Historically, the issue of racial and ethnic disparities in mental health care has been understudied (
1 ), but there is growing interest in documenting and understanding these differences (
2 ). From the work that has been reported, it is clear that racial and ethnic minority groups are disadvantaged relative to their white counterparts in overall receipt of services. Consistent with the larger literature on inequalities in other types of health care (
3,
4,
5,
6,
7,
8 ), there are significant differences in the use of mental health services on the basis of race and ethnicity (
9 ), even when economic and demographic factors are accounted for (
1,
10,
11,
12,
13,
14,
15,
16,
17 ). However, the key decisions affecting service availability are made at the organizational rather than individual level. Thus, in contrast to studies that examine the experiences of individuals within the mental health system, this research considers whether the racial and ethnic composition of substance abuse treatment organizations' caseloads is associated with the availability of selective serotonin reuptake inhibitors (SSRIs) in these settings.
The substantial rate of co-occurrence of substance abuse and psychiatric disorders highlights the need for delivery of appropriate treatment services for these conditions (
18,
19,
20 ). Given that unmet psychiatric needs predict worse substance abuse treatment outcomes (
21,
22,
23 ), experts in these fields have advocated the integration of services for substance abuse clients with co-occurring psychiatric treatment needs such that substance abuse and psychiatric services are provided within a single organizational setting (
24,
25 ).
One aspect of integrated care within the substance abuse treatment system is the availability of psychotropic medications. Mood disorders represent the most common type of co-occurring condition for this population (
20 ), and SSRIs may improve outcomes for some clients (
26 ). Although data from clinical trials suggest that SSRI effectiveness may be limited (
27 ), the safety and tolerability profiles of SSRIs have resulted in calls for them to be a "first-line treatment" for substance abuse clients with co-occurring depression (
28 ). However, there is little research regarding the extent to which these medications are made available within specialty substance abuse treatment centers, and no data are available to suggest whether there are racial-ethnic disparities in SSRI availability.
Individual-level analyses of the prescription of psychotropic medications have revealed significantly lower access to these medications among racial and ethnic minority groups (
2,
29,
30,
31,
32,
33,
34 ). Explanations of these disparities emphasize the characteristics of patients, including insurance coverage, socioeconomic status, and cultural differences in help seeking, as well as the characteristics of medical providers, including prejudices and stereotypes that may shape the clinical encounter (
1,
3,
13 ). Because data are usually collected at the individual level, it is unclear whether these racial disparities are also found at the organizational level, such that the racial-ethnic composition of an organization's caseload is associated with the services it provides.
Although individually focused research has resulted in important insights about disadvantages faced by clients with particular characteristics, working at this level of analysis masks the possibility that disparities may also be a function of variability in the availability of appropriate services among organizations that serve different client populations. The Institute of Medicine's report on racial disparities in health care suggested that racial and ethnic differences in the locations where individuals seek medical treatment are likely to produce disparities (
3 ). An association between racial-ethnic composition and the availability of psychiatric services, particularly after accounting for organizational resources such as funding and medical resources, would suggest that racial-ethnic disparities also operate at the level of the health care system in terms of the availability of mental health care services.
This research considered the issue of racial and ethnic disparities by modeling the likelihood of SSRI availability in substance abuse treatment centers as a function of the racial and ethnic composition of the center's caseload. In addition, this research examined whether any identified disparities were mediated by organizational-level control variables. The mediation of disparities by the control variables would suggest that racial and ethnic disparities may be partly explained by structural differences in the organizations that serve these populations.
Methods
Sample
Data were drawn from the National Treatment Center Study (NTCS), which focuses on the long-term adaptation of substance abuse treatment organizations to the environmental contexts in which they operate. The NTCS has several components, including nationally representative samples of specialty addiction treatment programs in the public and private sectors. The face-to-face interviews conducted with program administrators between mid-2002 and early 2004 represent the initial NTCS activity with the public-sector sample and the fourth such wave of data collection from the private-sector sample. The human subjects committee of the institutional review board at the University of Georgia approved the research design.
