A 12-week course of continuous treatment with buprenorphine-naloxone and counseling is more effective than conventional detoxification and counseling in treating youth for opioid addiction, a randomized clinical trial has found.
From July 2003 to December 2005, 152 youth aged 15 to 21 who received outpatient addiction treatment at six programs (four methadone programs and two substance treatment programs for adolescents) were randomly assigned to two groups: One group underwent outpatient detoxification for two weeks, with a maximum dose of 14 mg/day buprenorphine (n=78); the other group received buprenorphine-naloxone with a maximum buprenorphine dose of 24 mg/day for five to seven days a week for 12 weeks (n=74).
All patients met DSM-IV criteria for opioid dependence with physiological features. In addition to the medication treatment, every participant was provided with weekly counseling, including one individual session and one group session a week, for the 12-week period.
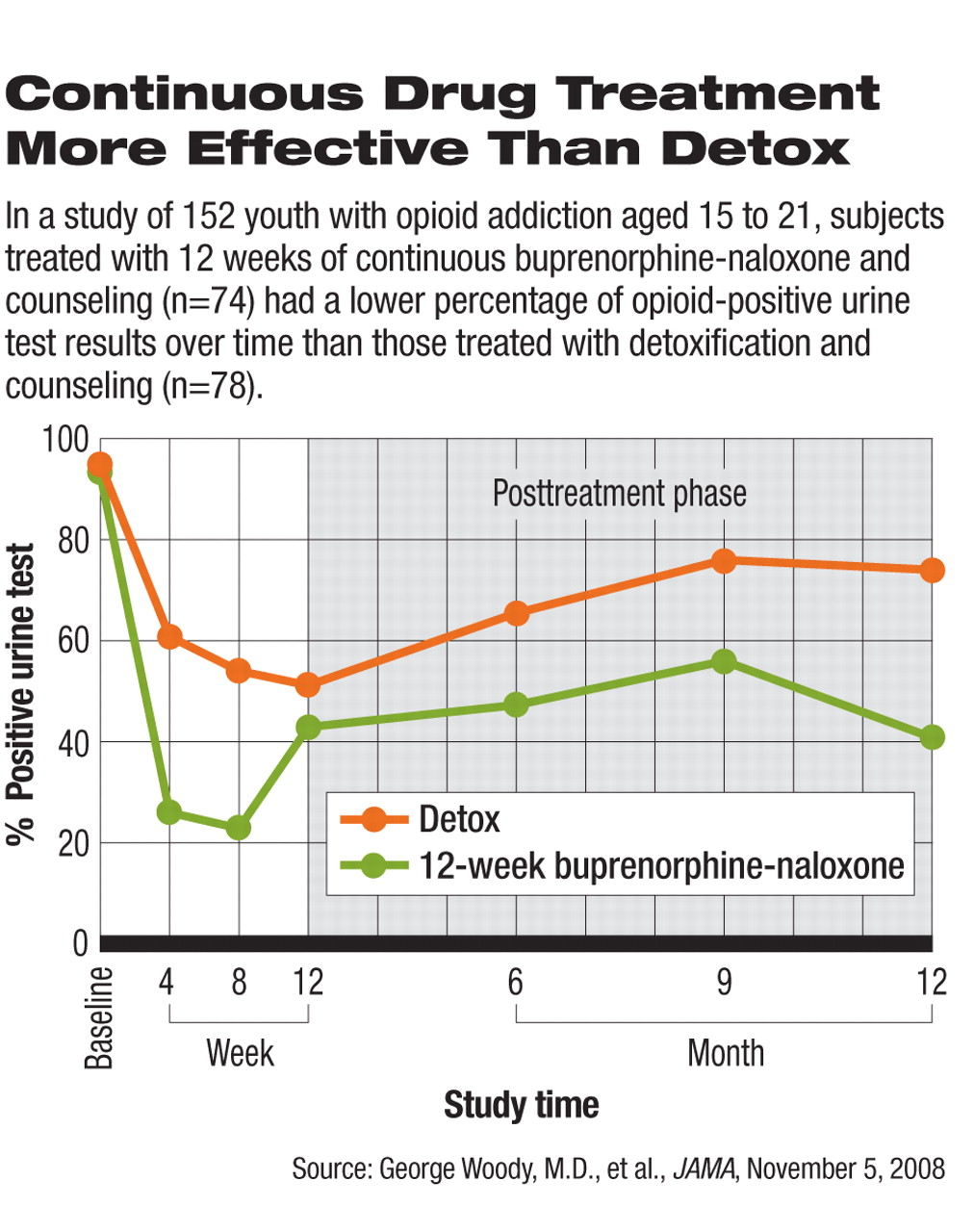
At week 4, 61 percent of patients in the detoxification group and 26 percent of patients in the 12-week-treatment group tested positive for opioids (see chart). By week 8, 54 percent in the detoxification group and 23 percent in the 12-week-treatment group had opioid-positive urine tests. The difference was statistically significant at both time points. At week 12, the percentage of patients who tested positive was 51 percent in the detox group and 43 percent in the 12-week treatment group; the difference was not significantly different.
In an interview with Psychiatric News, the study's lead author George Woody, M.D., a professor of psychiatry at the University of Pennsylvania and the Treatment Research Institute in Philadelphia, explained that the lack of statistical significance at week 12 may be attributable to the fact that the dosage of buprenorphine-naltrexone was tapered off from week 9 to week 12.
The 12-week buprenorphine-naloxone treatment group had a much higher retention rate than did the outpatient detox group. By the end of week 12, 15 of the detox patients (20.5 percent) were still in treatment, compared with 52 (70 percent) in the 12-week-treatment group.
In addition to the primary endpoints, self-reported opioid use, marijuana use, self-injection behavior, and enrollment in other addiction treatments were all significantly more common in the detoxification group than the 12-week-treatment group. At six, nine, and 12 months, patients in the detox group continued to have significantly higher proportions of positive urine test results than those in the 12-week-treatment group.
No serious adverse events related to buprenorphine-naloxone were reported in the study, and no one was removed from the study because of adverse events.
The study results suggest that clinicians “should not be in a hurry to take patients off the medication just because they are young and have not been addicted for a long time,” according to Woody.
“These data can help change the current guidelines,” he said. For underage patients with opioid addiction, “the field has been primarily using psychosocial treatment alone following detoxification,” he noted. “The study shows that you can improve results if you are willing to use medications in outpatient treatment. And that can be lifesaving.”
The study results were published in the November 5 Journal of the American Medical Association. The research was funded by the National Institute on Drug Abuse. The manufacturer of buprenorphine-naloxone (Suboxone), Reckitt Benckiser, provided the medication for the study.
An abstract of “Extended vs. Short-term Buprenorphine-Naloxone for Treatment of Opioid-Addicted Youth: A Randomized Trial” is posted at<jama.ama-assn.org/cgi/content/abstract/300/17/2003>.▪