Emergency departments play a critical role in our nation's efforts to intervene early and effectively with children experiencing psychiatric symptoms. Estimates suggest that slightly less than 2% of all emergency department visits made for patients under age 18 are for mental health concerns (
1 ). Patterns of return need to be better characterized than is currently the case. Recidivism raises questions about the efficiency of mental health care delivery for these patients, with repeat visitors contributing to the growing number of pediatric psychiatric emergency department visits. Developing a better understanding of factors related to patients with multiple emergency department visits could lead to improvements in the delivery of mental health care in both emergency and clinic-based settings.
Previous cross-sectional studies suggest that most return visits occur within a short period. For example, 50% of return visits occur within the same month of the initial visit (
2,
3 ) and 85% occur within six months (
3 ). However, these studies had a significant methodological limitation—unequal periods of follow-up for patients enrolled in the studies—resulting in different periods in which to return.
Our analysis examined a six-month follow-up for pediatric psychiatric patients presenting to an urban, academic medical center. The goal of the analysis was to identify factors that differentiated repeat and one-time patient visitors at an index visit, as well as factors associated with returning to the emergency department.
Methods
Data collection and analysis were granted an exemption waiver by the Johns Hopkins University Institutional Review Board. Data used for analysis were from a limited data set for which patients' identities were masked. Data were collected from all admissions from July 1, 2003, to June 30, 2005, to the Johns Hopkins Hospital pediatric emergency department, situated within a large urban general hospital serving approximately 24,000 youths each year from the surrounding community, metropolitan region, and state. Data were abstracted from all cases in which patients age 18 and under were evaluated in the emergency department by child psychiatry residents. Child psychiatry residents are on call daily from 8 a.m. until 11 p.m.; no overnight coverage is provided. All child psychiatry resident evaluations were discussed with a child psychiatry attending physician at the time of the evaluation and before the final disposition.
Each consultation included a comprehensive written clinical assessment, summarized into a one-page standardized data form, used in this analysis. Data included age, gender, and race; presenting symptoms; diagnosis; patient-reported receipt of mental health services (broadly defined to include any treatment type); patient involvement with the department of social services, child protective services, or juvenile justice; receipt of special education services; history of suicide attempts or psychiatric hospitalization; and disposition. Most of the sample (335 patients, or 80%) was African American, reflecting the demographic characteristics of the hospital's surrounding neighborhood. As a result, for the purpose of analysis, race was categorized as African American or other.
During the study period (July 2003 through June 2005), 1,342 visits were made to the emergency department by patients ages 18 and younger for which a psychiatric consultation was obtained. The focus of analysis was index visits occurring anytime in 2004. The data available from July to December 2003 were used to provide a "washout period," to ensure that visits occurring during the first half of the analysis period (January to June 2004) reflected index visits. Data available from January through June 2005 were used to provide six-month follow-up for visits occurring during the second half of the analysis period (July through December 2004), which allowed for all patients in the sample to have an equal duration of follow-up. A repeat patient was defined as any patient who returned within six months of their study index visit if the index visit was not within six months of a previous visit.
In 2004 there were 634 visits to the pediatric emergency department for psychiatric consultations. Removing 36 visits made by patients who used the emergency department during the washout period left 598 visits made by 509 patients occurring in 2004. As a minority of patients (N=30) were 17 or 18 years old at the time of their index visits, a percentage may be lost to follow-up due to their receiving additional treatment as an adult, as opposed to pediatric, emergency department.
Patients who did not live in Baltimore City comprised 18% of the original study sample. Given that there was a significant association between patient residence and return (5% of noncity residents returned as compared with 19% of city residents: χ 2 =9.6, df=1, p<.01), factors related to recidivism might vary for individuals not from Baltimore City. Because there was insufficient power to conduct an analysis stratified by city, the analyses were limited to the subsample of Baltimore City residents (N=417).
Data were analyzed with Stata SE, version 9.1 (Stata Corp., College Station, Texas). Nonparametric chi squares with Fisher's exact tests were used to compare characteristics at the index visit of patients who were repeat visitors or one-time visitors. Factors associated with return were identified through logistic regression modeling procedures. Likelihood ratio tests were used to evaluate the significance of individual variables, and Pearson goodness-of-fit statistics were used to test the overall model fit.
