In the two years after the Canadian regulatory agency issued a warning about the use of antidepressants in children and adolescents, researchers have found a decrease in medical treatment for depression in children, adolescents, and young adults and a parallel increase in the rate of completed suicides among children and adolescents, according to a study in the April 8 Canadian Medical Association Journal.
Laurence Katz, M.D., an associate professor of psychiatry at the University of Manitoba in Winnipeg and a pediatric psychiatrist, and colleagues extracted medical and prescription data on nearly 3 million youth who were covered by the universal health care system in Manitoba from April 1, 1995, to March 31, 2006. In addition, they obtained data on completed suicides during this period in the province from several sources.
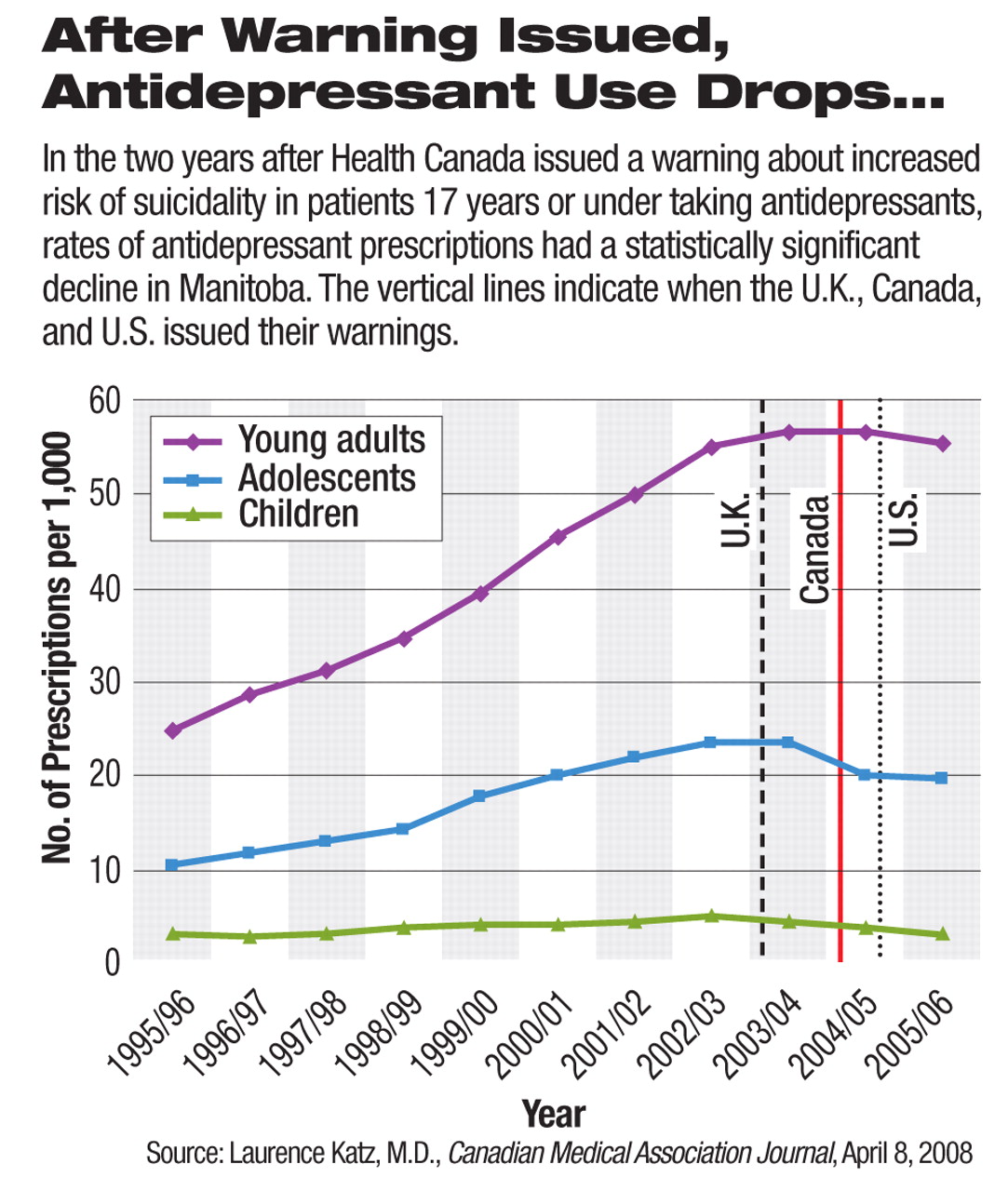
The researchers used May 31, 2004, as the cutoff date to compare depression treatment trends in the nine years before and two years after Health Canada issued a warning to health professionals and the public about increased risk of suicidal thoughts and behaviors associated with “newer antidepressants.” The agency specifically named selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) as the drugs of concern.
