Even before Hurricane Katrina struck in late August 2005, people in the U.S. Gulf Coast were among the sickest, poorest, and most underserved in the country (
1 ). Their burdens were severely compounded by the subsequent devastation and displacements experienced by 1.5 million inhabitants in an area the size of Great Britain (
2,
3 ). More than $100 billion in federal aid has already been allocated or requested, much of it initially focused on addressing immediate needs for shelter, food, injuries, and other acute medical conditions (
4,
5,
6,
7,
8,
9,
10,
11 ).
Treatment needs of the many Katrina survivors with mental disorders have received far less attention, despite the fact that the widespread experience of trauma may have precipitated many new cases and exacerbated preexisting mental disorders (
12 ). Entire delivery systems were destroyed, and people with mental disorders may have been unable to overcome the formidable financial, structural, and other barriers to obtaining care (
13 ). Attitudinal barriers and competing demands may have prevented even those with access from obtaining effective treatments (
14,
15 ).
The aims of the study presented here were to describe the mental health services used by respondents to a geographically representative survey of displaced and nondisplaced Katrina survivors. We examined the system sectors and treatment modalities used as well as the intensity and continuity of treatments. We also identified correlates and reasons for undertreatment to help ensure that future relief efforts will meet the needs of survivors with mental illness.
Methods
Sample
Data come from the Hurricane Katrina Community Advisory Group (CAG), a representative sample of 1,043 prehurricane residents of counties in Alabama and Mississippi and parishes in Louisiana that were defined by the Federal Emergency Management Agency (FEMA) as directly affected by Katrina (
12,
16 ). The target population for the CAG was English-speaking adults aged 18 and older who were prehurricane residents of these areas and who were in either of two sampling frames: a random-digit dial telephone frame and a frame that included the telephone numbers of the roughly 1.4 million families that applied to the American Red Cross for assistance. Prehurricane residents of the New Orleans metropolitan area were oversampled. Potential respondents were informed that joining the CAG required a commitment to participate in follow-up surveys over several years and provide tracing information if they moved.
Between January 19 and March 31, 2006, the 1,043 respondents who agreed were administered by telephone the baseline CAG survey; this group represented an estimated 41.9% of all the individuals whom we attempted to contact or interview. This is only an estimate because we had no definitive way to determine the true proportion of all the phone numbers never contacted that were working numbers. Responses to a brief questionnaire that was administered to an informant in all households contacted, whether or not the designated respondent in the household subsequently agreed to join the CAG, were used to weight the responses of the CAG sample to adjust for somewhat lower trauma exposure and lower prevalence of hurricane-related psychological distress among those who agreed to join the CAG compared with those who decided not to join. Other weights adjusted for probability of selection and residual discrepancies between the CAG and the population of the affected area in 2000 as characterized by the U.S. Census Bureau. The consolidated CAG sample weight was trimmed to increase design efficiency on the basis of evidence that trimming did not significantly affect prevalence estimates of mental disorders. More detailed information on CAG sampling and weighting is available elsewhere (www.hurricanekatrina.med.harvard.edu). Institutional review board approval from Harvard Medical School and informed consent were obtained.
Measures
Thirty-day mental disorders. The K6 scale of nonspecific psychological distress (
17 ) was used to screen for
DSM-IV anxiety and mood disorders in the 30 days before the interview. On the basis of a previous validation study (
18 ), a score of 13 or greater (possible range of 0 to 24) was considered as probable serious mental illness in the previous 30 days. A score of 8 to 12 was considered as probable mild-moderate mental illness in the previous 30 days, and a score of 0 to 7 was considered as probable absence of mental illness in the previous 30 days. A small clinical reappraisal study that administered the Structured Clinical Interview for DSM-IV (SCID) (
19 ) to five respondents with probable serious mental illness, five with probable mild-moderate mental illness, and five with probable absence of mental illness confirmed K6 classifications for 14 respondents; the exception was a respondent who was classified as having serious mental illness by the K6 and as having mild-moderate mental illness by the SCID with a Global Assessment of Functioning score of 65.
Mental health service use. Respondents were asked whether since the hurricane they received professional counseling for "problems with your emotions, nerves, or mental health." If respondents answered affirmatively, they were asked what types of professionals they saw, the number of visits made, the average length of sessions, whether they were still receiving counseling, and if not, the reasons for stopping. Professionals were classified as psychiatrists, other mental health specialists (psychologist, psychotherapist, and any form of mental health counselor), general medical providers (primary care physician, other general medical physician, nurse, and any other health professional not previously mentioned), human services professionals (religious or spiritual advisor or social worker), and complementary-alternative medicine professionals (any other type of healer, such as a chiropractor, herbalist, or spiritualist). Respondents were asked to provide information on prescription medicines taken for problems with emotions, nerves, or mental health since the hurricane, including the name of the medication, number of days taken, and type of provider prescribing it.
