A recent survey of clinicians, including psychiatrists, in Nebraska has directly connected the Food and Drug Administration's (FDA's) warning on antidepressants to their reluctance to prescribe antidepressants to treat children and adolescents with depression.
Although several studies based on prescription databases have recorded flat or declining trends in antidepressant use after the FDA issued its black-box warning about increased risk of suicidal thoughts and behaviors in children and adolescents, these data could not establish a causal relationship or clear association for the decline. Supriya Bhatia, a fourth-year medical student and faculty members at the University of Nebraska Medical Center (UNMC), conducted a survey of physicians and other prescribing clinicians, including nurse practitioners and physician assistants. The survey was mailed in July 2005, less than a year after the black-box warning was issued, to 1,521 prescribing clinicians in Nebraska based on the clinician database in the Health Professionals Tracking Center at UNMC and other supplemental sources. A total of 866 clinicians responded, resulting in a response rate of 57.5 percent. Among the survey respondents were 122 psychiatric clinicians, 139 pediatric clinicians, and 605 family medicine clinicians who practiced in various clinical settings in both urban and rural areas of Nebraska. Almost all (97 percent) of the respondents said they were aware of the warning.
The psychiatric clinicians included 65 general psychiatrists, 20 child and adolescent psychiatrists, and 37 residents, specialized nurse practitioners, and physician assistants.
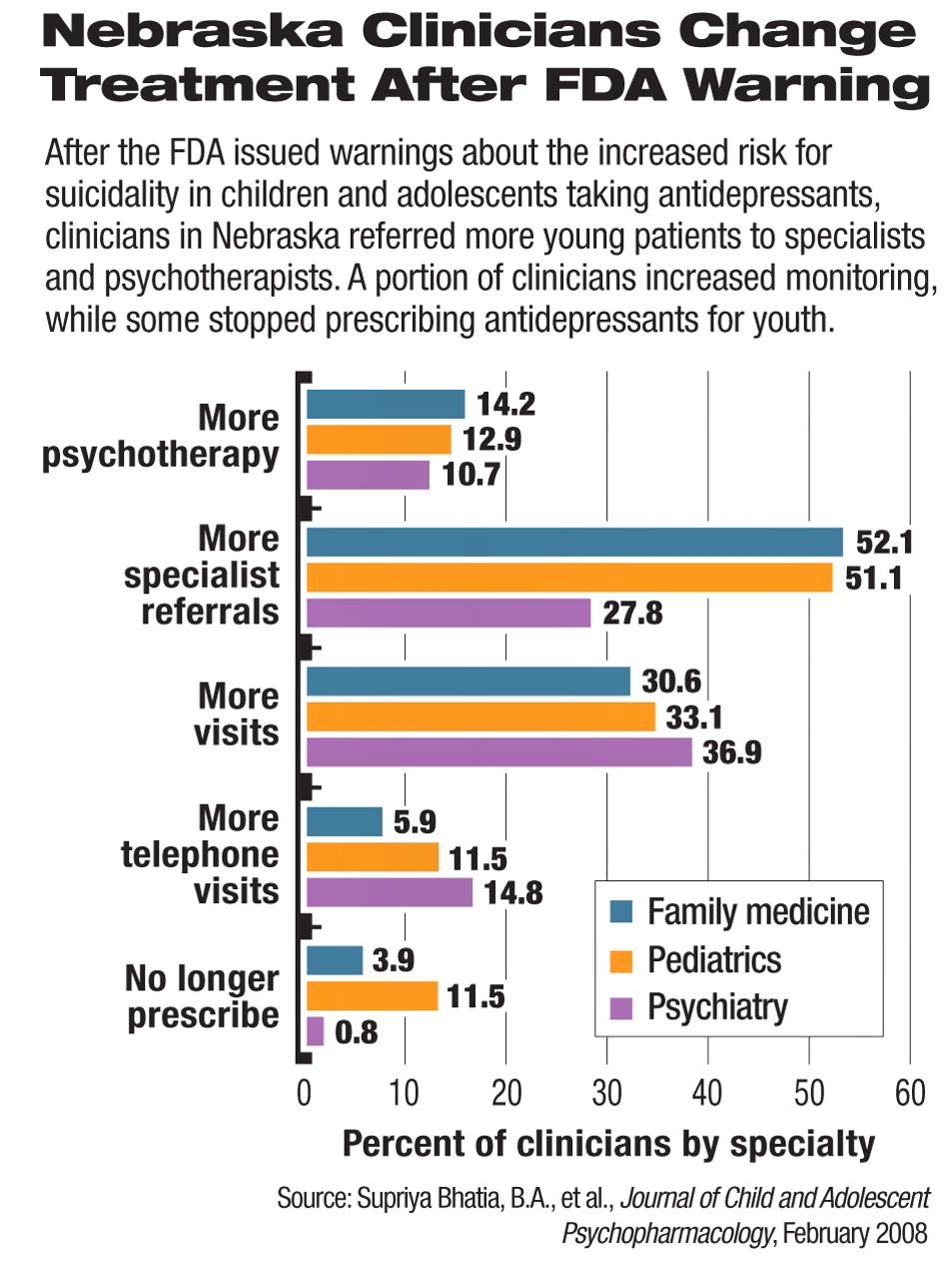
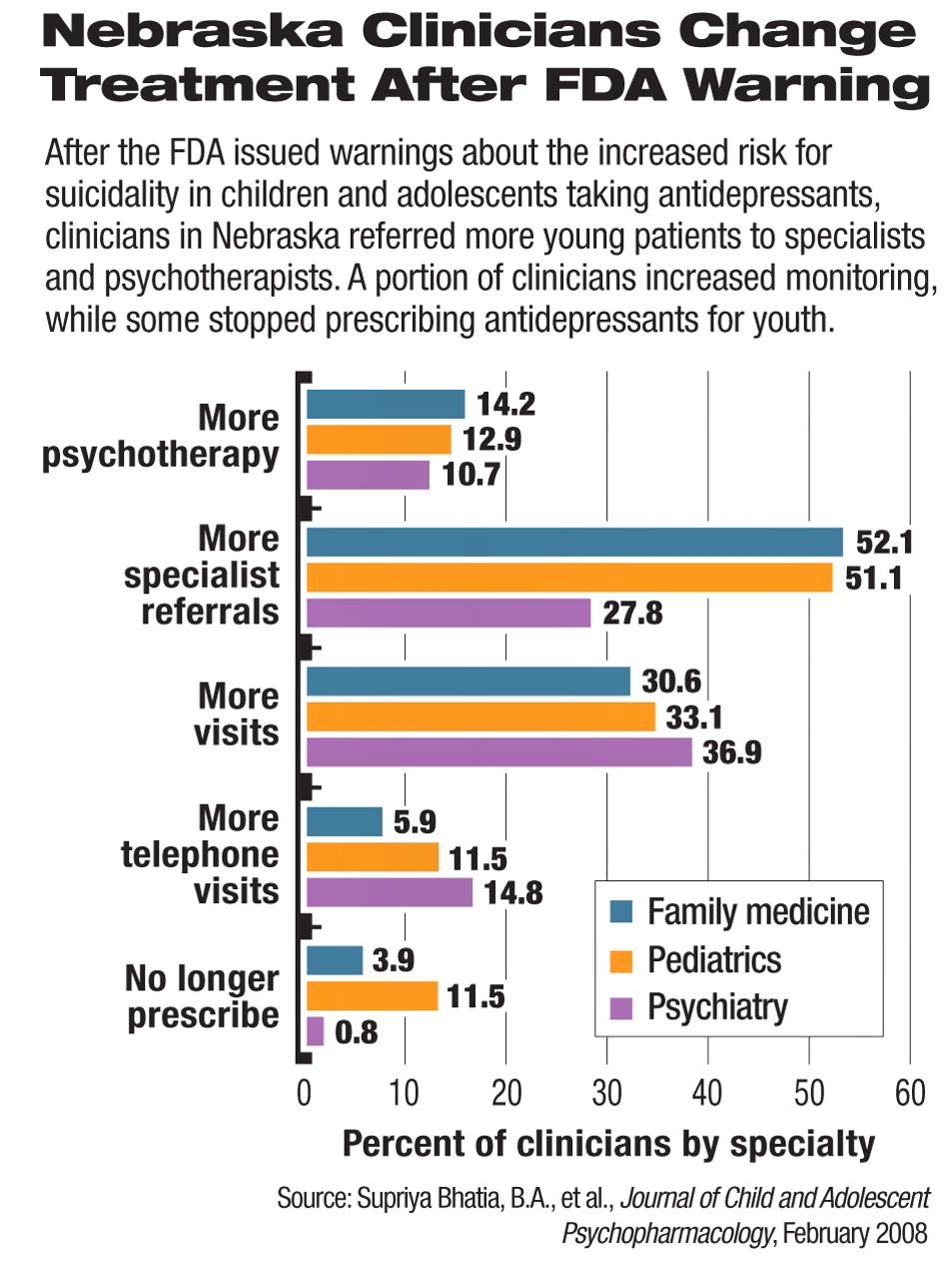
