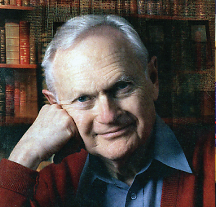
By most measures, surgeon, author, and educator Sherwin Nuland, M.D., is a great physician. By his own definition, he’s a “good” one too.
Nuland believes that while physicians’ kindness, compassion, and morality have been thought to play a key role in healing since the days of Hippocrates, “medicine at a distance” has increasingly become the standard of care. According to Nuland, this weakening of the doctor-patient relationship is in need of redressing.
Nuland has been invited as a guest lecturer at APA’s 2012 annual meeting in Philadelphia in May. In his lecture, titled “The Goodness of the Physician: From Hippocrates to High-Tech,” he will discuss how to strengthen the bond between doctor and patient to achieve lasting improvements in wellness and well-being.
Recently retired as a clinical professor of surgery at the Yale School of Medicine, Nuland serves on the executive committee of Yale’s Interdisciplinary Center for Bioethics and is a fellow of the American Association for the Advancement of Science, the Hastings Center, and Yale’s Institution for Social and Policy Studies.
After 30 years of practicing surgery at Yale-New Haven Hospital, Nuland launched a second career as a celebrated author of books on medical history and biomedical ethics. His 1994 best-seller, How We Die —a reflection on the modern way of death—won that year’s National Book Award and was a finalist for the 1995 Pulitzer Prize.
Nuland’s other books include Doctors: The Biography of Medicine; How We Live; The Mysteries Within: A Surgeon Explores Myth, Medicine, and the Human Body; The Doctors’ Plague: Germs, Childhood Fever, and the Strange Story of Ignac Semmelweis; The Art of Aging: A Doctor’s Prescription for Well-Being; and The Soul of Medicine: Tales from the Bedside. He has also written biographies of Leonardo da Vinci and the 12th-century Jewish sage Maimonides.
From 1998 to 2003, he wrote a column on medicine for The American Scholar, the contents of which were later published in book form under the title The Uncertain Art: Thoughts on a Life in Medicine.
In 2003, Nuland released a memoir (Lost in America: A Journey With My Father) in which he described a life-changing bout with depression. Nuland’s struggle with mental illness became so severe that he ended up spending more than one year in a psychiatric hospital. Following unsuccessful attempts to treat his depression with psychotherapy and medication, physicians at the institution recommended that he undergo a lobotomy.
It was the passion and commitment of a 27-year-old psychiatry resident at the hospital who threatened to resign in disagreement with his superiors that ultimately saved Nuland from the procedure. Nuland subsequently underwent a course of electroconvulsive therapy that he credits for his recovery.
Regrettably, this type of recognition of patients’ humanity has gotten lost amid an increased focus on evidence-based medicine and the bottom line, according to Nuland in the October 2000 Yale Alumni Magazine.
“The ideal doctor, the true caregiver, also needs the skills of the heart: the ability to create the aura that a patient is important to the physician and they’re both enmeshed in a journey they’re taking together,” he said.