Reasons for not using services or not continuing to use them. Respondents who reported no use of mental health services were asked whether there was a time since the hurricane that they felt they might have needed to see a professional for problems with their emotions, nerves, or mental health. Those who answered affirmatively were then asked to endorse reasons that they did not see a professional from a list of potential reasons, including low need (for example, they thought that the problem was not severe or would get better by itself), lack of enabling factors (for example, lack of financial means, available treatments, personnel, or transportation or the presence of other inconveniences), and lack of predisposing factors (for example, the presence of stigma, low perceived efficacy of treatments, or the desire to handle the problem on their own). Respondents who used services since the hurricane but ceased to do so were asked to endorse a similar set of reasons for stopping.
Sociodemographic characteristics. Sociodemographic information obtained included age (18 to 39, 40 to 59, and 60 years and older), sex, race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), family income in the year before the hurricane (low, at or below the federal poverty line for the family size and composition; low-average, above the poverty line but no higher than the median ratio of income to family members; high-average, above the median to three times the median ratio of income to family members; or high, above three times the median ratio of income to family members), education (less than high school, high school, some college, or college graduate), marital status (married, previously married, or never married), home ownership status (own without a mortgage, own with a mortgage, or rent or occupy without rent), prehurricane location (New Orleans City, remainder of metropolitan New Orleans, or remainder of the hurricane area), posthurricane location (same house, same town but different house, or different city), and insurance status.
Analysis methods
