A scene from the 1991 film “Grand Canyon” finds two young working women commiserating over the stress and anxiety in their lives.
“Do you ever feel like you're just this far from being completely hysterical?” the first woman asks, holding her thumb and forefinger a hair's length apart.
The other woman replies, “Half the people I know feel that way.... They are the lucky ones.... The rest of the people are hysterical.”
This fictional dialogue is, of course, hyperbole. But a studied look at the country's emotional health was on display at APA's 2008 annual meeting in May via a research poster shown by scientists from the Centers for Disease Control and Prevention (CDC).
Frequent mental distress (FMD)—as self-reported in the agency's survey of more than 2 million U.S. adults—has increased in over half the country since the early 1990s. FMD, the poster explained, is a nonspecific CDC construct that aims to capture at a specific moment in time how many of the previous 30 days the mental health of a noninstitutionalized adult aged 18 or older was not good. The term “mental distress” was defined as having “stress, depression, and problems with emotions.”
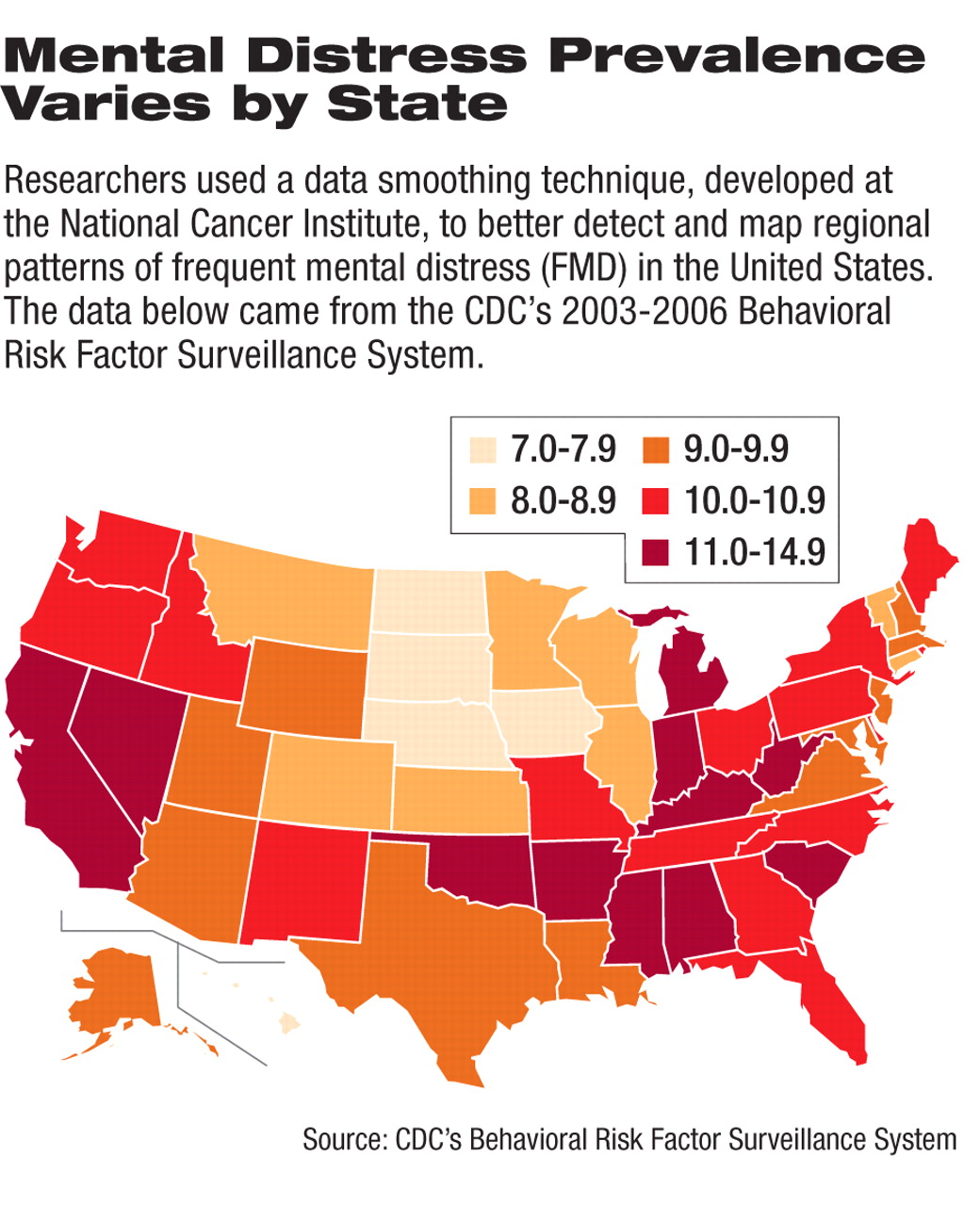
According to the poster, when the researchers compared geographic patterns of FMD by state across two time periods (1993-2001 and 2003-2006), they found“ areas of consistently high and low FMD, as well as changes in [some] states.” More than 1.2 million adults were surveyed over each study period.