The NTCS uses a two-stage random sample of treatment programs. Separate samples were drawn for the public and private treatment center components. In both samples eligible facilities are community-based organizations that offer treatment for alcohol and drug problems and provide a level of care at least equivalent to structured outpatient programming as defined by the American Society of Addiction Medicine's patient placement criteria (
35 ). Excluded from the study were counselors in private practice, halfway houses, required driving-under-the-influence programs or other driver education programs, correctional institutions, treatment facilities operated by the federal government, and units exclusively offering methadone maintenance services.
A sample of 450 private-sector programs was drawn in 1994 (
36,
37 ). Over time, random sampling was used to select replacements for units that closed, became ineligible, or refused to participate, such that geographic stratification and a target sample of 400 were maintained. Private-sector programs were defined as those receiving less than 50% of their annual operating revenues from government block grants and contracts; the average private center received less than 9% of its revenues from such sources. The private sector included both for-profit and nonprofit programs. This study used data from those 403 private programs. The response rate for this wave of interviews was 88% of those that were sampled and eligible.
Using similar stratification and identification procedures, we selected a separate sample of public-sector treatment programs in early 2002. Eligibility rules were the same as for the private sample, except that public-sector programs were defined as receiving at least 51% of their annual operating revenues from federal, state, or local government grants or contracts; the average public center received nearly 80% of their revenues from these sources. The public-sector sample included a mixture of state and local government-owned facilities and nonprofits under private ownership. A total of 363 publicly funded treatment programs (80% response rate) were interviewed between mid-2002 and early 2004.
For both samples data were collected in face-to-face interviews with administrators and clinical directors who oversaw the substance abuse treatment services delivered by the organization. These interviews were conducted by trained members of the project staff. The average on-site interview lasted approximately 90 minutes.
The NTCS utilizes a longitudinal design that includes telephone follow-up interviews at six, 12, and 18 months after baseline face-to-face interviews. Our research drew from data collected during the first telephone follow-up interview. Of the 363 public centers, 326 (90%) participated in the follow-up; the rate of follow-up was 84% (N=339) among the private-sector sample.
In summary, these analyses relied on 665 centers that participated in both a baseline interview and a six-month follow-up interview. Pooled, unweighted data from these samples of private and public centers formed the basis for the analyses.
Measures
The dependent variable was availability of SSRI medications at the center. This measure was dichotomous (1, yes; 0, no) and was constructed on the basis of a series of items. First, administrators were asked if any client had ever been treated with SSRIs at the center. Administrators who answered yes were then asked additional questions; specifically, they were asked whether the center currently uses SSRIs to treat clients at the center. If administrators responded no, they were asked whether the center had discontinued use of SSRIs at the center. This follow-up question was used to ensure that centers were not erroneously coded as nonusers of SSRIs simply because no clients were receiving SSRI medications on the day of the interview.
The primary independent variables of interest were the percentages of clients at the center that represent racial or ethnic minority groups. Specifically, administrators reported the percentage of the center's African-American clients and the percentage of its Hispanic clients. These data were collected during a telephone follow-up interview six months after the face-to-face interview; the baseline interview included only an aggregate measure of racial-ethnic group representation in the center's caseload. (Specifically, administrators were asked in the baseline interview, "Typically, what proportion of your total caseload are racial and/or ethnic minorities?") Comparison of the data from the baseline interview and the six-month follow-up interview suggests that the racial-ethnic composition of the center's caseload was reasonably stable during this six-month period. When the percentages of African-American and Hispanic clients (from the six-month follow-up) were summed and this additive measure was compared with the baseline aggregate measure of racial-ethnic composition, the correlation was .80.
Center type was measured in four categories that integrated ownership, predominant sources of funding, and profit status. From the private center sample, facilities were coded as for profit or as privately funded nonprofit. Public centers were differentiated by ownership, such that centers were characterized as government owned or as publicly funded nonprofit. In these analyses, privately funded nonprofit treatment centers represent the reference category.
