Clinicians who treat patients with generalized anxiety disorder or panic disorder should assess patients for symptoms of irritable bowel syndrome (IBS), according to the authors of a recent study headed by Daniel Gros, Ph.D., an assistant professor of psychiatry at the Medical University of South Carolina. It is in press with the Journal of Anxiety Disorders.
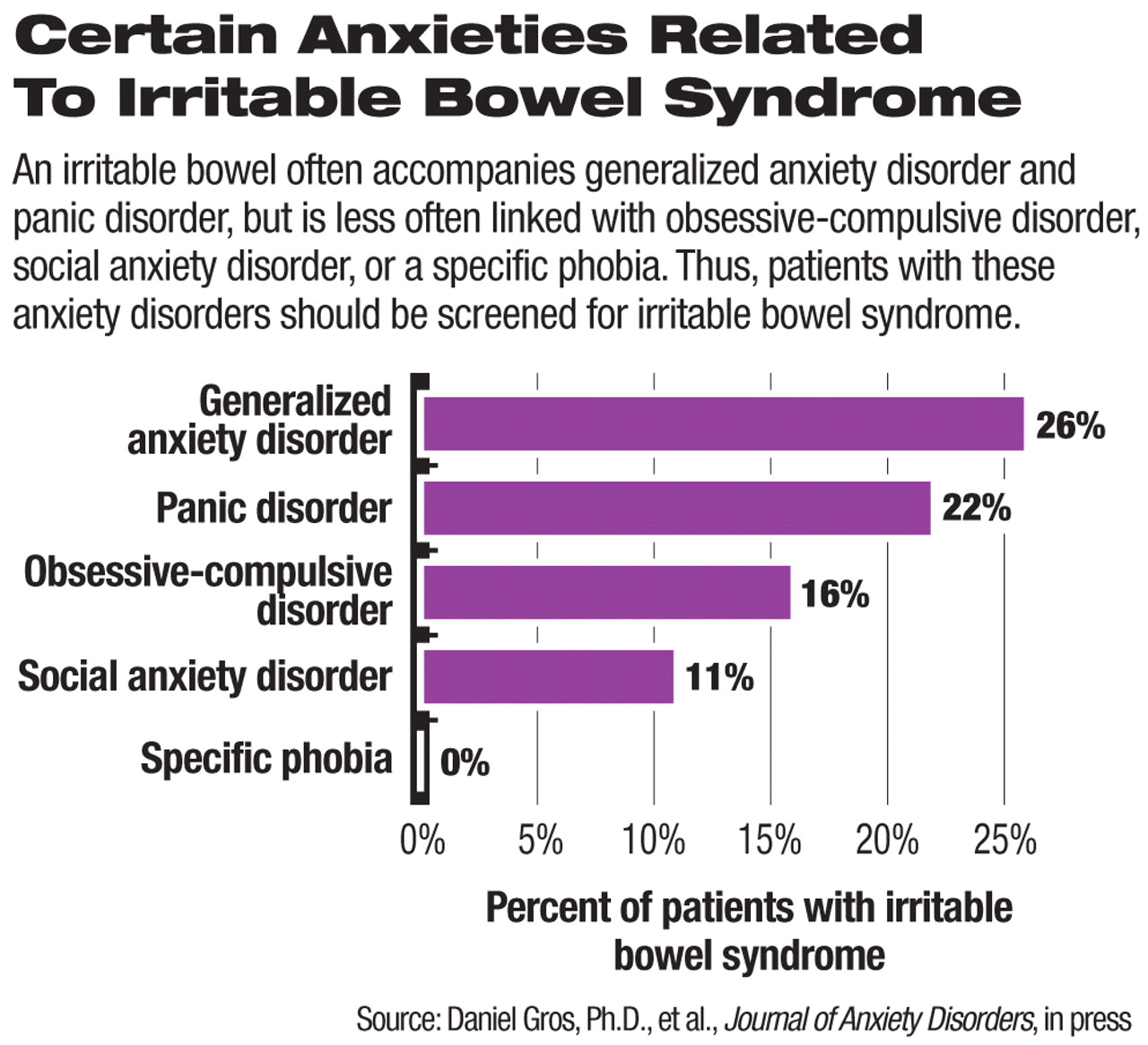
The investigators focused on 357 individuals who had come to an anxiety-disorder clinic for help with anxiety problems. They found that 17 percent of them had IBS. They also found the syndrome in a large number of subjects with generalized anxiety disorder or panic disorder, but in fewer with social anxiety disorder or obsessive-compulsive disorder and in none with a specific phobia. The syndrome was prevalent and severe among subjects with generalized anxiety disorder.
These findings prompted the researchers to examine more closely the relationship between various anxiety and depressive characteristics and IBS.
One important link they identified was worry—especially worry about illness and pain, because Gros and his colleagues found that subjects with generalized anxiety or panic were more anxious about illness and pain and more preoccupied with their bodies than were subjects with the other anxiet disorders.
An intolerance for uncertainty might be another crucial connection since such intolerance is often found both in individuals with generalized anxiety and in those with an irritable bowel, other researchers have found. And the worry about illness and pain and intolerance for uncertainty might then lead to dysfunction of the hypothalamic-pituitary-adrenal (HPA) axis. Such dysfunction has been linked with IBS and other inflammatory-related disorders such as fibromyalgia and chronic pain.
“It is possible that the stress response and vulnerabilities found in patients with panic disorder and generalized anxiety disorder ... may have a more severe impact on HPA-axis deregulation and excessive inflammatory activity than [the stress response and vulnerabilities found in patients with] social anxiety, specific phobia, and obsessive-compulsive disorder,” Gros told Psychiatric News.
In any event, the findings suggest that patients with generalized anxiety disorder or panic disorder should also be evaluated to see whether they have IBS, Gros and his team believe, and if that is the case, then they should be treated for both conditions.
The study had no outside funding.
An abstract of “Frequency and Severity of the Symptoms of Irritable Bowel Syndrome Across the Anxiety Disorders and Depression” can be accessed at<www.sciencedirect.com> under “Browse by Title” by clicking on “J,” then“ Journal of Anxiety Disorders,” then “Articles in Press.” ▪