It’s a new era in American health care—one that calls for physicians to collaborate with other doctors and health care professionals in a new model of integrated care.
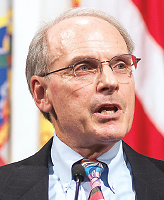
That’s what psychiatrist Jeremy Lazarus, M.D., president of the AMA, told delegates in his presidential address at the Interim Meeting of the AMA House of Delegates last month in Honolulu.
Integrated or collaborative care is a feature of the delivery system in the health care reform law, and policymakers and many clinicians have converged on the idea that the full range of medical services should be brought together in one patient-centered location.
But Lazarus noted that the move to integrated care requires a change in the core values that have traditionally motivated physicians—from autonomy to shared decision making and teamwork.
“For years, physicians have cherished autonomy,” Lazarus said. He quoted physician and medical writer Atul Gawande, M.D., who said that “the core structure of medicine—how health care is organized and practiced—emerged in an era when doctors could hold all the key information patients needed in their heads and manage everything required themselves.”
Lazarus noted that that was “before the red tape of big insurance and big government, before physician shortages, aging populations and chronic conditions, and before we had 6,000 drugs and 4,000 clinical procedures at our disposal.”
In that era, Lazarus said, it “made sense for physicians to value autonomy, independence, and self-sufficiency. But the game has changed. Integrated care asks us to cultivate mutual trust, to recognize that each team member offers unique skills and knowledge, and to support this trust with open and timely communication…. And we must go all in to improve the quality of health care for our patients and the country. That means collecting, sharing, and analyzing data, leveraged to care for patients. “
Lazarus added that he knows many physicians will resist the move to integrated care. “Perhaps they are trying to ride out a wave they fear will become a tsunami, or believe that these changes hamper their ability to think, create, or do good by patients,” he said. “I understand their concerns. And if their approach can match the quality goals of these new evolving systems [of integrated care], I support what they are doing. The AMA does not subscribe to one-size-fits-all solutions and welcomes all ideas. Nonetheless, for most physicians, these new systems can bring better results.”
As an example of the success of integrated care, Lazarus cited the Southcentral Foundation in Anchorage, Alaska, in which patients are assigned to a health care team that includes a physician, nurse, medical assistants, and even traditional healers. “Run by and for Alaska Natives, they’ve earned national attention for reducing health disparities and improving outcomes,” he said. “In the last decade, Southcentral Foundation has seen a decrease of 40 percent in visits to the emergency department, 75 percent in hospitalizations, and 30 percent in routine doctor visits. And they’ve made inroads in curbing disparities. Today, binge drinking, strokes, heart disease, and cancer rates among Alaska Natives are about the national average, a major victory for the demographic.”
In addition, Lazarus outlined recent AMA successes, as well as ongoing challenges. The latter include working to eliminate the Independent Payment Advisory Board established by the health care reform law and reforming the Medicare physician payment formula.
These were among the successes:
•.
Persuading the Centers for Medicare and Medicaid Services to revise its rules related to accountable care organizations so that relevant quality measures are used and financial risks for physicians are reduced.
•.
Securing physician representation on the “insurance exchanges” envisioned in the health care reform law and ensuring that health plans comply with state scope-of-practice laws.
•.
Delaying implementation of ICD-10.
•.
Working with the Medical Association of Georgia to fight insurance industry efforts to overturn state laws requiring that physician bills be paid on time—a confrontation that has national implications for holding third-party administrators accountable for late payments.
In his speech Lazarus noted that many of the AMA’s most important efforts are at the state level working with state medical societies and specialty groups. And while in Honolulu, he and other AMA leaders, as well as the entire psychiatric delegation, met with Hawaii Gov. Neil Abercrombie and a host of state legislators during a reception at the Hawaii Convention Center (see photo). Organized with the help of psychiatrist Jeffrey Akaka, M.D., a member of the Section Council on Psychiatry, it was an opportunity for physicians to talk to policymakers about scope of practice and other issues important to psychiatry and the rest of medicine.
In his address to the House of Delegates, Lazarus also noted that the AMA has been working with specialty societies in Florida to overturn a state law that prohibits physicians from asking patients and families about guns in their home and from noting a patient’s gun ownership in the medical record. (APA was among the organizations that signed on to an amicus curiae brief by the AMA challenging the law. See APA Urges Court to Reject Ban on Gun Discussions.)
“Lawmakers cannot insert the state into the patient-physician relationship by dictating, prohibiting, or threatening the open communication between patient and physician,” he said. “It’s been shown that patients who get physician counseling on firearm safety were more likely to adopt one or more safe gun-storage practices. We want to reduce firearm-related accidents and suicides.”