The measure of organizational affiliation categorized centers on the basis of whether they were affiliated with a hospital or mental health center or were freestanding (the reference category). This measure integrated information collected during the on-site interviews (such as ownership by or affiliation with a hospital) and data derived from the Substance Abuse and Mental Health Services Administration (SAMHSA) Mental Health Services Locator (www.mentalhealth.samhsa.gov/databases). The locator database was used to categorize sampled centers; about 25% of the sample identified themselves to SAMHSA as a mental health service provider. The database further categorized these centers as general hospitals, psychiatric hospitals, substance abuse organizations, multisite mental health organizations, and outpatient clinics. Facilities listed in the database as hospitals or as substance abuse organizations retained their hospital or freestanding code in our data set. However, facilities identifying themselves as multisite or outpatient mental health facilities were coded as mental health centers for these analyses.
Two geographical measures were included in the model of SSRI availability. First, the state in which the center was located was coded into four geographic regions: Northeast, Midwest, South (reference), and West. Second, a dichotomous measure of location in a rural county was constructed on the basis of whether the county was within a metropolitan statistical area. Both measures use current U.S. Census area definitions.
Other organizational characteristics included center age, center size, accreditation status, physician availability, presence of a dual diagnosis program offering integrated care, and adherence to a 12-step treatment model. Center age was measured in years, and center size was measured by the number of full-time-equivalent employees; both measures were natural log-transformed to correct for substantial skew. Accreditation by the Joint Commission on Accreditation of Healthcare Organizations or the Commission on Rehabilitation Facilities (1, yes; 0, no) was included as a proxy measure of center quality (
38 ). A set of dummy variables categorized the type of physician availability at the center: at least one physician on staff, at least one physician on contract, and no physicians (reference). Center administrators were asked whether they offered a dual diagnosis program that addressed both the mental health and substance abuse needs of clients (1, integrated care program; 0, no integrated care program). Finally, a dichotomous measure was included to identify whether the center was based on a 12-step model of recovery (1, yes; 0, no).
Analysis
Logistic regression was used to estimate three models of SSRI availability in specialty substance abuse treatment centers because of the dichotomous nature of the dependent variable (
39 ). The bivariate association between the percentage of racial-ethnic minority clients and the likelihood of SSRI availability was presented in model 1. In model 2, center type and basic organizational characteristics were added to the regression equation. In model 3, measures related to treatment inputs, including physician availability, availability of integrated care, and the 12-step orientation of the center, were added to the analysis. Unstandardized coefficients and standard errors are reported as well as several measures of model fit, including likelihood ratio chi square tests, McKelvey and Zavoina's R
2, and the Bayesian information criterion (BIC). McKelvey and Zavoina's R
2 attempts to model the proportion of variation explained by the independent variables and has properties that are preferable to other pseudo-R
2 measures (
40,
41 ). More negative BIC values also indicate improvement in model fit (
42 ).
All three models used the subsample of 578 centers that provided complete information on all measures. Additional analyses (not shown) were undertaken to examine possible sources of bias because of missing data. First, centers with complete data were compared with those that were excluded in the models of SSRI availability because of missing data. Chi square and t tests were used to compare included and excluded centers on all variables. The only significant difference was in the natural log-transformed measure of full-time employees. Centers providing complete data were smaller (mean±SD=2.80±1.12) than centers that were excluded because of missing data (3.06±1.34; t=2.50, df=751, p<.01).
An additional source of missing data was related to the six-month follow-up interview, which included the measures related to racial-ethnic caseload composition; some centers did not complete this interview, whereas others were unable to provide specific information on the racial-ethnic composition of the center's caseload. A logistic regression analysis was performed where the dependent variable was coded 1, indicating missing data on the race-ethnicity variables, or 0, indicating that the center provided these data. Neither the measure of SSRI availability nor the other organization-level measures were associated with the likelihood of missing race-ethnicity data.
