Patient safety rose in prominence in American medical thinking with the publication a decade ago of “To Err Is Human,” the Institute of Medicine's (IOM) report estimating that tens of thousands of people die every year in American hospitals due to preventable medical errors.
Now APA has published a 33-page handbook that addresses ways to develop and integrate systems to reduce or prevent six critical events: suicide, aggression, falls, elopement, medical comorbidities, and drug or medication errors. Each chapter provides examples of unsafe care along with discussions of what went wrong and how to prevent mistakes.
The publication is an APA resource document prepared by the Committee on Patient Safety and approved by the Council on Quality Care and the Joint Reference Committee in June 2008. It can be downloaded free from the Web site at<
http://psych.org/safemd>.
“We wanted to place the idea of patient safety directly in the hands of working psychiatrists,” said Alfred Herzog, M.D., medical director of the professional programs at Hartford Hospital in Connecticut, in an interview. Herzog was co-editor of the publication with Geetha Jayaram, M.D., M.B.A., an associate professor of psychiatry at the Johns Hopkins Hospital and in its Department of Health Policy and Management.
“It had to be practical, useful, concise, and readily available,” said Herzog.
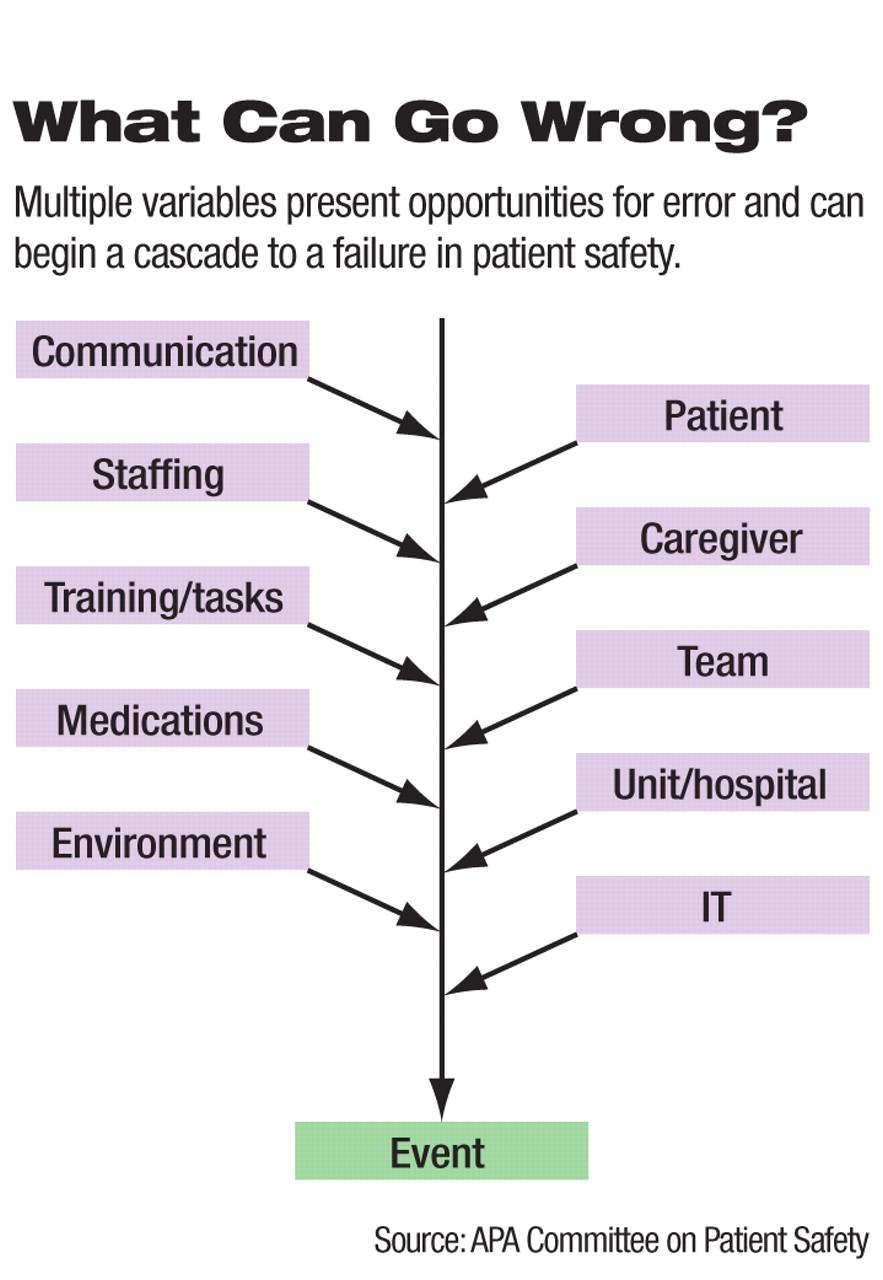
Like the rest of the patient-safety movement, the APA handbook emphasizes a shift away from blaming medical professionals for mistakes and toward creating systems that produce safe practices, wrote the editors.
“The likelihood that an individual will commit an error is far greater in systems that are poorly organized and that have weak procedures and regulations,” they said. “A good staff member cannot combat a bad system.”
The systemic approach has produced progress since the IOM report came out, said patient-safety expert Lucian Leape, M.D., an adjunct professor of health policy in the Department of Health Policy and Management at the Harvard School of Public Health. Leape was a member of the IOM panel that produced the original report.
“There's been a tremendous increase in activity, concern, and action and a real improvement in safety,” said Leape, in an interview.“ The most important new development is the movement away from procedural guidance to teamwork and relationships. This is hard for doctors, because they train as individuals, not as team members.
The mistakes in medical specialties where practice involves more procedures, preventing egregious errors like operating on the wrong leg have been addressed with such protocols. Not surprisingly, the pattern is different in psychiatry. True, a medication error is a medication error. Messy handwriting or an added or missing zero on a prescription can confuse a physician, pharmacist, nurse, or patient.
“Patient safety in psychiatry is more of a cognitive-awareness process than a procedural process,” said Herzog. “The psychiatrist must ask, 'What information do I need, and what steps do I take to assume safety with this patient?' The human interaction is critical.”
Psychiatry may be less procedurally oriented than orthopedic surgery but can still benefit from many of these safety ideas, said Leape. A patient using several medications at once must be carefully managed to avoid interactions or overmedication. Psychiatrists, even those who do not work primarily in hospitals, are often part of treatment teams. In the course of treating one patient, they may interact with psychologists, social workers, internists, members of patients' families, as well as patients themselves.
Safety in psychiatry also means doing things more than once—constantly reassessing risks while interacting with the patient, said Herzog. “Making sure you minimize risk is more difficult with psychiatric patients.”
The APA handbook uses patient vignettes delineating cases in which existing safeguards failed. The text discusses each case briefly, analyzing the failures, while adjacent tables list risk or protective factors, and summarizes steps needed to minimize that particular danger.
The document draws on existing knowledge, said Herzog. “This is not intended as original research, but rather serves as a summarizing and integrating resource.”
If one thread runs through the document, it is communication. Psychiatrists need to communicate closely and continuously with other members of the treating team, as well as with patients and their families, as Leape suggested.
“SAFE MD: Practical Applications and Approaches to Safe Psychiatric Practice” is posted at<http://psych.org/safemd>.▪