Results
Of the Baltimore City residents who used the emergency department during the study period, 228 (55%) were male and 189 (45%) were female. The age range of the sample was four to 18 years. A total of 338 patients (83%) reported receiving medical assistance, 100 (24%) were enrolled in special education, 51 (12%) were involved with child protective services, 75 (18%) with the department of social services, and 33 (8%) with the juvenile justice system. With regard to psychiatric symptoms and service use, 263 (64%) reported being in some form of mental health treatment at the time of their visit, 195 (49%) had a history of psychiatric hospitalization, and 51 (13%) reported a previous suicide attempt.
Patients' presenting symptoms were assessed across multiple domains, and patients may have reported more than one presenting complaint. Disruptive behaviors (disruptive behavior, aggressive behavior, or homicidal ideation) were the most frequent presenting symptoms, reported by 225 patients (54%), followed by suicidal behavior (ideation, attempt, self-injurious behavior; 166 patients, or 40%). Given that illness severity was not directly assessed, variables were selected as proxies for severity: history of suicide attempt, visit being rated by the physician as "emergent" (229 patients, or 55%), more than two psychiatric diagnoses recorded for the visit (95 patients, or 23%), more than two presenting symptoms (60 patients, or 14%), and symptom duration greater than six months (240 patients, or 58%).
Seventy-nine patients (19%) were classified as repeat, with these patients having a mean±SD of 2.37±.72 visits and a maximum of five visits during the subsequent six months. Approximately 50% of patients who returned did so within one month of their initial study visit.
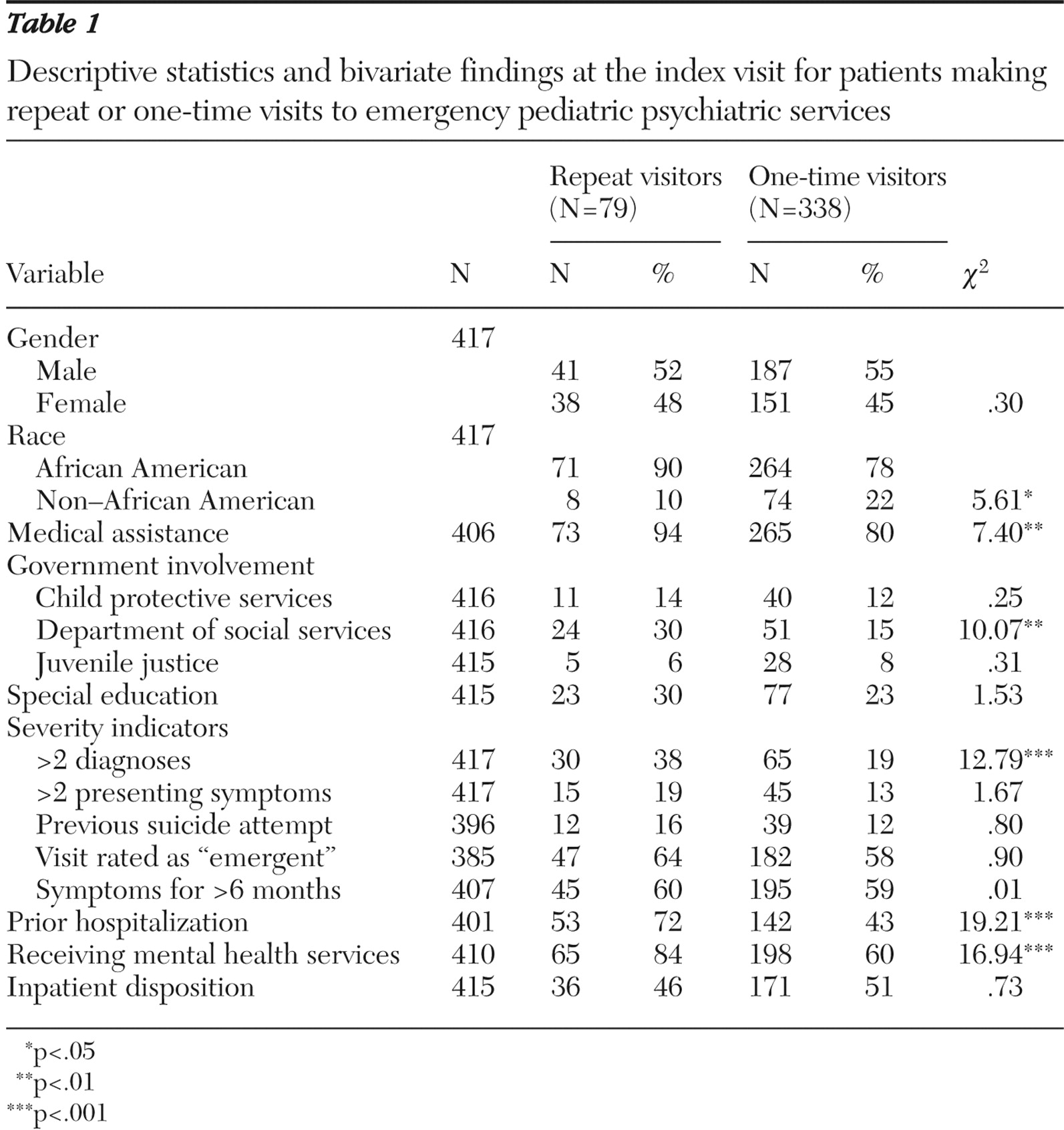
Table 1 presents the bivariate comparisons of return and one-time patients. Close to 90% of repeat visitors were African American, compared with 78% of nonrepeat visitors (
χ 2 =5.61, df=1, p<.05). Involvement with the department of social services was found to be associated with return; 30% of patients who returned were involved with these services, as compared with 15% of patients who did not return (
χ 2 =10.10, df=1, p<.01). Disruptive behavior was the only category of symptom that was associated with return in bivariate analyses; 68% of repeat patients displayed disruptive behavior as compared with 51% of one-time patients (
χ 2 =7.03, df=1, p<.01).
A higher proportion of patients who returned (72%) than patients who did not return (43%) had a history of psychiatric hospitalization ( χ 2 =19.20, df=1, p<.001). A greater proportion of return visitors (84%) than nonreturn visitors (60%) were involved in mental health treatment at the time of the index visit ( χ 2 =16.9, df=1, p<.001). Inpatient disposition from the emergency department did not differentiate between the two groups. Of all patients (repeat and nonrepeat) who