The number of antidepressant prescriptions per year per 1,000 individuals decreased significantly for children (5 to 11 years old) and adolescents (12 to 17 years old) as well as for young adults (19 to 24 years old). Those aged 18 were excluded by the authors in the analysis so they could better determine whether there was a clear difference between young adults and the 17-and-under population. The trends were not significantly different.
The trend in medical services for depression treatment also saw a decline after the regulatory warning about antidepressants. The rate of depression-related physician visits decreased significantly for children, adolescents, and young adults. The authors expressed concerns that “in an environment where the treatment of a life-threatening disorder has become more complicated, vulnerable patients are receiving less care.”
“People went to the doctor less often for the treatment of depression,” Katz told Psychiatric News. He pointed out that the study found no signs of increased alternative treatment for depression in place of reduced antidepressant prescriptions, which implied patients' reluctance to seek a physician's diagnosis and assessment for depression.
“The warning's effect was not only seen in physicians' practice, but also the public's attitude... .With fewer visits to physicians, people are deprived of all kinds of treatment,” he commented.
Katz emphasized that their study results are limited to a temporal association between the widely publicized regulatory warning and a decline in depression treatment including medications and physician visits. A causal relationship cannot be established from the observations alone, however.
“What we are most concerned about is how this information was disseminated from the regulatory review to the public and potential unintended effects afterward,” he said. The media attention devoted to the connection between antidepressants and increased suicide risk around 2003 and 2004 was as intense in Canada as it was in the United States, he noted, which may have contributed to fear of depression treatment in patients and their families and the decreased number of depression-related visits.
In Canada, psychotherapy provided by a physician is covered by the government's universal health care system. Psychotherapy provided by psychologists is usually covered by supplemental private insurance. Therefore, Canadians face few financial barriers to physician-provided psychotherapy compared with Americans.
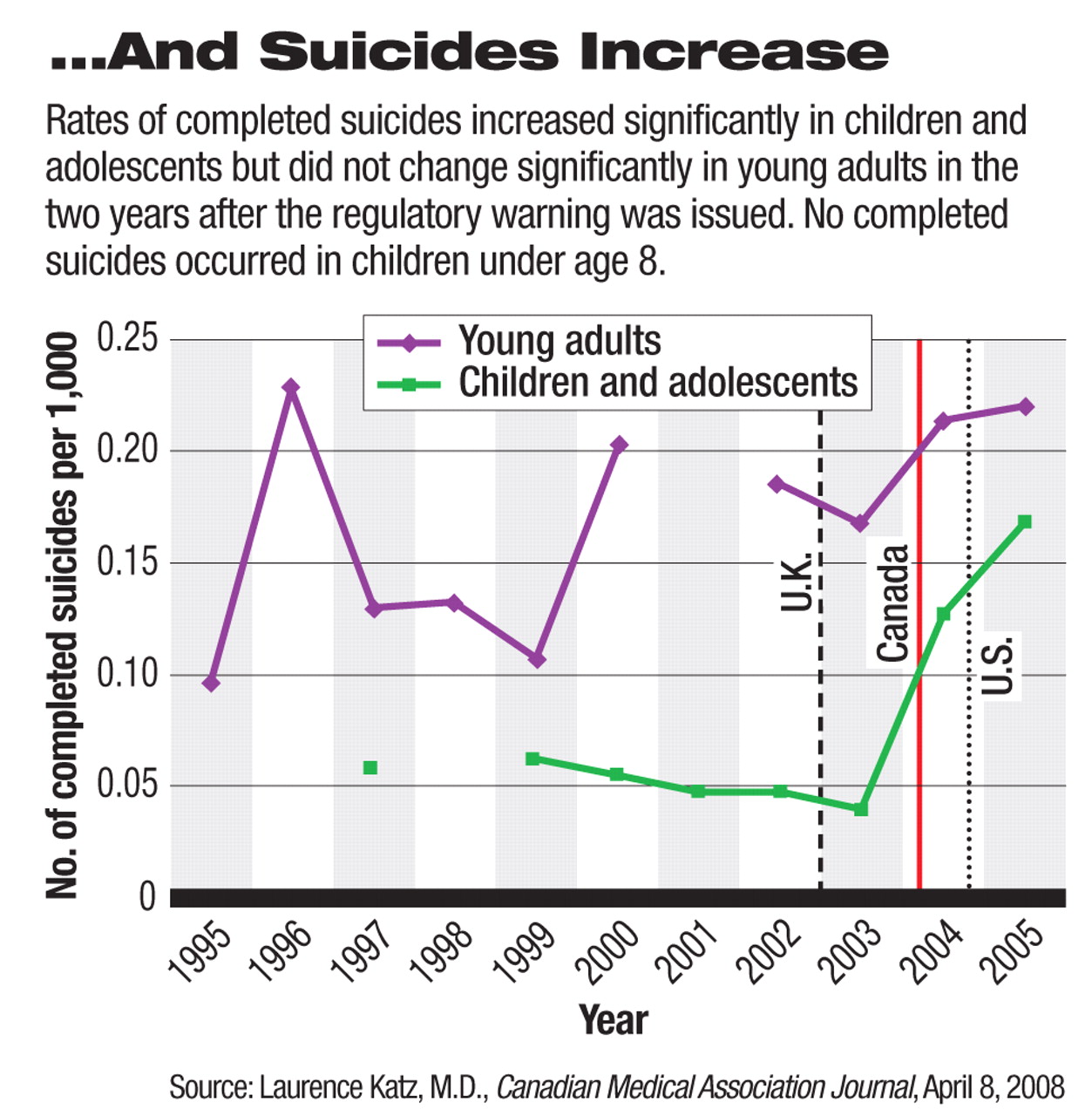
During the same period of declining physician visits and prescriptions for depression, the rate of completed suicides saw a statistically significant increase in children and adolescents aged 17 and younger, from 0.04 a year per 1,000 individuals before the Health Canada warning to 0.15 a year per 1,000 after the warning. The rate of completed suicides in young adults (19 to 24 years) was not statistically significantly changed. A total of 99 children and adolescents and 136 young adults completed suicide between 1995 and 2005 in Manitoba.