Prevalence rates of using any services, specific sectors, or specific treatment modalities and of continuing in treatment were estimated for the sample of 1,043 respondents on the basis of the sample's responses, and separate estimates were made for strata defined by severity of mental disorder. Frequency distributions of perception of a need for treatment, reasons for not seeking treatment, and reasons for dropout were recorded. Logistic regression analyses were used to examine correlates of using services among all respondents and of continuing in and dropping out of treatments among respondents who used services. All analyses were carried out with use of the design-based Taylor series linearization method (
20 ). Multivariate significance was estimated using Wald chi square tests on the basis of design-corrected coefficient variance-covariance matrices.
Results
Use of services by severity of illness
As reported in a previous publication from this study (
12 ), 31% of CAG respondents were estimated to meet criteria for a
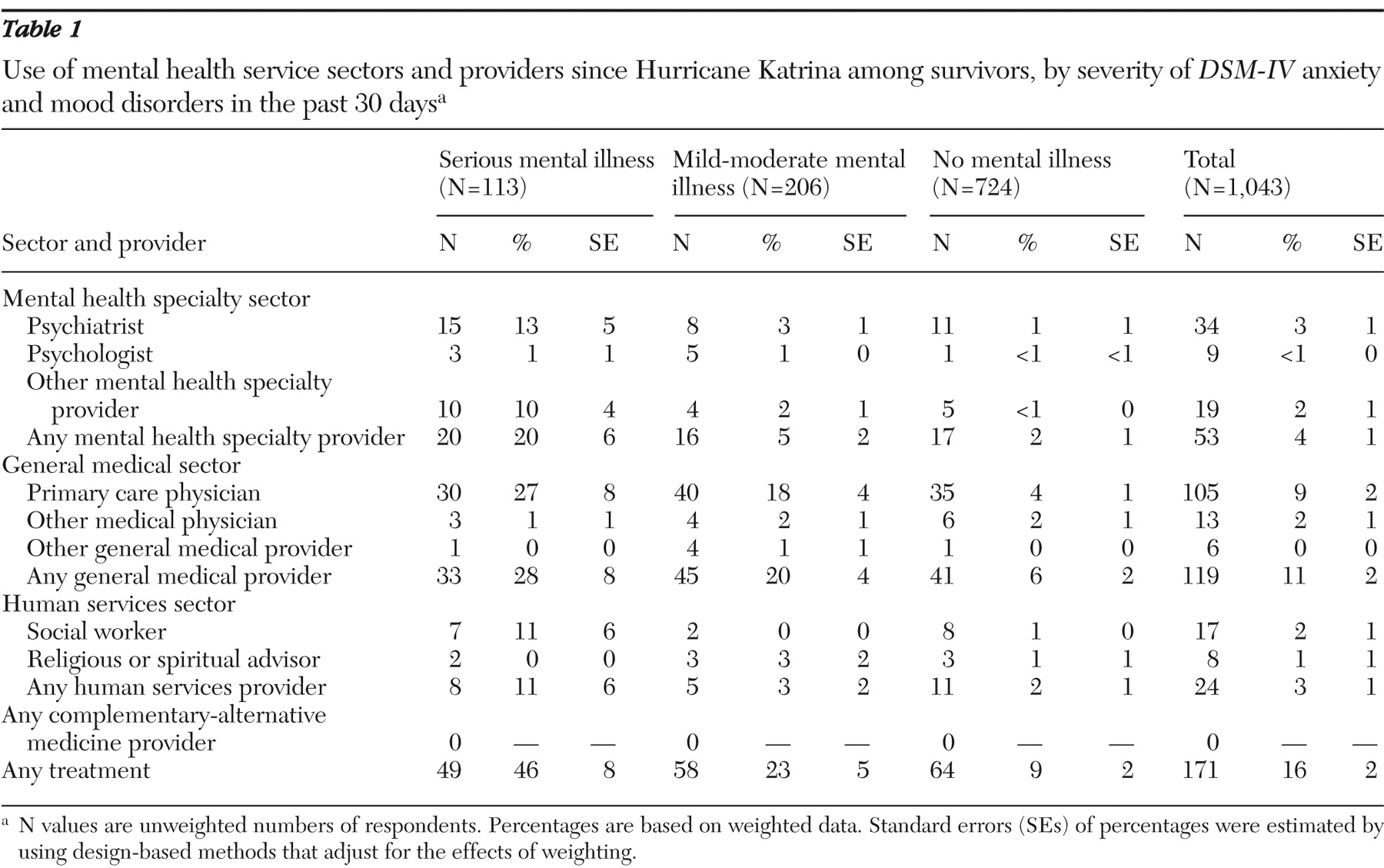
DSM-IV mood or anxiety disorder in the 30 days before interview; 11% of respondents were classified as having a seriously impairing mood or anxiety disorder and 20% as having a mild-moderate mood or anxiety disorder. As
Table 1 shows, 16% of respondents used mental health services since the disaster, including 46% of those with serious anxiety or mood disorders in the past 30 days and 23% with mild-moderate anxiety or mood disorders in the past 30 days (32% of those with either serious or mild-moderate disorders [results not shown but available on request]), and 9% of those with no disorders of these types. Among all respondents, the general medical sector was used most commonly. Overall, 11% of respondents received services in the general medical sector, followed by the mental health specialty sector (4% of respondents), and the human services sector (3%). No respondents reported use of the complementary-alternative medicine sector. This pattern of sector use was evident in all groups defined by severity of disorder.
Use of psychotherapy and pharmacotherapy
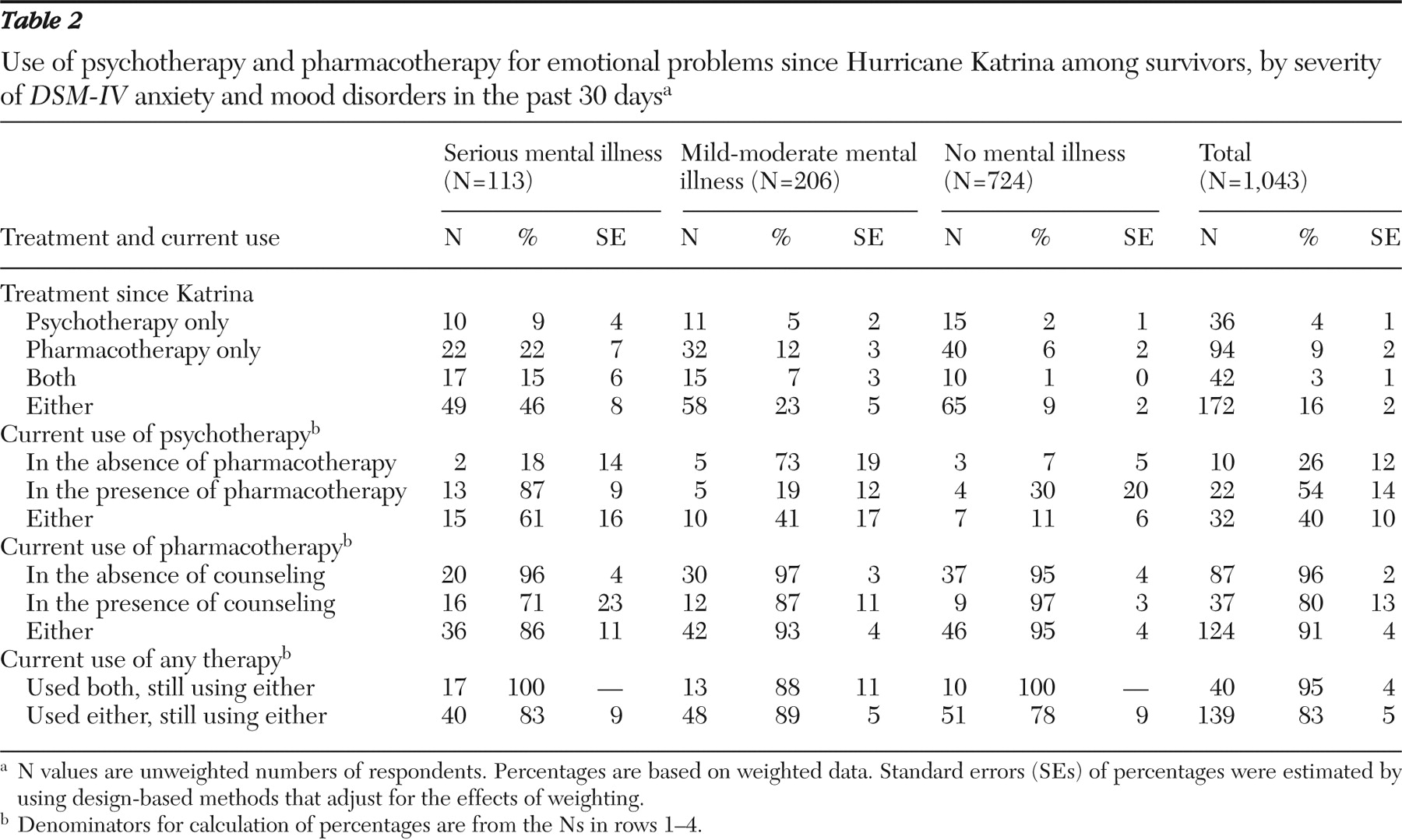
As shown in