Before the FDA warning, 80 percent of the responding clinicians in family medicine, 69 percent of responding pediatric clinicians, and 71 percent of responding psychiatric clinicians reported that they were prescribing antidepressants to children and adolescents. After the black-box warning, 16 percent of the respondents said they decreased prescribing antidepressants for children, and 37 percent said they decreased prescribing for adolescents. About 5 percent stopped prescribing antidepressants for young patients.
“We found it a bit startling that so many clinicians just stopped treating child and adolescent depression altogether or decreased treatment after the warning,” said Bhatia, the study's first author, in an interview with Psychiatric News.
About half (49 percent) of the respondents said they were “moderately comfortable” or “comfortable” in prescribing antidepressants to children and adolescents; 8 percent said they felt “very comfortable.”
In response to the black-box warning, half of the clinicians in family and pediatric medicine said they began to refer more young patients to specialists such as psychiatrists, psychologists, and clinical social workers, for treatment of depression.
About 32 percent of respondents, or 276 clinicians, reported more frequent contacts, either by telephone or in office, with young patients upon initiating antidepressant treatment after the black-box warning. The survey did not ask clinicians why they did not see patients more often or follow the FDA's recommendation of weekly follow-up. Bhatia suggested that limited access to care—especially in rural areas of Nebraska—lack of insurance reimbursement, and patients' lack of resources are possible factors for the phenomenon.