Results
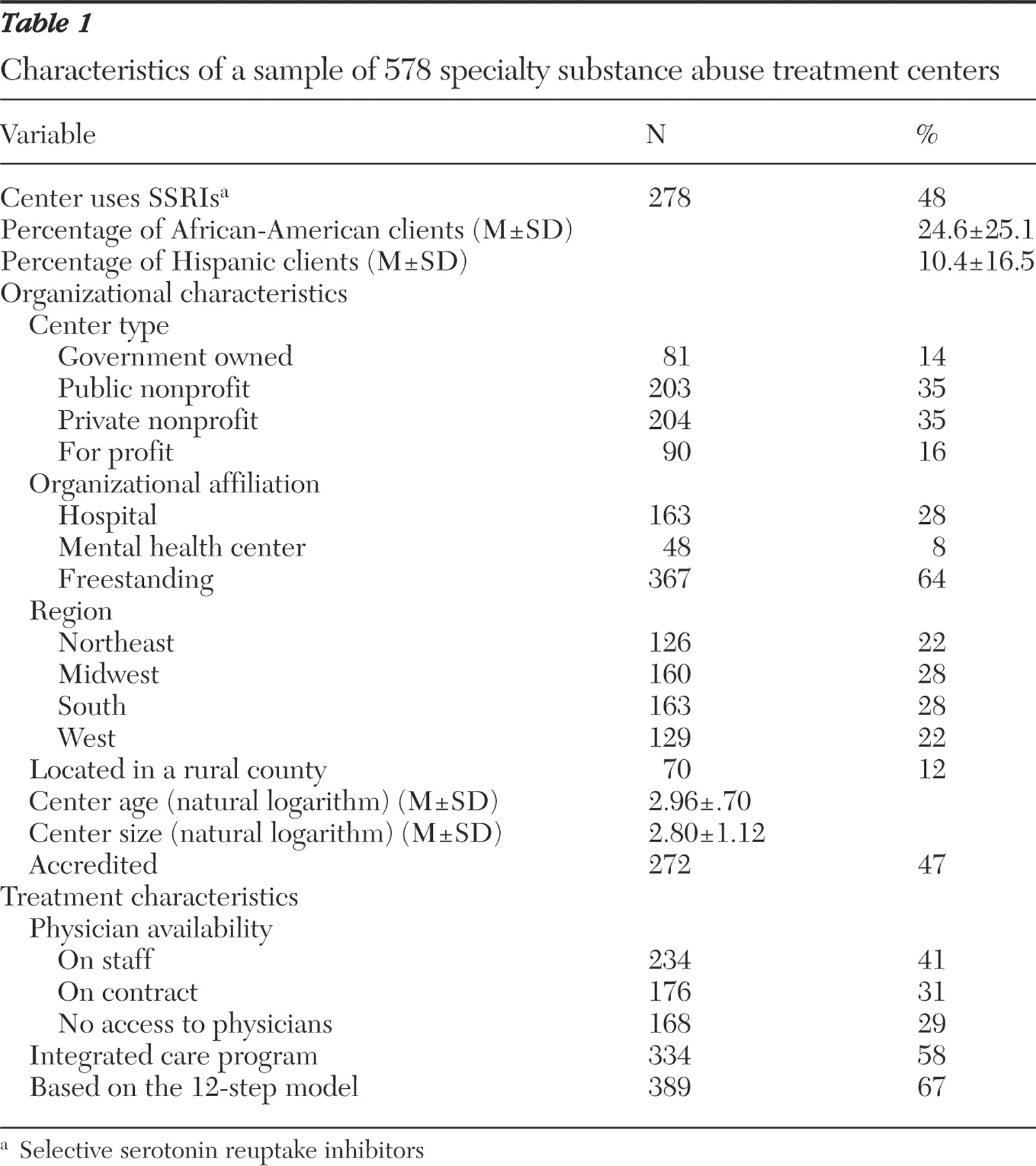
Descriptive statistics for all variables appear in
Table 1 . SSRI medications were available in about 48% of the substance abuse treatment centers in the sample. Within the sampled treatment centers, the mean±SD percentage of African-American clients was 25±25, whereas the mean percentage of Hispanic clients was 10±17.