Table 2, the most common treatment was pharmacotherapy alone (used by 9% of respondents), followed by psychotherapy alone (4%), and pharmacotherapy plus psychotherapy (3%). The relationships between disorder severity and use of these treatments were generally monotonic. Combined pharmacotherapy plus psychotherapy was the second most commonly used treatment among respondents with serious disorders, whereas it was the least common among respondents without serious or mild-moderate disorders.
Among respondents who received treatment since the disaster, only a minority were still receiving psychotherapy at the time of the interview. On the other hand, the vast majority of those treated since the disaster were still receiving pharmacotherapy. Continuing use of any treatment at the time of the interview was more common among those who had ever used combined-modality treatment than among those who had used a single modality only (95% compared with 83%).
Types of psychotropic medications
The most frequently used specific classes of psychotropic medication were antidepressants (used by 91 respondents, or 60% of those using any type of psychotropic medication), followed by benzodiazepines (43 respondents, or 30%), mood stabilizers (five respondents, or 6%), nonbenzodiazepine hypnotics (14 respondents, or 5%), and antipsychotics (six respondents, or 3%). (More detailed results are available at hurricanekatrina.med.harvard.edu/publications.php.) Generally monotonic relationships between disorder severity and use of individual drug classes existed only for antipsychotics, mood stabilizers, and nonbenzodiazepine hypnotics.
Number and duration of psychotherapy visits
Although 59 of the 78 psychotherapy users had visits that typically lasted for 30 minutes or more, 19 did not. Likewise, the number of psychotherapy visits obtained since the disaster was low; only 11 respondents (9%) received eight or more visits, and 46 (64%) received one or two visits.
Perceived need and reasons for not using services
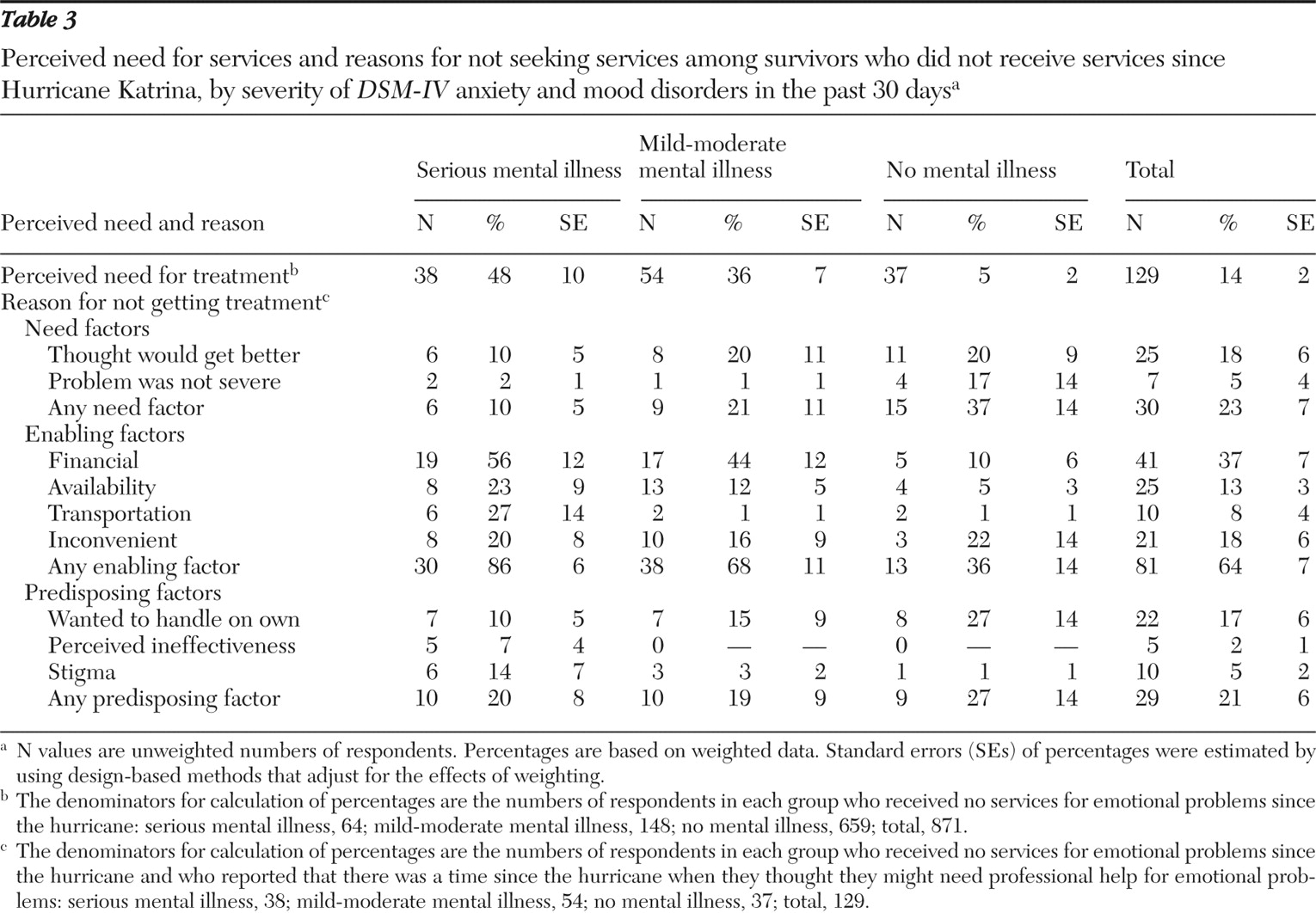
As
