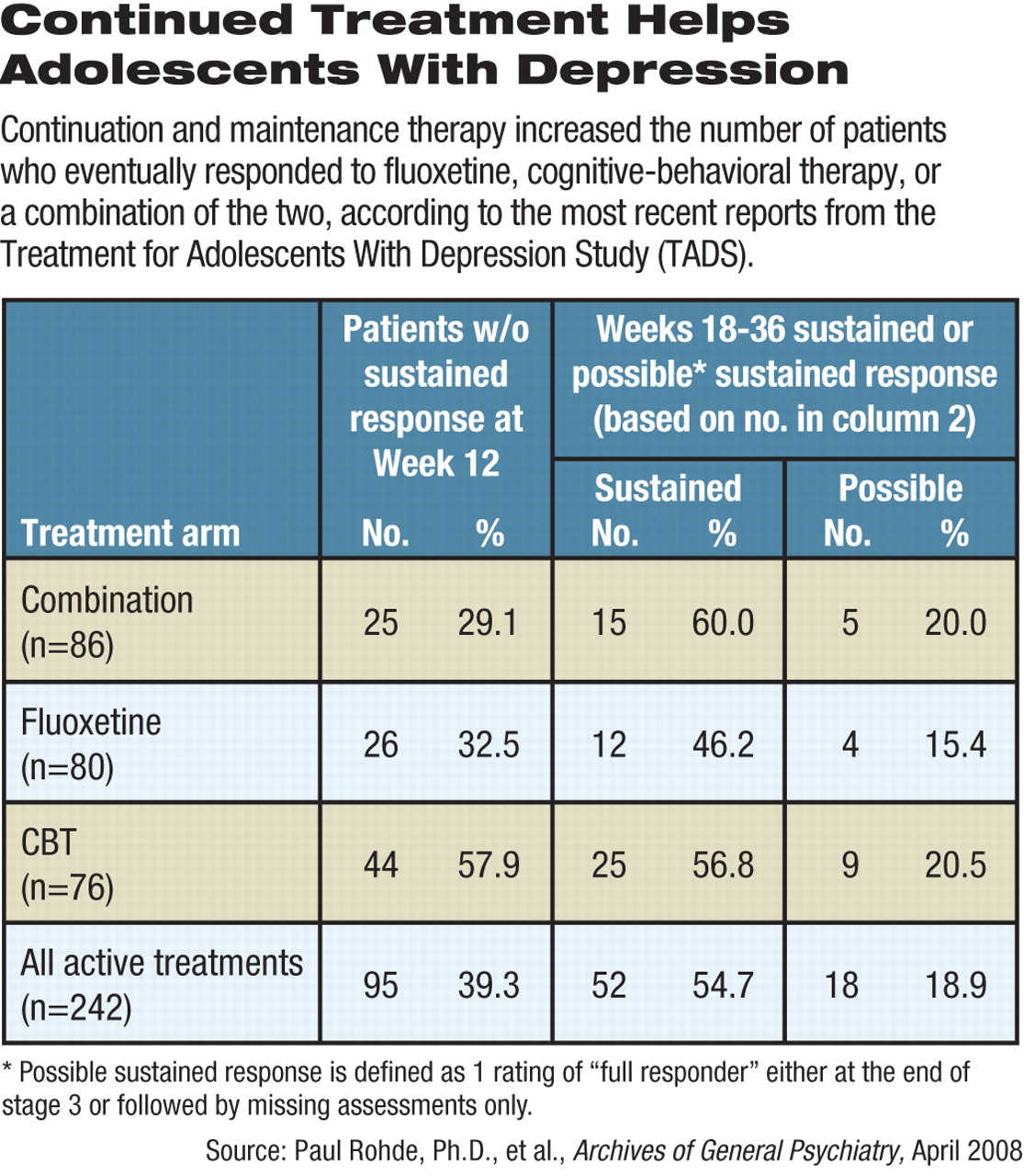
Most patients who achieved a sustained response to treatment in the first 12 weeks of the Treatment for Adolescents With Depression Study (TADS) maintained their gains at 36 weeks, while over half of those who did not achieve a sustained response at 12 weeks did so with further treatment, according to the investigators' latest report.
Response was measured on the Clinical Global Impression-Improvement (CGI-I) scale. Two consecutive ratings of 1 or 2 on the scale were considered a sustained response.
