Depression is a robust predictor of stroke, M. Maria Glymour, Sc.D., an assistant professor at the Harvard School of Public Health, and colleagues reported in the December 7, 2010, Neurology.
The study included some 19,000 Americans aged 50 or older. The cohort was oversampled for minority subjects to make sure that it was as representative of them as of white subjects.
None of the subjects had had a stroke prior to the start of the study. The subjects were evaluated for both depressive symptoms and memory impairment. Depressive symptoms were signalled by a score of 3 or more on the eight-item Centers for the Epidemiologic Study of Depression instrument. Memory impairment was defined as a score of 6 or less on a test of immediate and delayed recall of a 10-word list.
Subjects were then followed for about eight years to see whether they experienced a stroke, and about 1,900 (10 percent) did.
The researchers assessed whether there was an association between baseline depression and later having a stroke even when sociodemographic and cardiovascular risk factors were considered. They found that such an association did exist. Depression symptoms were also associated with an increased risk of stroke regardless of whether subjects were male or female or whether they were over or under age 65.
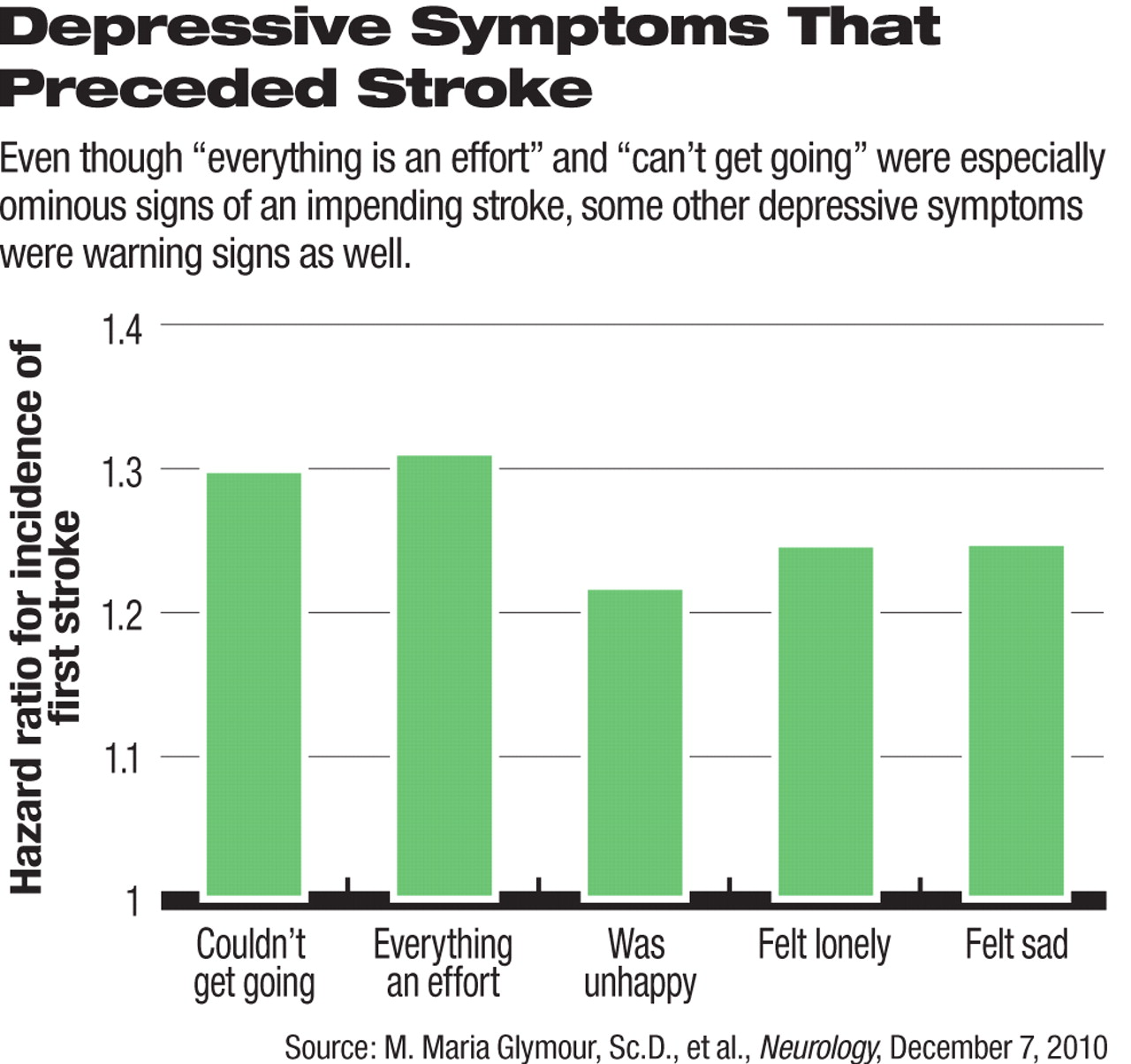
In addition, each one-point increase in baseline depressive symptoms was associated with an 8 percent increased risk of having a stroke. Two depressive symptoms—agreeing with the statements “everything is an effort” and “can't get going”—were especially ominous signs of an impending stroke.
“I was surprised at the robustness of the association between depressive symptoms and stroke,” Glymour told Psychiatric News. “It mattered very little how we modeled the association. Even if we used only a single item on the depressive symptom screen, we found that individuals who endorsed the symptom were at higher risk of subsequent stroke onset.”
The scientists then examined whether baseline memory impairment was linked with later having a stroke even when sociodemographic and cardiovascular risk factors were considered. Again they found that such a link did exist.
Finally they evaluated whether depressive symptoms predicted stroke independently of memory impairment, and whether memory impairment predicted stroke independently of depressive symptoms. The answer was affirmative in both cases.
And if depression does help trigger a stroke independently of memory impairments, what is the physiological mechanism? Probably not cerebrovascular disease, the researchers contend, and they outlined their line of reasoning in their paper: Since memory impairments that precede stroke probably reflect cerebrovascular disease, and since depression predicts stroke independently of memory impairments, then depression probably does not reflect cerebrovascular disease.
But if this is the case, then how might depression set the stage for a stroke? “One possibility that we were intrigued about,” Glymour said, “is that depressive symptoms may increase the risk of arrhythmias, such as atrial fibrillation. We do not yet have the data to examine this research question, but we hope to look at this in the future.”
Although this study “adds to the more recent literature suggesting that depression is a risk factor for stroke,” it contains several weaknesses, William Regenold, M.D., an associate professor of psychiatry at the University of Maryland and a geriatric psychiatrist and depression expert, told Psychiatric News.
One weakness is the researchers' assumption that the link between memory impairments and stroke is strictly cerebrovascular disease. Another is that they did not know which subjects were using SSRI antidepressants and therefore could not take into consideration the effect of SSRI antidepressants on stroke risk. The SSRIs can be anti-inflammatory and thus might help prevent stroke, but they can increase the risk of a bleed and might help trigger a stroke. And further complicating the SSRI-stroke scenario is that depression itself is inflammatory and thus capable of promoting a stroke.
“[So] how much [stroke] risk is due to depression and how much is due to medications used to treat it is unknown right now,” Regenold said.
The study was funded by the American Heart Association.