Table 3 shows, 14% of the respondents who reported not using treatment felt that they needed mental health care. The proportion ranged from 48% among those with serious mental illness to 5% among those with neither serious nor mild-moderate mental illness. Among those who perceived a need for treatment, nearly 64% reported a lack of enabling factors (for example, available services, financial means, and transportation) as a reason for not seeking care; the proportion ranged from 86% of those with serious mental illness to 36% of those with neither serious nor mild-moderate mental illness.
Low need (for example, thinking that the problem was not severe or would get better on its own) was reported as a reason by 23% of all respondents; the proportion ranged from 10% of those with serious mental illness to 37% of those with neither serious nor mild-moderate mental illness. Attitudinal or predisposing factors (for example, stigma, perceived ineffectiveness of treatment, or a desire to handle the problem on one's own) were reported by 21% of respondents; the proportion ranged from 19% of those with mild-moderate mental illness to 27% of those with neither serious nor mild-moderate mental illness.
Treatment dropout
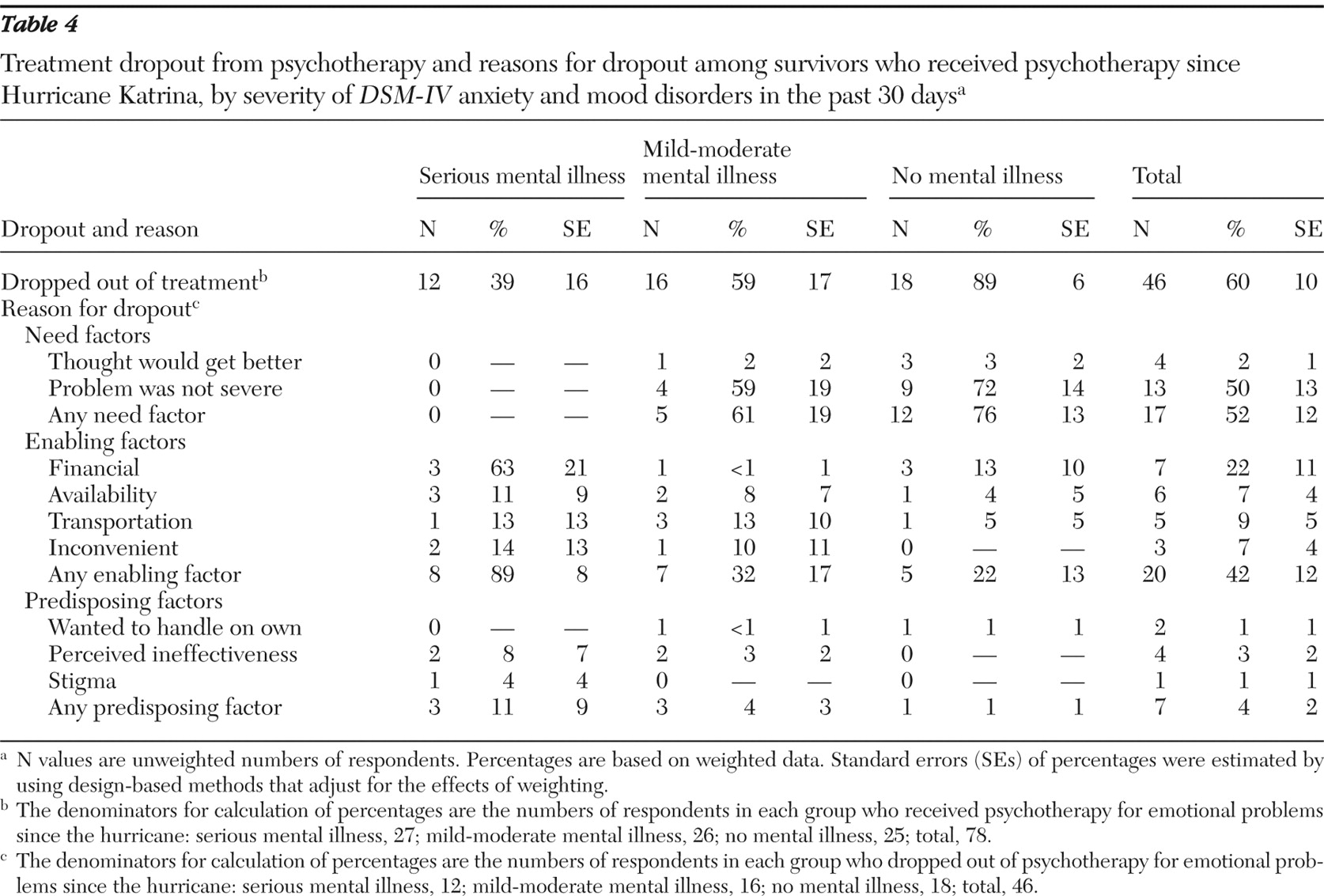
As
Table 4 shows, 60% of respondents who had used psychotherapy since the disaster had dropped out of psychotherapy by the time of the interview; the proportion ranged from 39% of those with serious mental illness to 89% of those with neither serious nor mild-moderate mental illness. Among respondents who had dropped out, lack of enabling factors was a reason for 42%; the proportion ranged from 89% of those with serious mental illness to 22% of those with neither serious nor mild-moderate mental illness.
Low need was reported as a reason for dropout by 52%; the proportion ranged from none of those with serious mental illness to 76% of those with neither serious nor mild-moderate mental illness. Attitudinal or predisposing factors were reported by 4%; the proportion ranged from 11% of those with serious mental illness to 1% of those with neither serious nor mild-moderate mental illness.
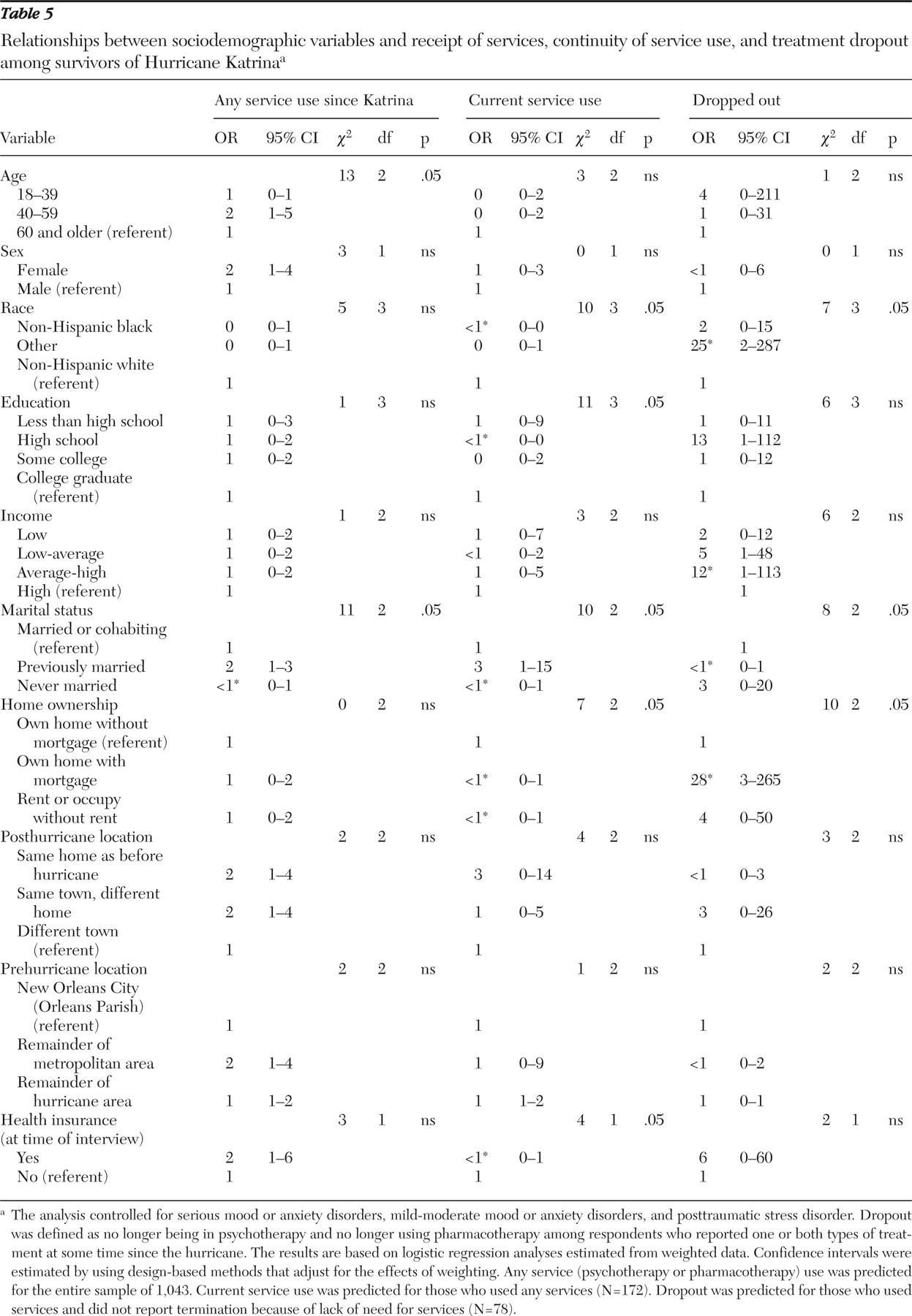