were not hospitalized, 151 (72%) were referred to an outpatient mental health center, 45 (22%) to a mobile crisis service, nine (4%) to the custody of an agency, and four (2%) had a disposition of "other" (patients eloped, left against medical advice, or were admitted for medical care). Diagnostic comorbidity was the only severity indicator variable that was significantly associated with return; 38% of repeat patients were coded as having more than one diagnosis in comparison with 19% of those who did not return ( χ 2 =12.79, df=1, p<.001).
Bivariate logistic regression models were used to determine which covariates were most associated with the outcome of six-month return to the emergency department. [Table 2, which is included as an online supplement at ps.psychiatryonline.org, presents the final model.] The relationship between age and the log odds of returning to the emergency department was not linear; the probability of returning to the emergency department tended to increase for patients up to age ten, then decrease after age 15. For the purpose of analysis, age was divided into quintiles. There was little difference in the likelihood of returning for children in the first through third quintiles, but as children get older, they appear to become less likely to return. None of these effects were statistically significant. Insurance status was also a nonsignificant covariate. Gender was not included in the model because it was not hypothesized to be associated with returning to the emergency department, and there were no findings from the initial bivariate analyses to suggest that it should be included.
Results of logistic regression models showed significant associations between mental health service use and return to the emergency department. Patients who at the time of their emergency department visit reported that they were also receiving mental health services had increased odds of returning in comparison with those not receiving mental health services (odds ratio [OR]=2.63, 95% confidence interval [CI]=1.29–5.35). A history of psychiatric hospitalization was associated with return (OR=2.52, CI=1.35–4.69), as were suicidal (OR=2.04, CI=1.06–3.92) and disruptive behaviors (OR=2.85, CI=1.21–6.70) and having more than two diagnoses (OR=2.01, CI=1.08–3.72). Given that in a main effects model hospitalization was associated with decreased odds of returning to the emergency department, interaction effects between hospitalization and different presenting symptoms were included to see whether this was a general effect or specific to a symptom group. A significant interaction effect was found between inpatient disposition and the presenting symptom of disruptive behavior. For patients presenting with disruptive behavior, hospitalization at the index visit was associated with decreased odds of returning to the emergency department in the short term (OR=.29, CI .09–.92). This effect was not found for suicidal behaviors.
