.D., of the International Agency for Research on Cancer in Lyon, France.
The results from Bierut and her team were posted online in AJP in Advance on May 15 and will be published in the print edition of the American Journal of Psychiatry in September. The results from Stefansson and his team and from Brennan and his were published in the April 3 Nature. The findings from Amos and his group were posted online on April 2 in Nature Genetics.
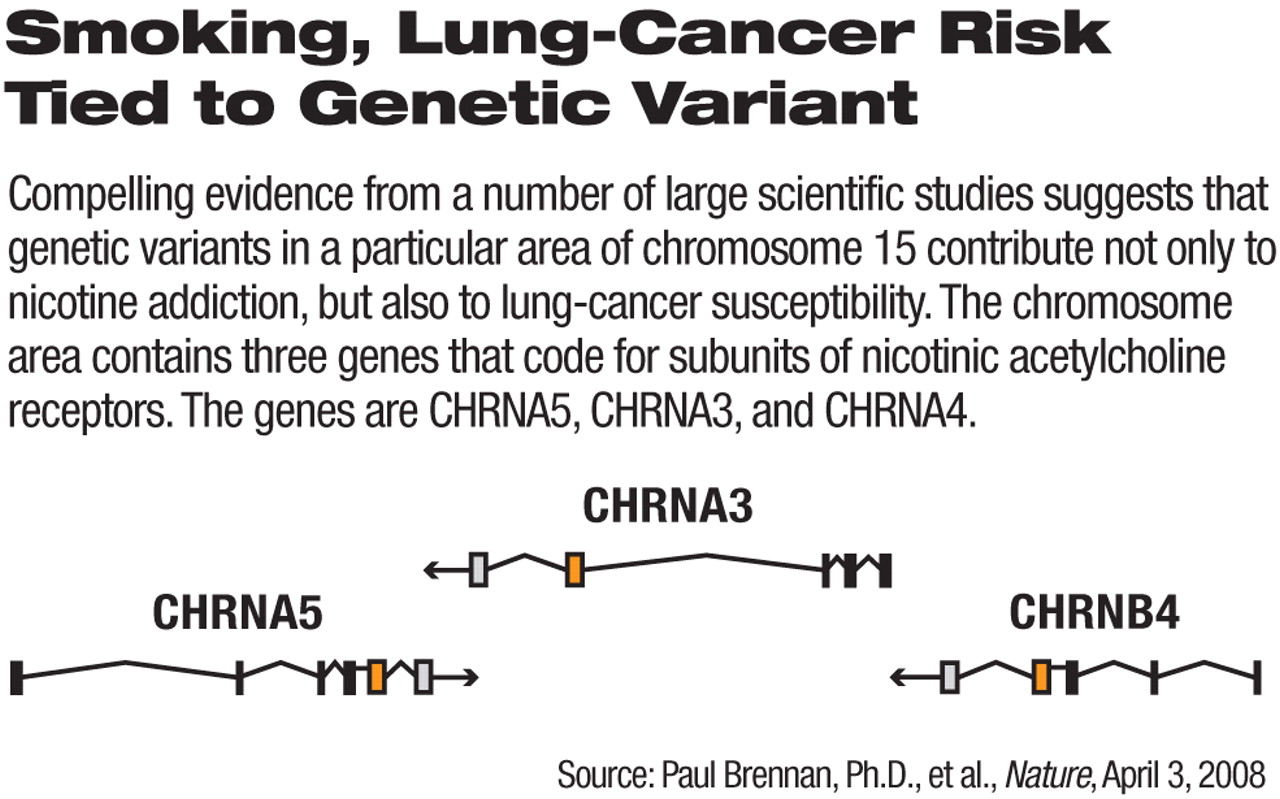
The genetic variant that all four groups have linked with nicotine addiction and lung cancer is located in a cluster of three genes on chromosome 15 that code for subunits of nicotinic acetylcholine receptors. The genes are CHRNA5, CHRNA3, and CHRNB4—or in short, the alpha 5-alpha 3-beta 4 nicotinic receptor gene cluster. The suspect genetic variant is called rs1051730.
After comparing genetic material from nonsmokers, light smokers, and heavy smokers—altogether some 2,000 subjects—Bierut and her colleagues found a highly significant link between rs1051730 and nicotine addiction. Stefansson and his coworkers found the same by comparing genetic material from light, medium, and heavy smokers—altogether some 14,000 smokers.
Then Stefansson and his team, Amos and his, and Brennan and his found a highly significant link between rs1051730 and lung cancer. Stefansson's group obtained this result by comparing genetic material from some 1,000 lung-cancer patients with that from some 32,000 controls. Amos's team obtained this result by comparing genetic material from some 1,000 smokers with lung cancer with that from some 1,000 smokers without it. And Brennan's group obtained this result by comparing genetic material from about 2,000 lung-cancer subjects and controls.
These findings, Volkow said, point to “potential targets for new smoking-cessation medications that may be more effective at helping smokers to quit.”
The findings also suggest that smokers might be screened for the genetic variant rs1051730, Amos told Psychiatric News, and if found to have it, might then be screened regularly for early signs of lung cancer. In fact, Brennan and his team stated in their report that drugs targeted to the protein made by genetic variant rs1051730 might be able to prevent lung cancer.
Meanwhile another nicotinic acetylcholine receptor story has been unfolding for some time. It concerns the alpha 7 nicotinic acetylcholine receptor. Schizophrenia patients are known to have a fewer-than-normal number of such receptors, and this deficiency seems to be responsible for some of their neurocognitive deficits. Moreover, schizophrenia patients tend to be heavy smokers, which might be a way of self-medicating their neurocognitive deficits. Indeed, nicotine has been found to improve neurocognition, especially concentration, in schizophrenia patients (Psychiatric News, December 30, 2002; July 21, 2006; December 1, 2006). So Psychiatric News asked Amos whether the above findings might have implications for schizophrenia patients.
The gene for the alpha 7 receptor is located on a different region of chromosome 15 than is the alpha 5-alpha 3-beta 4 nicotinic receptor gene group, Amos said. “So I don't know that our findings have any relevance to schizophrenia patients. [On the other hand] it is interesting that schizophrenia patients have been reported to smoke very heavily and yet have low lung-cancer risks.”
The study by Bierut and her team was funded by the National Institutes of Health. The study by Stefansson and colleagues was funded by deCODE Genetics, the National Institute on Drug Abuse, and the European Commission. The study by Amos and colleagues was funded by the National Institutes of Health, the M.D. Anderson Cancer Center, the Flight Attendants Medical Research Institute, and the Center for Inherited Disease Research. The study by Brennan and coworkers was funded by INCa France, the National Cancer Institute, and the Ontario Institute for Cancer Research.
“Nicotine Dependence and the Alpha 5-Alpha 3-Beta 4 Nicotinic Receptor Gene Cluster” can be accessed at<http://ajp.psychiatryonline.org/pap.dtl>. An abstract of “A Variant Associated With Nicotine Dependence, Lung Cancer, and Peripheral Arterial Disease” is posted at<www.nature.com/nature/journal/v452/n7187/abs/nature06846.html>. An abstract of “Genome-Wide Association Scan of Tag SNPs Identifies a Susceptibility Locus for Lung Cancer at 15q25.1” is posted at<www.nature.com/ng/journal/v40/n5/index.html>. An abstract of “A Susceptibility Locus for Lung Cancer Maps to Nicotinic Acetylcholine Receptor Subunit Genes on 15q25” is posted at<www.nature.com/nature/journal/v452/n7187/abs/nature06885.html>.▪