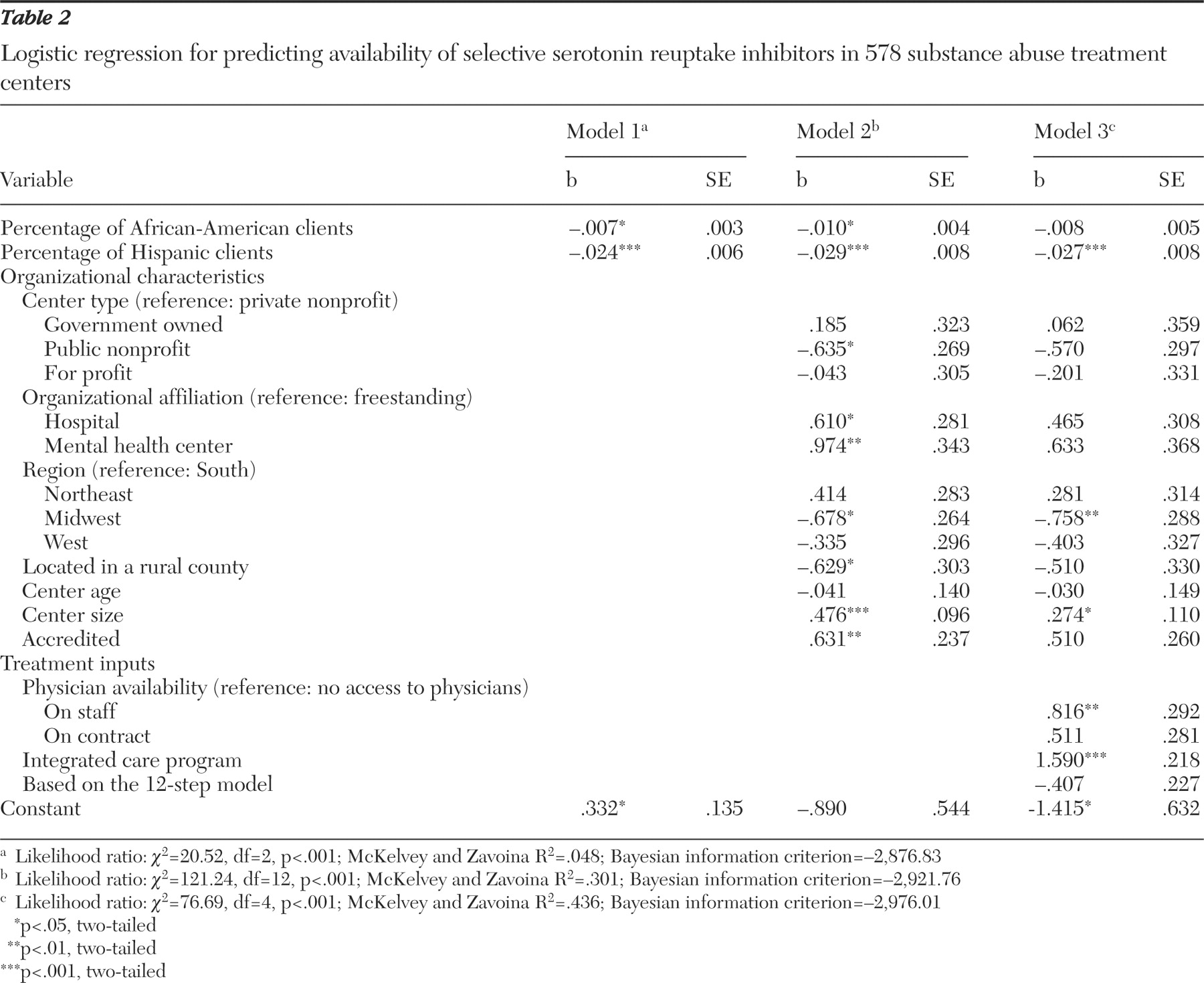
Table 2 presents the logistic regression results, with the associations between the percentages of African-American and Hispanic clients and the likelihood of SSRI availability reported in model 1. Both associations were significant and in the negative direction, suggesting that centers with greater percentages of minority clients were significantly less likely to make available this class of medications. A standard deviation increase in the percentage of African-American clients was associated with a 16% decrease in the likelihood of SSRI availability (odds ratio [OR]=.99, p<.05). Likewise, a standard deviation increase in the percentage of Hispanic clients was associated with a 32% decrease in the odds that SSRIs were available at the center (OR=.98, p<.001).
Organizational characteristics were added in model 2. Both measures of racial and ethnic composition remained significant, even after we controlled for these organization-level variables. In this second model a standard deviation increase in the percentage of African-American clients was associated with a 21% reduction in the odds of SSRI availability (OR=.99, p<.05), whereas a standard deviation increase in the percentage of Hispanic clients was associated with a 38% decrease in the availability of SSRIs (OR=.97, p<.001).