Predictors of receiving treatment and dropping out
Table 5 presents data on predictors of receipt of services. After clinical variables were controlled for, significant predictors of receiving any treatment among all respondents included being middle-aged (compared with being older or younger) and being married at some point in one's life. Significant predictors of being in treatment at the time of the interview included being white, married at some point, having low or high levels of education, owning one's home without a mortgage, and having health insurance after the disaster.
Among respondents who had received any services since the disaster, significant predictors of dropping completely out of treatment (that is, no longer receiving any psychotherapy or pharmacotherapy) by the time of the interview included being of Hispanic or "other" race-ethnicity (that is, neither non-Hispanic white or non-Hispanic black), never being married, and home ownership with a mortgage.
Discussion
Results from this geographically representative survey of Hurricane Katrina survivors conducted between five and eight months after the disaster indicate that less than one-third of those with active anxiety or mood disorders received any form of mental health care after the hurricane. Although respondents with more severe disorders tended to use more mental health services, more than half of the respondents with the most severe disorders received no mental health care. Large proportions of those who used services received treatments of low intensity or frequency. Of those who did manage to access services at some point after the disaster, more than half dropped out of treatment by the time of the survey interview.
The limited data available on mental health service use after disasters corroborate our findings. Among evacuees living in Louisiana FEMA shelters, parents reported difficulties finding appropriate and accessible mental health services for both themselves and their children with mental health needs (
21 ). Use of mental health services has been surprisingly low even after disasters that were not marked by large-scale displacement or extensive destruction of infrastructure (
