Type 2 diabetes, the sixth leading cause of death in the United States, affects approximately 17 million adults (
1 ) and is associated with annual medical expenses exceeding $132 billion (
2 ). Type 2 diabetes is associated with a two- to fourfold increased risk of major cardiovascular events. The long-term cardiovascular and cerebrovascular complications of type 2 diabetes account for between 60% and 75% of deaths from this disease (
3 ). Individuals with schizophrenia and other serious mental illnesses have higher rates of type 2 diabetes compared with the general population (
4,
5,
6 ), and their life expectancy is approximately 20% lower than that of the general population (
7 ), with much of the excess mortality attributed to higher rates of cardiovascular disease (
8 ).
Persons with serious mental illness have several risk factors and behaviors that likely influence both intermediate and long-term diabetes outcomes. These include a sedentary lifestyle, obesity, poor diet, and high smoking rates (
9,
10,
11,
12 ) and receipt of second-generation antipsychotic agents (
13 ). For example, our previous studies of diabetes outcomes among persons with serious mental illnesses (
14,
15 ) found that they had glycosylated hemoglobin (HbA1c) values that exceeded those recommended by the American Diabetes Association (
16 ). We also found that persons with serious mental illness and diabetes fell short of meeting recommended goals for cholesterol levels and adequate blood pressure control (
15 ).
Although the burden of diabetes can be reduced by receipt of regular medical care, the quality of diabetes care remains suboptimal for the general population (
15 ). Previous studies have also documented poor adherence to nationally recommended diabetes quality-of-care measures for several subpopulations, including elderly persons, economically disadvantaged persons, ethnic minority groups, and persons from rural areas (
17 ). However, less is known about the quality of diabetes care provided to persons with serious mental illness.
Four published studies that have limited generalizability have examined the quality of diabetes care for persons with serious mental illness (
17,
18,
19,
20 ). Three were conducted in the Department of Veterans Affairs (VA), which has an integrated somatic and psychiatric health care system that is not reflective of other less integrated community-based systems. The first of these studies compared the quality of diabetes care received by veterans with a wide range of mental disorders and by veterans without mental disorders (
18 ). It found that although indicators of quality were higher than national benchmarks for both groups, veterans with mental disorders (particularly substance use disorders) were less likely to receive recommended retinal and foot examinations. However, the authors did not find consistent evidence that patients with a serious psychiatric illness (major affective, psychotic, or posttraumatic stress disorders) were at greater risk of poorer quality of diabetes care.
The second study also compared the quality of diabetes care among veterans with and without mental health conditions (
19 ). Failure to meet diabetes performance measures, including HbA1c testing, retinal eye examination, and cholesterol testing, was more common among patients with mental health conditions. Results from this study showed disparities in quality of care after case-mix adjustment; disparities were more pronounced among those with specific conditions, including psychotic disorders, bipolar illness, substance use disorders, and personality disorders. This study also found that veterans with mental illnesses were more likely to evidence poor glycemic and lipemic control.
The third and most recent study, drawing on large national samples of VA patients who had diabetes and a serious mental illness and patients who had diabetes but no diagnosis of mental illness, found that both groups were equally likely to have their HbA1c, low-density lipoproteins, and cholesterol measured (
20 ). Notably, patients with serious mental illness had more primary care and medical specialty visits and made more multiclinic visits, including visits to both primary care and mental health services on the same day, than those without mental illness, leading the authors to conclude that the absence of differences in the quality of diabetes care observed between groups was likely attributable to increased levels of contact that were made readily available within an integrated medical and mental health service system such as that of the VA.
The single study that focused on non-VA community-based delivery of care was a retrospective analysis of administrative claims data from Blue Cross/Blue Shield of Iowa comparing diabetes care for adults with and without mental disorders (
17 ). Although persons with a coexisting mental disorder had greater numbers of diabetes-related medical visits than participants without mental conditions, they were less likely to have received HbA1c and cholesterol testing. Receipt of a dilated-eye examination and urine protein test, however, were similar for both groups. Overall quality of diabetes care for both groups was poor, with few patients (less than 6%) in either group receiving care that adhered to all guidelines of the American Diabetes Association. Although this study included a more heterogeneous sampling of service systems than the VA-based studies, it relied on claims data, which is often limited by undercoding of mental disorders. In addition, this study focused only on individuals with private insurance and was conducted only in Iowa, which is a racially homogeneous state.
In the study reported here, we compared the quality of processes of care for type 2 diabetes delivered to adults with serious mental illness and co-occurring type 2 diabetes and to patients with type 2 diabetes and no serious mental illness. The patients were receiving care in a range of community-based clinic settings. Unlike the studies described above, which relied on large administrative databases, our study used individual review of medical chart data as its primary source of data. Although both methods have limitations (
21 ), there is evidence to suggest that chart review data are as reliable as data abstracted from administrative sources (
22,
23 ). We relied primarily on the quality-of-care processes referenced in the Diabetes Quality Improvement Project (DQIP) (
24 ). The American Diabetes Association and the National Committee for Quality Assurance, as well as other organizations, developed the DQIP to provide a comprehensive set of performance measures for diabetes care.