In addition several of the organizational characteristics added in model 2 were associated with SSRI availability. Publicly funded nonprofit facilities were significantly less likely than privately funded nonprofit centers to make SSRIs available (OR=.53, p<.05). Organizational affiliation was also associated with the availability of SSRIs. Compared with freestanding centers, centers affiliated with hospitals (OR=1.84, p<.05) and mental health centers (OR=2.65, p<.01) were more likely to offer SSRI medications. The only regional difference was that centers located in the Midwest were less likely than centers in the South to make SSRIs available (OR=.51, p<.05). Rural centers were significantly less likely than nonrural centers to offer SSRIs (OR=.53, p<.05). There was a significant positive association between center size and SSRI availability (OR=1.61, p<.001). Finally, accredited centers were about 88% more likely than nonaccredited centers to offer these medications (OR=1.88, p<.01).
In the final model, three measures of treatment inputs—physician availability, integrated care, and 12-step orientation—were added to the model of SSRI availability. The addition of these variables fully mediated the association between the percentage of African-American clients and the availability of SSRIs (p=.09). However, the negative association between the percentage of Hispanic clients and SSRI availability remained significant after we controlled for organizational characteristics and treatment inputs (OR=.97, p<.01). After controlling for organizational characteristics and treatment inputs, we found that a standard deviation increase in the percentage of Hispanic clients was associated with a 35% decrease in the odds that the center offered SSRIs.
The addition of these measures of treatment inputs mediated several of the associations between organizational characteristics and SSRI availability. Differences based on center type, organizational affiliation, and rural location were no longer significant, although the difference between accredited and nonaccredited centers maintained significance (OR=1.66, p=.05). Location in the Midwest relative to the South (OR=.47, p<.01) and center size (OR=1.31, p<.05) remained significantly associated with SSRI availability.
Of the treatment inputs, the availability of integrated care was most strongly associated with SSRI availability (OR=4.90, p<.001). In addition, centers with at least one physician on staff were significantly more likely than centers without physician services to offer SSRIs (OR=2.26, p<.01). The difference between centers with contract physicians and those without physicians approached, but did not achieve, significance (p=.07).
Given the importance of these treatment inputs, we conducted additional analyses to more fully understand the associations between the measures of racial-ethnic composition and these variables. There was no association between the measures of minority clients and physician availability. However, centers with integrated care programs reported significantly lower proportions of African-American (23%±24%) and Hispanic (8%±12%) clients than centers not offering integrated care (27%±26% for African Americans; t=2.03, df=576, p<.05; 13%±21% for Hispanics, t=3.79, df=576, p<.001).
Integrated care programs were more likely to be offered by centers affiliated with hospitals (72%) and mental health centers (77%) than freestanding clinics (49%), so analyses were also conducted to examine minority representation by organizational affiliation. Analyses of variance revealed significant mean differences in the percentages of these groups by organizational affiliation. The average proportion of African-American clients was 21% in hospital-affiliated programs, 21% in mental health centers, and 27% in freestanding facilities (F=3.21, df=2 and 575, p<.05). The average proportion of Hispanic clients in hospital, mental health center, and freestanding programs was 7%, 12%, and 12%, respectively (F=4.83, df=2 and 575, p<.01).
Discussion
Although a relatively recent development, SSRIs have become an established pharmacotherapy within the context of substance abuse treatment. Nearly half of the treatment centers in this study offered SSRIs during the course of treatment for clients with co-occurring addiction and psychiatric disorders. However, there was a significant inverse relationship between the proportion of African-American and Hispanic clients and the availability of SSRIs in these centers. These relationships held even after analyses controlled for several organizational characteristics. However, the addition of treatment characteristics mediated the association between the percentage of African American clients and the availability of SSRIs such that it was no longer statistically significant. In the final model, the percentage of Hispanic clients continued to be negatively associated with SSRI availability.