22,
23,
24 ). For example, after the September 11, 2001, terrorist attacks in New York, where the service infrastructure remained largely intact, only 11.3% of people with a mental disorder received any psychiatric help and only 26.7% of those with the most severe psychiatric symptoms obtained treatment by three to six months (
25 ). Only 15% of those directly affected and 36% with probable posttraumatic stress disorder (PTSD) or depression sought mental health care by six months (
26 ).
Our findings may not be surprising given that Katrina struck people who before the disaster were among the poorest in the nation, many of whom were members of racial or ethnic minority groups. Although people with lesser means and those from minority groups are at higher risks of psychological sequelae from disasters, they are underserved when it comes to their mental health care needs (
27,
28,
29,
30 ). Furthermore, after the disaster there was widespread loss of mental health care facilities, treatments, and personnel. In addition, because of loss of employment many people lost financial resources and insurance to pay for care. For example, according to estimates made soon after the disaster, there were only two psychiatric beds available in all of New Orleans and its surrounding suburbs (
13,
31,
32 ).
In addition, many individuals with mental disorders have a low perceived need for treatment, while others recognize their need for treatment but avoid mental health care for fear of reexperiencing painful memories. Others avoid treatment because of the perception that mental disorders and treatment are associated with high levels of stigma (
33,
34 ). These attitudinal barriers appear to have caused many Katrina survivors with access to treatments to leave their mental disorders undertreated. The negative consequences of this widespread unmet need are uncertain but presumably large; dysfunction, morbidity, and mortality are associated with untreated mental disorders, and even subthreshold PTSD symptoms have been associated with poor functioning and suicidality (
35,
36 ).
