Teenagers who suffer from antidepressant-resistant depression and have a concurrent history of family conflict, nonsuicidal self injury, or more severe symptoms of depression will likely have a poorer response to a new course of treatment, according to a study published in the March Journal of the American Academy of Child and Adolescent Psychiatry.
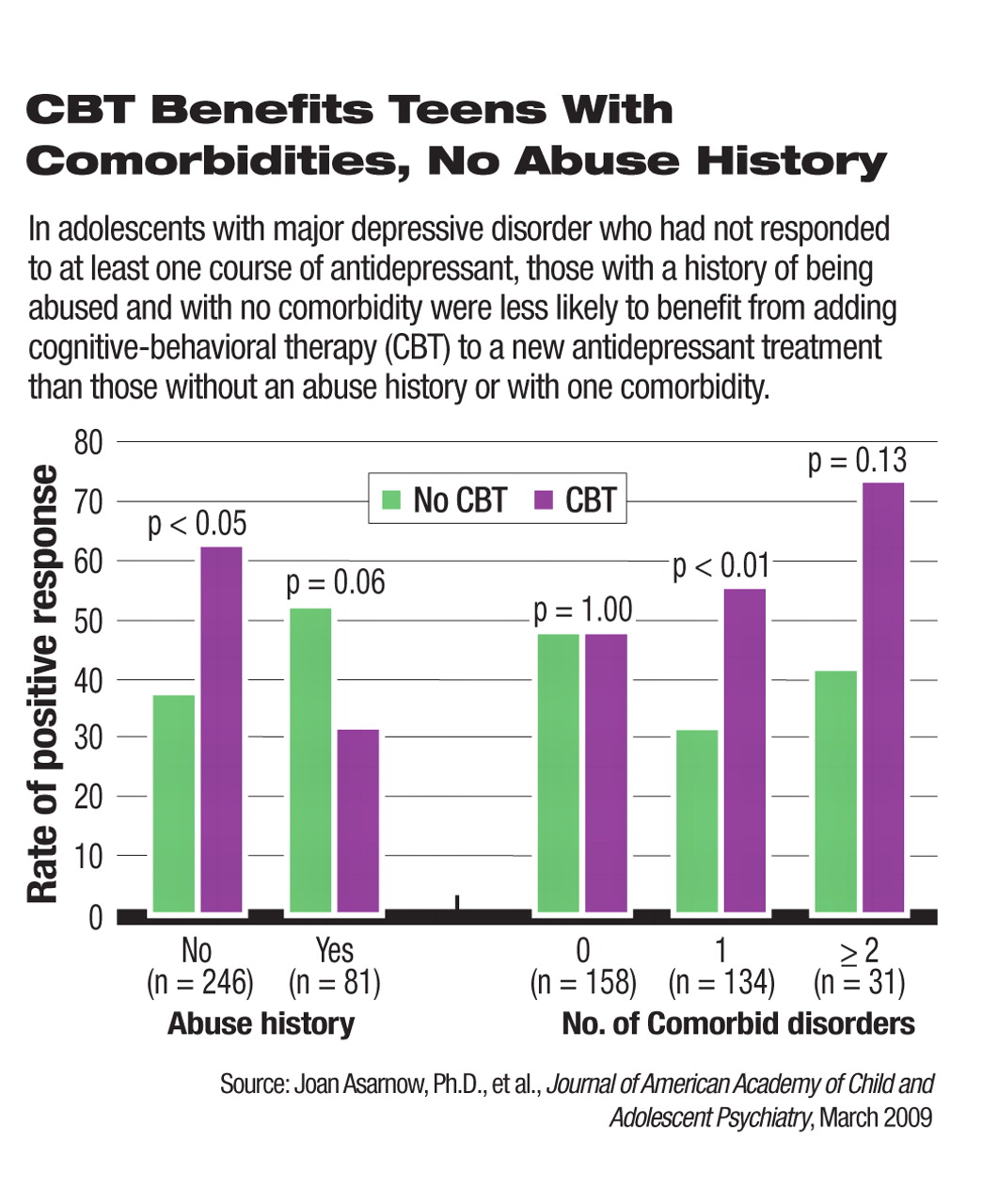
The study also found that adding cognitive-behavioral therapy (CBT) to antidepressant medications produces the most benefit for patients who have comorbidities such as anxiety disorders.