Although the DQIP includes quality-of-care measures related to both processes of care and immediate outcomes, we focused on processes of care; our previous work already documented the extent of poor intermediate outcomes of diabetes care among our study participants (
14,
15 ). We acknowledge that a host of patient, provider, and environmental factors likely contributed to the poor intermediate disease outcomes reported. However, our intention was to examine the important role of service delivery in affecting the quality of care of patients with serious mental illness and type 2 diabetes. Additionally, we compared the two groups on self-reported receipt of provider-delivered diabetes education, an additional quality-of-care indicator that is being field tested as a part of the DQIP. Finally, we compared the groups on self-reports of receipt of diabetes self-care cues from providers. We hypothesized that persons with serious mental illness would receive poorer quality of diabetes care than those without serious mental illness.
Methods
Study setting and sample
Data were collected as part of a cross-sectional study of 300 nongeriatric adult patients with a current diagnosis of type 2 diabetes in their medical or psychiatric records. A total of 201 participants had a serious mental illness (100 had schizophrenia and 101 had a major mood disorder), and 99 had no serious mental illness. Participants with serious mental illness were recruited from six public and private outpatient mental health clinics in urban and suburban communities across the Baltimore metropolitan area. The sample represented a broad range of individuals receiving psychiatric services for serious mental illness. Serious mental illness diagnoses were obtained from the psychiatric chart.
Participants without serious mental illness were recruited from three primary care clinics located near the psychiatric clinics in order to identify patients who had demographic characteristics similar to those of the participants with serious mental illness. To reach this goal, all patients with a diagnosis of type 2 diabetes were identified from appointment logs. Primary care providers next asked potential participants whether they were willing for to be screened for study eligibility by research staff. On the basis of this screening procedure, those who had received any treatment for a psychiatric disorder within the past year, including antidepressant medication, were excluded.
One-fourth of the total sample from each group consisted of veterans recruited from the Baltimore VA Medical Center. Additional details regarding the recruitment and description of participants have been published elsewhere (
14 ). The institutional review boards of the University of Maryland School of Medicine and of each participating facility approved the study.
Although diabetes care was provided to study participants in more than 50 medical settings, the majority of care was delivered in a small number of similar hospital- and community-based primary care clinics. Specifically, 73% of the sample (N=220) received diabetes care in this type of setting. By design, virtually all patients in the group that did not have serious mental illness (96 of 99) received care from this type of primary care clinic, as did 62% (N=124) of the group with serious mental illness. The remaining 80 patients (27%) received diabetes care either at specialty settings (13 patients), from private providers (36 patients), from psychiatric providers (nine patients), in emergency departments (17 patients), or at unclassifiable sites (five patients).
Procedure
After receiving a full description of the study and providing written informed consent, each participant met with research staff for a 2.5-hour assessment. Assessments were conducted between September 1, 1999, and September 30, 2002. Participants signed a medical release of information form to allow access to their medical records that contained information on their diabetes care for the year preceding the research assessment. In all, charts for 270 patients (90% of the total sample) were reviewed. Of the 30 missing charts, 21 were for those with serious mental illness and nine were for those without serious mental illness. On-site chart reviews were conducted at the VA and the university outpatient primary care clinic. For the other sites, photocopies of medical records were sent to us in response to written requests.
Measures
Quality-of-care indicators. Medical chart records were reviewed to determine whether in the past year participants received six services recommended by the DQIP (
24 ): HbA1c testing, retinal eye examination, foot examination, blood pressure measurement, urine protein testing, and lipid assessment. We also created two summary variables: whether all six performance measures were met and the total number of performance measures met. If it was not possible to determine whether a quality-of-care criterion was met, it was coded as missing and not included in calculating whether the performance measure was met. The extent of missing data across the quality-of-care criteria ranged from 12% to 14%. Approximately 10% of the records were rated by two raters, with greater than 90% agreement across raters.
Education and cues. Participants provided self-reports of receipt of any form of diabetes education during the past six months, as described in DQIP field tests (
24 ). Cues to diabetes care were derived from specific questions about whether health care workers reminded them to adhere to diet, exercise, medication, and glucose-monitoring recommendations—for example, "In the past month, have any of your health care workers reminded you to check your (sugar) blood glucose?" Only participants reporting current cigarette use were asked if they received tobacco counseling.