Discussion and conclusions
The goals of the analysis were to describe patterns of emergency department use and to identify factors that differentiated pediatric psychiatric patients who were repeat or one-time visitors at their index visit to an urban emergency department. Concurrent or past involvement in treatment, prior hospitalization, connection to social services, and disruptive and suicidal behaviors were associated with repeated use of the emergency department.
There are several possible explanations for the finding that repeat visitors to emergency services were patients already connected to services. Returning patients may have more severe cases of illness, which may include involvement in social services, receipt of mental health treatment, and history of psychiatric hospitalization as indicators of disease severity. Alternatively, the issue may not be severity at the time of contact but the nature of the underlying disorder. As with other chronic illnesses (for example, asthma), psychiatric patients may seek outpatient care for predictable illness episodes but seek care in the emergency department to manage new episodes or crisis situations.
Half of the current sample received a disposition of inpatient hospitalization, and 46% of the sample reported a history of psychiatric hospitalization. Although some repeat visits and hospitalizations may be clinically indicated, it also is possible that the patterns observed reflect deficiencies in the existing system of services. A recent study of Maryland psychiatric hospital readmissions after the initiation of a Medicaid managed care plan found that adolescents were more likely to be readmitted after the start of the managed care plan than before the reforms (
4 ). One possible explanation is that the community-based service alternatives are not available, accessible, or adequate (in terms of lack of crisis intervention, mobile treatment, and family support) or that inpatient admission is an easier disposition from the emergency department. The emergency department may be a step on the path toward readmission. In the current analysis, inpatient hospitalization protected against return in the short term. It did not, however, prevent return, nor did it clarify the purpose of the hospitalization.
When the analysis was limited to city residents only and when it controlled for payer type, African-American patients continued to have higher odds of returning than all other patients, although this may reflect proximity of the hospital for patients living near the hospital (East Baltimore, Maryland). Snowden and colleagues (Snowden L, Catalano R, Shumway M, unpublished manuscript, 2007) investigated racial disparities as they relate to use of psychiatric emergency services in California's public mental health system and found that African-American children have a greater probability than Caucasian children of using a hospital-based crisis stabilization program and a community-based crisis intervention service. Snowden and colleagues concluded that these children were at greater risk of "revolving door" use of the emergency department. Residing in impoverished neighborhoods and its associated stressors, as well coming from families experiencing multiple problems, may put minority children at increased risk of using psychiatric emergency services (Snowden and colleagues, unpublished manuscript, 2007).
Although this study has identified some important challenges to the U.S. system of care, we recognize that the study is limited because findings are based on patients presenting to a single academic medical center in an urban neighborhood and may not generalize to other emergency departments. Data concerning earlier admissions were available from only the hospital being studied, and it is possible that some "incident" visits were misclassified because earlier visits were at another institution. Finally, there was no direct measure of disease severity. Although diagnostic comorbidity was associated with return to emergency services, the accuracy of this variable is questionable, given that the evaluation was not meant to be diagnostic and rule-out diagnoses were included on the data collection sheet.
Additional research is required if we are to understand how emergency departments can best assist communities in developing systems of care. It is possible that the more intensive services (the repeated visits) may be overutilized as strategies for patient management. Future research should explore diagnostic issues and illness severity among these patients and further examine the match between the services provided and the youth and families' needs. Chronic use of the emergency department may be an indicator for either insufficient or inappropriate outpatient mental health care.
Acknowledgments and disclosures
This work was conducted while Dr. Goldstein was a postdoctoral fellow at the Johns Hopkins Bloomberg School of Public Health and was supported by grant 5T32-MH019545 from the National Institute of Mental Health to Dr. Leaf, through which Dr. Goldstein was funded. The views expressed are the opinions of the authors and not those of the National Institute of Mental Health, the National Institutes of Health, or the federal government.
The authors report no competing interests.