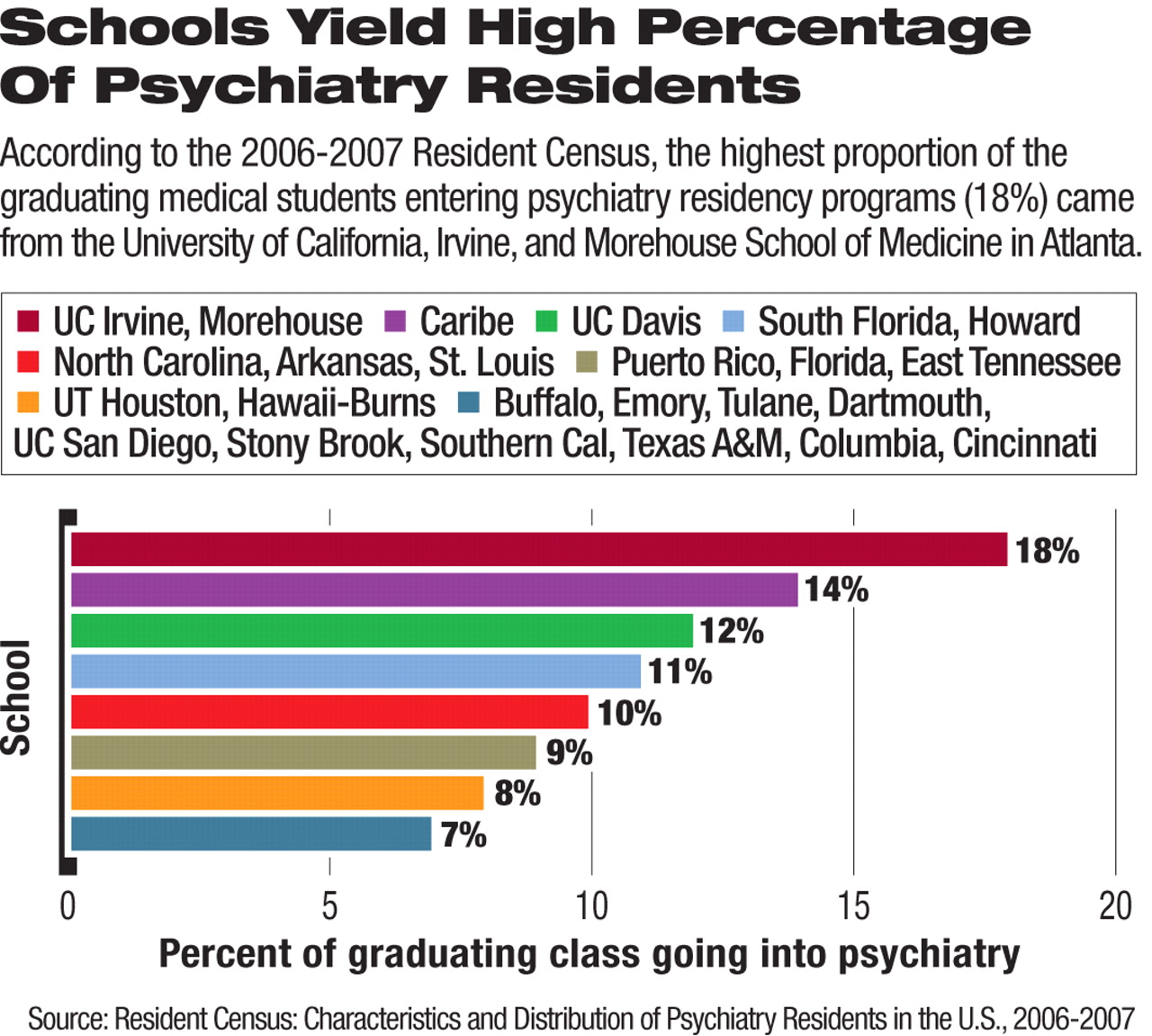
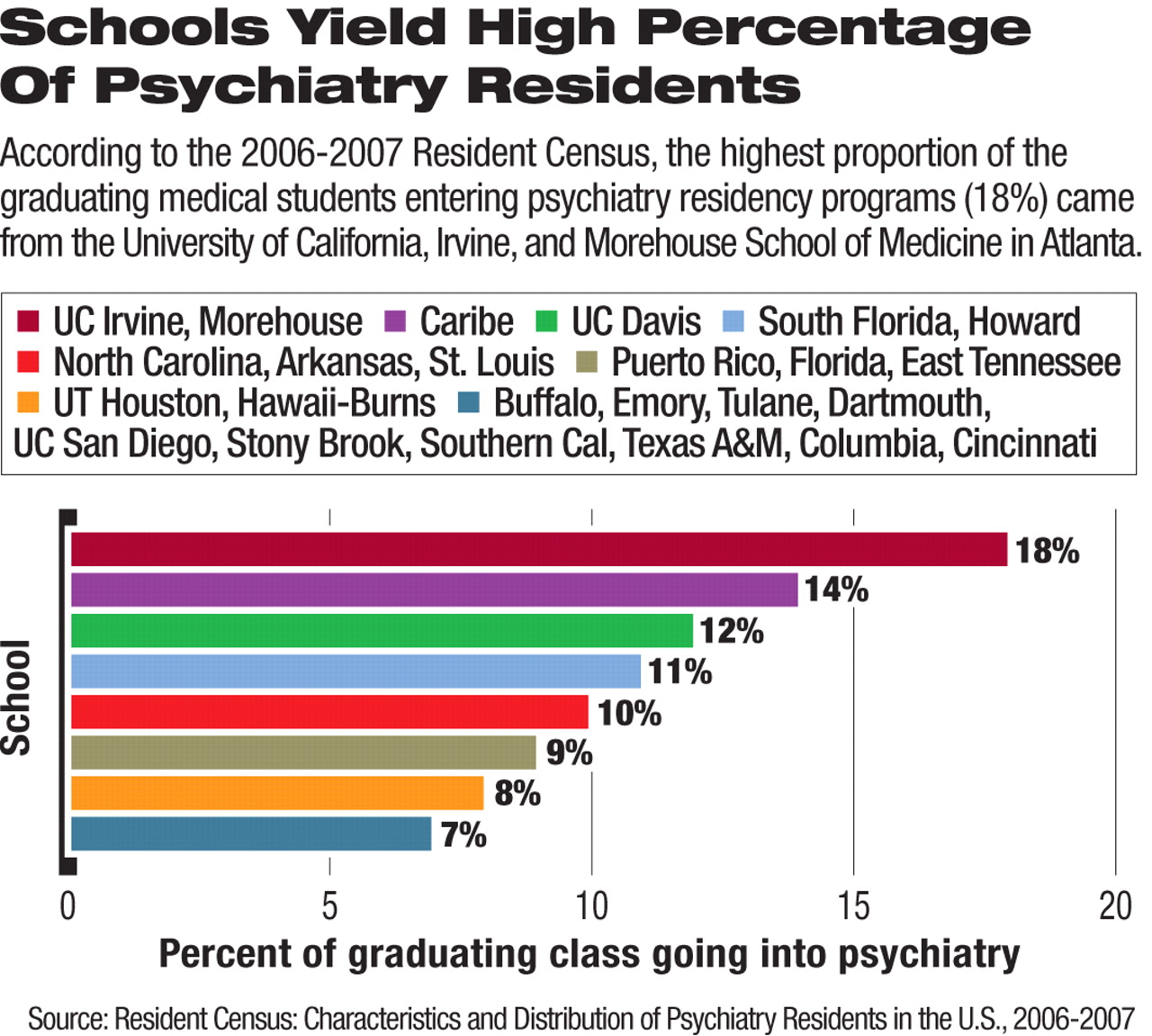
The practice of psychiatry affords a broad array of enriching professional opportunities and a unique chance to get to know patients one on one. This is part of the message imparted to medical students at the University of California, Irvine (UCI), where last year, 18 percent of graduating medical school students entered psychiatry residency programs in the United States, according to the 2006-07 Resident Census (see also
Morehouse Aims to Diversify Psychiatric Workforce.) The Association of American Medical Colleges and the AMA conduct the Resident Census each year. APA's Office of Graduate and Undergraduate Education compiles the information on psychiatry residents for the census.