The study's findings can help clinicians individualize treatment plans for adolescents with more chronic and complicated forms of depression.
Analyzing the data from the Treatment-Resistant Depression in Adolescents (TORDIA) study, Joan Asarnow, Ph.D., a professor of psychiatry and behavioral sciences at the University of California at Los Angeles (UCLA) and the principal investigator of TORDIA at UCLA, and coauthors identified a number of patient characteristics that are associated with the likelihood of response to treatment and the benefit of medication—CBT combination therapy versus medication alone in this hard-to-treat population.
In the TORDIA study, 334 adolescents with moderate to severe depression who had failed to respond to a course of a selective serotonin-reuptake inhibitor (SSRI) were randomized to one of four treatments for 12 weeks: a different SSRI, a different SSRI plus CBT, venlafaxine, or venlafaxine plus CBT.
Because only 40 percent to 55 percent of these SSRI-resistant patients achieved response after the study treatment, knowing the predictors and moderators of clinical response can be valuable for clinicians in devising the most effective strategy as early as possible for patients who have already gone through a course of unsuccessful treatment.
A higher percentage of patients who received the medication and CBT combination reached clinical response than patients who received medication alone (Psychiatric News, March 21, 2008). The authors pointed out, however, that the response rate to the combination therapy was 54.8 percent, statistically significantly but not vastly higher than the 40.5 percent response to medication alone. In addition, they noted that high-quality CBT can be too expensive and inaccessible for many patients to take advantage of combination therapy.
Similar to previous research on first-step treatment response, depressed teens with a greater severity of depression symptoms, functional impairment, suicidal ideation, hopelessness, and youth-reported family conflict at baseline were more likely to have a poor response to the second-step treatment, the authors found. In addition, the analyses revealed a new link between a history of nonsuicidal self-injury, such as cutting, scratching, and burning, and poor treatment response.
“One of the predictors for poor response was high [level of] family conflict—this is a replication of previous studies,” David Brent, M.D., a professor of psychiatry at the University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic and the senior author of the study, told Psychiatric News. “For clinicians, [the message is that a] high level of family conflict will affect the efficacy of treatment and needs to be addressed and managed up front.” Brent was principal investigator of the TORDIA study at the Pittsburgh site.
The added benefit of CBT was particularly evident in patients with comorbid disorders, especially attention-deficit/hyperactivity disorder and anxiety disorders. “The combination therapy really pulled away from medication alone in these patients,” Brent commented. “Many patients in the community setting have these comorbidities. The combination therapy can be very cost-effective for this group.”
However, the addition of CBT to medication made no significant difference in patients with a history of being abused and a higher level of hopelessness. Treating depressed teens with a history of abuse and with nonsuicidal self-injurious behaviors is particularly challenging for psychiatrists, Brent acknowledged.
“A history of maltreatment predicted less response to CBT,” he said. “We don't quite understand the mechanism yet. Clinicians should take patients' history of maltreatment into consideration.... They may need more individualized treatment.”
Meanwhile, adolescents with nonsuicidal self-injurious behaviors“ have more difficulty with emotional regulation and [have] a lower stress tolerance,” according to Brent. He suggested that, although the addition of standard CBT did not provide substantial benefit for these patients in the study, psychotherapy with specific focus on addressing these deficits might be useful.
An abstract of “Treatment of Selective Reuptake Inhibitor–Resistant Depression in Adolescents: Predictors and Moderators of Treatment Response” is posted at<journals.lww.com/jaacap/Abstract/2009/03000/Treatment_of_Selective_Serotonin_Reuptake.13.aspx>.▪