“The overall prevalence of FMD for the combined period was 9.4 percent,” the researchers reported. During the 2003-2006 period, the prevalence of FMD rose by 1 or more percentage points in 27 states from the levels reported in the earlier study period, 1993-2001. The 2003-2006 FMD in 23 states and the District of Columbia remained within a percentage point of the 1993-2001 FMD prevalence. The 2003-2006 FMD increased by 3 percent or more in Oklahoma, Mississippi, and West Virginia from the 1993-2001 levels.
Over the two study periods, the states that showed the highest prevalence of FMD were Kentucky (14 percent), West Virginia (11.2 percent), Nevada (10.9 percent), Alabama (10.8 percent), and Mississippi (10.8 percent), while the states that showed the lowest prevalence were Hawaii (6.6 percent), South Dakota (6.7 percent), Washington, D.C. (7.4 percent), Kansas (7.5 percent), and Nebraska (7.5 percent). The average spread between the five highest-prevalence states and five lowest-prevalence states grew from 4 percent to 5.9 percent.
The researchers found that in general the prevalence of FMD was higher in California and Nevada and the Appalachian and Mississippi Valley regions of the country, and lower (or diminishing) in the upper Midwest.
“Just as we are seeing obesity and other physical health problems as rising public health concerns, we should also see the rising prevalence of frequent mental distress as a public health concern,” Daniel Chapman, Ph.D., a psychiatric epidemiologist and one of the four authors of the CDC poster, told Psychiatric News.
The data studied by Chapman and his colleagues, led by David Moriarty, B.S., came from the CDC's Behavioral Risk Factor Surveillance System. It is the largest continuing, state-by-state telephone survey, typically reaching more than a million U.S. adults aged 18 and older in a given study period. Interviews are conducted 12 months a year—every year—by state health departments in all 50 states, the District of Columbia, and three U.S. territories (Puerto Rico, the U.S. Virgin Islands, and Guam). CDC analyzes the collected data annually (on a calendar-year basis).
Since early 1984, the survey has tracked the health of the population based on answers given by participants about their disease status, their disease-prevention and safety-oriented behaviors, and their high-risk, unhealthy behaviors and activities.
The number of individuals completing the surveys in the two study periods ranged from a low of 98,619 in 1993 to a high of 334,606 in 2006. Those surveyed in both study periods (totaling 2.5 million individuals) were asked a series of validated, health-related, quality-of-life questions. As one example related to mental health, one of the questions asked each respondent to estimate if “for 14 or more days out of the previous 30 days you felt your mental health—including stress, depression, and problems with emotions—was not good.”
The results of this question were analyzed and mapped by state to track the self-perceived FMD across the country (see accompanying map).
Chapman said that the finding most striking to him and his colleagues wasn't the expected though slight rise in FMD in New York and the Washington, D.C., metropolitan area following September 11, 2001. Rather, “There appears to be some patterns of relatedness between FMD and the 'stroke belt,'” said Chapman. “That's a geographical area in the U.S. that roughly follows the Mississippi Valley and Appalachian mountain range. That's because there appears to be a higher prevalence of stroke in those regions,” he said, drawing on federal reports and academic studies.“ However,” Chapman noted, “the etiologic parallels of FMD and the stroke belt are strictly speculative at this point.”
According to the literature, one of the most difficult health statistics to nail down is the prevalence of “mental disorders,” given the breadth and complexity and sheer number of disorders inherent in that single term. Thus, most rates are typically estimates, and they can vary widely.
Chapman acknowledged this and said the weakness of the study is the construct of FMD, which they used to define the prevalence. FMD, he said, is a nonspecific measure that is self-reported; thus it relies on the subjective perceptions of the survey respondents without benefit of independent validation via medical and psychiatric assessments.
Even so, Chapman noted that “surveillance of FMD can be useful in identifying [geographical] regions characterized by unmet needs and disparities, targeting interventions, and evaluating programmatic interventions over time.”