Most Katrina survivors relied on the general medical sector for mental health care, which emphasizes the importance of ensuring that primary care personnel can deliver high-quality mental health treatments in disaster settings. On the other hand, the specialty sector played a large role, especially in the care of those with the most serious illness, indicating the need to have specialty personnel as well as coordinated triage plans during future disasters. Pharmacotherapy was the most commonly used modality, suggesting that current initiatives, such as the Strategic National Stockpile of emergency medications, include frequently used psychotropic classes (
37 ). Although psychotherapy was a less commonly used modality, it does appear to play an important role in the care of those with serious disorders and in promoting treatment continuity, especially in combination with pharmacotherapy.
Other correlates of service use were generally consistent with those found in previous research, including the few studies of disaster survivors. Lower service use by young and elderly persons may be attributable to the greater dependence of younger individuals on others to access treatments and on the greater stigma of mental disorders and treatments in older populations (
22,
38,
39,
40,
41 ). People who were never married may lack social supports needed to initiate or remain in treatments (
22,
25 ). Individuals of modest means, as reflected by middle levels of education and home ownership, may be at greatest risk of undertreatment—not only do these persons have fewer resources to pay for treatments but they also do not qualify for entitlements reserved for the severely disadvantaged population (
26,
42 ). Finally, we found that having insurance was associated with continuing in mental health treatments, which is similar to findings among persons affected by the World Trade Center disaster (
23 ). This finding is worrisome given that 20% of the nonelderly population in Louisiana and Mississippi were uninsured before Katrina and this proportion swelled after the disaster because of job losses (
31,
32,
43,
44 ).
These results should be interpreted with several limitations in mind. The survey excluded people who were unreachable by telephone, which led to underrepresentation of the most disadvantaged and possibly most severely ill people. Systematic survey nonresponse or nonreporting are also possible and may have led to underestimates of unmet needs for mental health treatments (
18,
45,
46,
47,
48,
49 ). Psychopathology was assessed using a brief screening scale rather than a clinical interview; however, good concordance with clinical interviews has been consistently documented in published reports (
17,
18 ). Furthermore, we considered only survivors with active psychopathology after Katrina; how the disaster may have affected the particularly vulnerable subgroup of persons who had predisaster mental disorders requires further study. Without corroborating data we do not know the validity of the self-reported data on treatment use; some investigators have found that self-reports of mental health service use overestimate treatment, especially the number of visits and especially among respondents with more distressing disorders (
50,
51 ).
To reduce respondent burden, we did not ask extensive questions about service use or potential barriers to help seeking. We thus were unable, for example, to distinguish between social worker visits in the specialty mental health care sector and those in the human services sector, although this is unlikely to have materially affected our findings given the small number of respondents who reported making social worker visits. Likewise, the extent to which specific attitudes may have deterred treatment seeking is unclear; for example, older adults may hold an altruistic view that services should be reserved for younger survivors. Finally, the survey's cross-sectional nature prevents us from concluding that the observed correlates and reasons are causally related to mental health service use.
Experiences with Hurricane Katrina have shown that many survivors with mental disorders fail to receive needed treatments in the aftermath of complex disasters (
52 ). On the basis of such lessons, what can be done to meet the needs of survivors of future disasters and to deal with financial, structural, and attitudinal barriers to mental health care? Informational resources on disaster-related mental disorders and their treatment, such as those developed by the Centers for Disease Control and Prevention, the Substance Abuse and Mental Health Services Administration, and other organizations, should be provided and promoted, but clearly these alone will not be sufficient (
53 ).
To help survivors pay for treatments, emergency insurance coverage, such as Medicaid waiver programs enacted after the World Trade Center disaster and by 17 states for Katrina survivors, may be essential (
43,
54 ). Local personnel could be organized to provide crisis counseling and referrals as in Project Liberty after the World Trade Center terrorist attacks but only in areas where clinicians and infrastructure remain (
55 ). Emergency mental health units could be stationed in devastated areas, as has been done in Operation Assist in Louisiana and Mississippi (
21 ). However, novel strategies may be necessary to reach widely dispersed populations of evacuees; for example, personnel outside affected areas could be employed to remotely deliver services such as cognitive-behavioral therapy over the telephone (
56 ).
All strategies chosen should anticipate and address common attitudinal barriers among survivors that can undermine programs in which services are only passively made available (
42 ). Screening and aggressive outreach programs that have already shown promise in overcoming such barriers and enhancing mental health treatments in primary care populations may also be useful in disaster settings (
56 ).
Acknowledgments and disclosures
Preparation of this manuscript was supported by grant R01-MH-070884-01A2 from the National Institute of Mental Health, with supplemental support from the Federal Emergency Management Agency and the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. The funders had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. The views and opinions expressed in this report are those of the authors or participants and should not be construed to represent the views of any of the sponsoring organizations or agencies or the U.S. government.
Dr. Kessler has been a recent consultant for AstraZeneca International, Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, and Wyeth and has had recent research support from Bristol-Myers Squibb, Eli Lilly and Company, and the Pfizer Foundation. The other authors report no competing interests.