“Despite widespread knowledge of the black-box warning, only 7.5 percent of the clinicians responding to the survey reported following the initial FDA guidance of weekly monitoring throughout the first month after initiating treatment with an antidepressant,” Christopher Kratochvil, M.D., an associate professor of psychiatry at the UNMC and the senior author of the study, commented to Psychiatric News. The FDA later removed this monitoring guideline from antidepressant labeling.
More than 20 percent of the respondents said they had encountered at least one caregiver or patient who had refused an antidepressant prescription because of the much-publicized black-box warning.
“[Our survey] highlights the importance of patient and parent education, accompanied by open discussion, in order to facilitate adherence, safety, and optimal patient care,” said Kratochvil. “It is essential that the patient, parents, and clinician work together as a team in treating depression in children and adolescents.”
The survey was funded in part by the Spurlock Minority Medical Student Fellowship of the American Academy of Child and Adolescent Psychiatry.
Both authors pointed out that this survey has tackled a new perspective in the unresolved question regarding the effect of the FDA's black-box warning on treatment for children and young adults with major depression.
“There have been a lot of published data from insurance claims data and national trends, but we were able to get clinicians' response on a more personal basis,” said Bhatia. She and her colleagues were“ pleasantly surprised” by the 58 percent response rate to this mailed survey.
“Antidepressant Prescribing Practices for the Treatment of Children and Adolescents” is posted at<www.liebertonline.com/doi/pdfplus/10.1089/cap.2007.0049>.▪