Additional analyses suggested that these associations are indicative of a larger disparity in the availability of integrated care services. Data from this study suggest that centers offering integrated care for co-occurring psychiatric and substance abuse conditions have caseloads in which African-American and Hispanic clients are less represented. These integrated care programs are more likely to be embedded in hospital-affiliated and mental health center-affiliated treatment facilities; however, centers affiliated with hospitals also reported smaller percentages of clients from racial and ethnic minority groups. Greater attention by policy makers to the availability of integrated care programs might begin to address the disparities identified in this research.
Whereas much of the research on disparities in health services focuses on individual clients as the unit of analysis, the data from this study suggest that racial and ethnic disparities should also be considered at the organizational and system levels. If organizational adoption of particular treatment techniques varies with the racial and ethnic composition of a center's caseload, then apparent health care disparities may be better understood, in part, as a function of the services offered by the organizations from which clients seek care. Rectifying such inequalities may require system-level efforts to ensure equal access to hospital-based programs and mental health centers, enhance program quality, and increase overall rates of adoption of evidence-based treatment practices.
On the other hand, some part of the observed variation may be explained by differences in consumer demand for antidepressant medications in treatment centers serving a high proportion of minority clients. For example, individual-level data on women of racial and ethnic minority groups suggest that there are racial and ethnic differences in perceptions regarding mental health needs (
43 ). Another recent study revealed racial differences in the likelihood that clients had their antidepressant prescriptions filled (
44 ). To some extent, organization-level differences in the availability of SSRI medications may in part reflect differences in consumer demand for these medications. Future research should explore the role of consumer demand in the availability of psychotropic medications within substance abuse treatment settings. Relatedly, research should consider differential compliance with treatment recommendations and steps taken by treatment organizations to enhance rates of medication compliance.
Some limitations of these analyses should be noted. These are organization-level data, and as such, these analyses cannot predict the probability that an individual with co-occurring mental illness and substance abuse will receive SSRI medications within these centers. The collection of multilevel data, at the levels of organizations and individual patients, may yield additional insights into health disparities in these treatment settings. In addition, these models focused on availability of SSRIs in terms of any use within the treatment facility. Further research is needed on differential implementation of SSRIs within these programs, in terms of their routine use in the treatment of clients with co-occurring disorders. Identifying systematic disparities in access to medications within treatment centers is an important area for future research. Nevertheless, organizational adoption is a necessary condition for service delivery to individual clients.
Other limitations are related to the design of the study. This study largely relied on self-reported data provided by center administrators, including the measures of racial and ethnic composition. Reliance on self-reported data may have been a source of bias. However, the average percentages of African-American and Hispanic clients reported by administrators (25% and 10%, respectively) are similar to the national racial and ethnic distribution seen in client-level data reported in the 2003 Treatment Episode Data Set (TEDS); the TEDS data indicated that African Americans constituted 24% and Hispanics represented 13% of substance abuse treatment admissions (
45 ). The similarities between these two sources of data provide validity for the estimates of these self-reported measures.
Some cases were lost because of the necessity of relying on data collected during the six-month follow-up interview in order to have information on specific racial and ethnic groups. However, these measures were strongly correlated with an aggregated measure of racial-ethnic composition collected during the baseline interview. In order to examine whether bias was introduced by relying on the subset of centers participating in both the baseline and follow-up interviews, we performed a logistic regression analysis that modeled the probability that the center's data on the race-ethnicity measures were missing, with all of the other measures as independent variables. None of the variables were associated with the log-odds that a center did not provide data on the percentages of African-American and Hispanic clients.
Conclusions
These data from large national samples of publicly funded and privately funded substance abuse treatment centers revealed a significant difference in the availability of SSRI medications that was associated with the racial-ethnic composition of the center's caseload. The inclusion of organizational characteristics and treatment factors as control variables mitigated the association for the percentage of African-American clients, but the association for the percentage of Hispanic clients remained significant. Future research should continue to consider racial and ethnic disparities in the availability of psychiatric services at the level of organizations. Further examination of disparities may yield important information about the mechanisms that have produced these differences, which can then be used to inform mental health care policy.
Acknowledgments and disclosures
The authors gratefully acknowledge the research support of the National Institute on Drug Abuse (R01-DA-13110 and R01-DA-14482).
The authors report no competing interests.