“These findings from Canada are quite similar to findings in the United States and the Netherlands based on our previous work and the work of others,” Robert Gibbons, Ph.D., director of the Center for Health Statistics at the University of Illinois, told Psychiatric News. He and his colleagues published a study in the American Journal of Psychiatry in 2007 that observed similar reductions in the number of antidepressant prescriptions as well as a rise in suicide rates that were consistent with the Canadian study's results during roughly the same period. He pointed out that other studies also identified decreased diagnosis and treatment of depression in youth and adults following the U.S. Food and Drug Administration's black-box warning about the risk of increased suicidality (Psychiatric News, September 7, 2007).
In this Canadian study, the authors found that only 10 percent of the children and adolescents who completed suicide had received an antidepressant prescription in the nine years before Health Canada's warning in June 2004. In the first year and second year after the warning, 10.5 percent and 4 percent of those who completed suicide had received an antidepressant prescription, respectively. The authors' statistics indicated that these rates were not statistically different from each other, however.
The warning issued by Health Canada and mandated wording in antidepressant labels differ substantially from that issued by the U.S. Food and Drug Administration (FDA). The FDA revised the black-box warning in prescription labels in 2007 to state that patients up to 24 years old are at risk of suicidal thoughts and behaviors, but there is no evidence of increased risk in adults older than 24. The agency requires all antidepressants, including the older tricyclic drugs, to carry this warning. Health Canada, in contrast, applies the warning to patients of all ages and specifically to SSRIs and SNRIs. It also requires drug labels and patient-information sheets to describe the increased risks of “agitation and hostility or anxiety, or. .impulsive or disturbing thoughts that could involve self-harm or harm to others” after a patient initiates antidepressant therapy.
“The way this information has been disseminated can be confusing for many physicians and patients,” Katz said.
This study was funded by a grant from the Health Sciences Centre Foundation, a Canadian Research Chair Award, and Canadian Institutes for Health Research New Investigator Award.
An abstract of “Effect of Regulatory Warnings on Antidepressant Prescription Rates, Use of Health Services, and Outcomes Among Children, Adolescents, and Young Adults” is posted at<www.cmaj.ca/cgi/content/full/178/8/1005>.▪