“At UCI, we show medical students that psychiatrists are physicians first,” said Gerald Maguire, M.D., senior associate dean for educational affairs at the UCI School of Medicine, in an interview with Psychiatric News. He noted that he thinks psychiatry has become separated from the field of medicine in some students' minds. “We show medical students that with the tools they will acquire as psychiatry residents, they can be better physicians for their patients.”
He credits a balanced experience in psychiatry during medical school. This enables students to understand that both medications and psychotherapy are essential for treating patients with mental illness.
During the six-week psychiatry clerkship, students work with patients in inpatient and outpatient settings and on different services, including consultation, child and adolescent, and adult units. UCI Medical Center includes a 65-bed, inpatient psychiatric facility where medical students work closely with residents treating patients.
Medical students also work with veterans through the Long Beach-va Health System and the County of Orange Health Care Agency, which provides community mental health services.
They also get the opportunity to become involved in community advocacy work, Maguire noted, due to the psychiatry department's links to local branches of national mental health advocacy organizations such as the National Alliance on Mental Illness and Mental Health America. In addition, there is a psychiatry interest group for medical students in which they are exposed to issues in different areas of psychiatry.
Faculty psychiatrists are also actively involved in a retreat held for all medical students during their first year, Maguire said. During the retreat, patients who are recovering from mental illness speak to the students about their experiences.
“The students realize that you can have a linear conversation with someone who is hearing voices” and get to know the person beyond their symptoms, he said.
In addition to being inspired by dedicated psychiatry faculty who participate in clinical rotations and didactics, Maguire said, the students work closely with UCI psychiatry residents. The psychiatry residents are required to complete four months of nonpsychiatric training, during which they may work on internal medicine or emergency medicine rotations as part of the treatment team. Thus the students are exposed to psychiatry residents in different capacities.
Maguire said that many medical students yearn to work in a field in which they can spend time with patients without feeling rushed and can “see that they are making a difference in patients' lives.” With advancements in treatments the students have the opportunity to do just that, he said.
Residents Play Key Role
Charles Nguyen, M.D., the UCI Irvine psychiatry residency training director, commended the residents' teaching skills and noted that they work carefully with medical students to help them understand the science of evaluation, diagnosis, and treatment, so they can appreciate what psychiatrists do on a daily basis.
When Nguyen teaches medical students, he encourages them to become invested in the patients' outcomes by spending time getting to know patients and their families. For instance, medical students may verify a patient's history with family and sit down to educate families about the symptoms of mental illness and how treatment will help.
“Medical students are included as part of the treatment team,” Nguyen said. “They see that they can make a difference in the patients' lives.”
PGY-4 psychiatry resident Visant Sanathara, M.D., told Psychiatric News that he and his fellow residents have a certain degree of freedom in terms of what they teach the medical students. For instance, he noted,“ not only do I get to teach [the students] clinical tips I have acquired along the way, but I also emphasize the administrative facets of medicine,” he said.
Such issues may include health care costs, billing systems, and the organization of health care systems—issues that are sometimes overlooked in other medical school curricula, Sanathara noted. “Teaching allows me to supplement their educational experiences with real-world principles beyond what is learned in the classrooms and wards,” he said.
Faculty Members 'Invested' in Teaching
According to Barry Chaitin, M.D., chair of the UCI Department of Psychiatry, medical students have consistently bestowed teaching awards on psychiatry faculty members (including Maguire). Not only do the small medical school classes (about 100 students each year) facilitate more interaction between students and psychiatry faculty, but the faculty members also work hard to maintain a strong presence in the medical school curriculum.
Barton Blinder, M.D., a representative to the APA assembly from the Orange County Psychiatric Society and a clinical professor of psychiatry at UCI, emphasized that medical students pick up on the way they are valued by psychiatry faculty members.
He and others in the department have mentored not only medical students, but also undergraduates who are majoring in psychology and related fields.
He added that any medical school with a psychiatry department that places great value on getting medical students involved in all aspects of psychiatric treatment can expect favorable recruitment rates for psychiatry residency programs. ▪