The study adds further evidence to the value of longer-term treatment and to the use of cognitive-behavioral therapy (CBT) added to or in combination with an SSRI antidepressant (Psychiatric News, November 2, 2007).
In the trial's first three months, patients treated with fluoxetine alone or in combination with CBT fared significantly better than those on CBT monotherapy. However, at the end of 36 weeks, rates of sustained response to fluoxetine alone, CBT alone, and combination therapy were about the same. Thus, CBT appeared to take longer to achieve similar levels of efficacy, compared with the other treatment conditions.
“These findings emphasize the value of ongoing treatment in facilitating the depression recovery process,” wrote clinical psychologist Paul Rohde, Ph.D., senior research scientist at the Oregon Research Institute in Eugene, and colleagues in the April Archives of General Psychiatry. “Approximately three-quarters of adolescents with depression who have not fully responded after 12 weeks of acute treatment will experience sustained response with further treatment.”
TADS was funded by the National Institute of Mental Health.
“This study adds some evidence to what we know from the overall TADS study and the efficacy of fluoxetine,” David Mrazek, M.D., told Psychiatric News. “It supports current practice—that medicine works, and that medicine in the context of a therapeutic relationship works even better.”
Mrazek, who was not involved with the TADS study, is chair of the Department of Psychiatry and Psychology at the Mayo Clinic and a professor of psychiatry at the Mayo Medical School in Rochester, Minn. He is also chair of APA's Council on Children, Adolescents, and Their Families.
The results are also a reminder that treatment of adolescents for depression can be a laborious process, Rohde told Psychiatric News.
“Clinicians have to educate patients and their parents that treatment is effective but that it takes time to work,” he said.
Researchers did not include patients randomized to placebo in the first 12 weeks of TADS. They tallied data for the 242 cases remaining in active treatment arms at the start of stage 2. Patients continued on the same regimen they used in the trial's first phase. Full responders were maintained at doses of fluoxetine up to 40 mg/day, while partial responders had doses raised to 50 mg/day or 60 mg/day.
In stage 1, patients getting CBT received 15 sessions. In stage 2 (12 to 18 weeks), full responders in stage 1 got CBT every two weeks, while partial responders received once-a-week therapy. During the third stage (18 to 36 weeks), patients saw a therapist at six-week intervals for three CBT booster sessions.
Full responders received CGI-I scores of 1 (“very much improved”) or 2 (“much improved”), while partial responders had scores of 3 (“minimally improved”). All others were ranked as nonresponders.
About 82 percent, or 121, of the 147 patients with a sustained response at the end of 12 weeks maintained that status through 36 weeks. While fewer patients on CBT alone achieved full response by 12 weeks, the effect proved highly durable. About 94 percent (30 out of 32) maintained their status, compared with 70 percent of those on fluoxetine alone and 87 percent on combination therapy. Rohde and his colleagues make no recommendations from this finding, except to note that it is “promising and warrants further investigation” in light of the small cohort involved.
The relatively poor showing of CBT in the first 12 weeks may not reflect on the treatment itself, said Rohde. “It might have been unrealistic to expect that 12 weeks of treatment would be adequate,” he said. “If these patients were treated for, say, 16 weeks, the results for CBT might have been better.”
Many of the 95 patients without a sustained response in the first phase of the trial did achieve a sustained response by 36 weeks. These included 56.8 percent of those originally on CBT, 46.2 percent of those on fluoxetine, and 60 percent of those on combination therapy. The differences were not statistically significant, according to the researchers.
The study gives some encouragement to continue treatment even if results don't appear right away, said Mrazek. “It tells people who use CBT that if it does work, it will tend to continue to work, and that's reassuring.”
However, maintaining consistency in the application of CBT across different settings might be difficult, said Mrazek.
“It might be highly variable even at one site,” he said.“ Fluoxetine can be prescribed in reproducible doses, but therapists and adolescents differ.”
TADS recruited patients during 2000 to 2003. The researchers followed their patients for a full year after the end of the 36-week active treatment trial and will eventually report on how the effects of treatment persisted, said Rohde.
Grants from the National Institute of Mental Health and the National Institute on Drug Abuse will also allow them to track their subjects for five years to record functional outcomes as they transition to college, young adulthood, and the workplace