Statistical analyses
Demographic and clinical characteristics of patients with and without serious mental illness were compared by using Pearson chi square tests for categorical variables, independent t tests for normally distributed continuous variables, and Wilcoxon two-sample tests for skewed continuous variables. Next, for each of the quality-of-care indicators, we calculated the percentage of patients with chart-documented receipt of the service within the past year. Multiple logistic regression models that controlled for age, gender, race, education, duration of diabetes, and current use of insulin were used to compare the six indicators of quality of diabetes care between patients with and without serious mental illness.
Because the recruitment strategy used for the parent study was not designed with regard to locus of diabetes care, our analyses for this study were conducted first for the full sample (N=300) and then again only for those receiving care in similar primary care hospital- and community-based clinics (N=220). Multiple regression models were used to compare the quality-of-care index variable between groups with use of the same covariates listed above. The same series of multiple logistic regression analyses were used to compare receipt of diabetes education and cues in both the full and restricted samples.
Results
Sample description
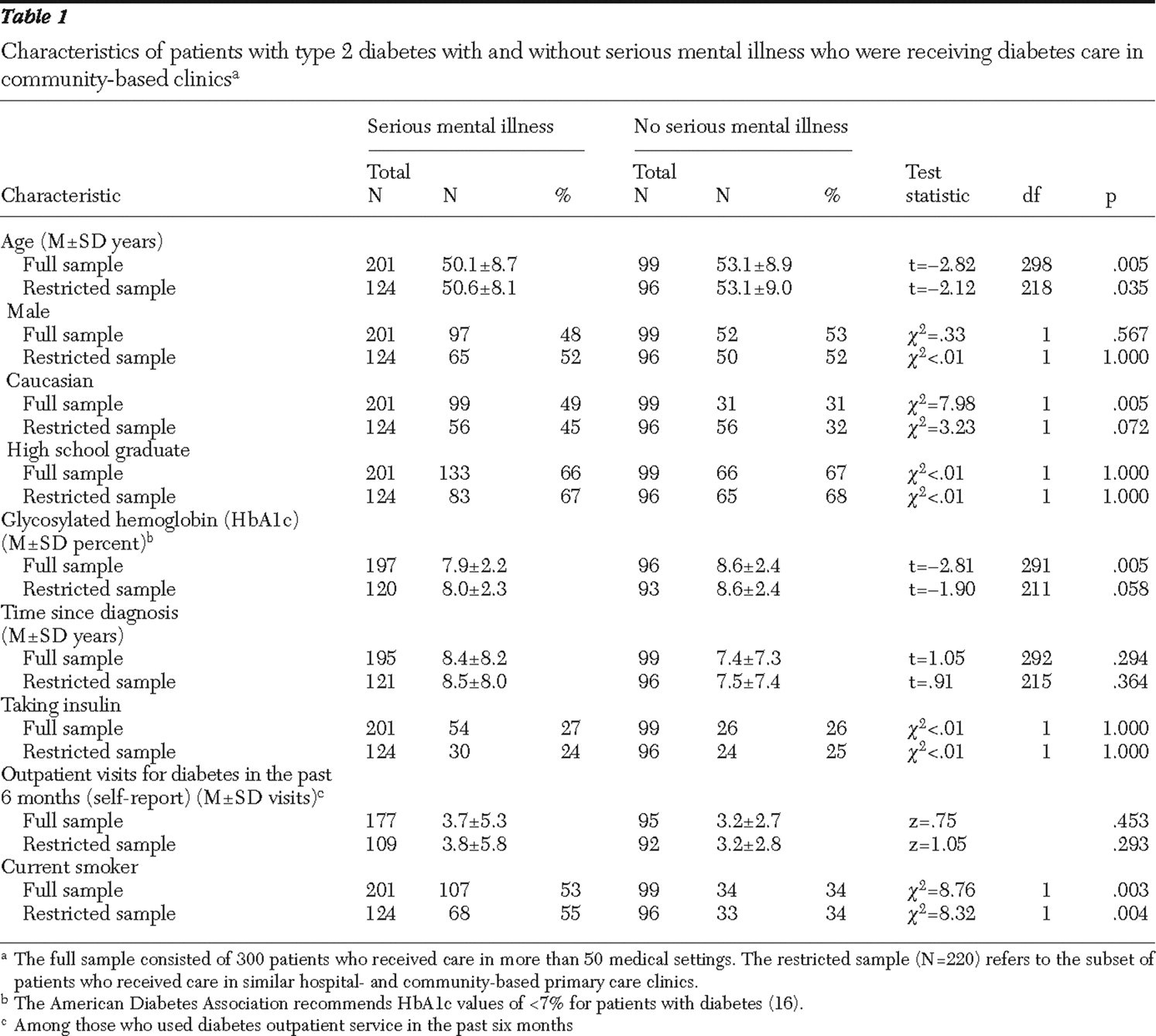
In the full sample, persons with serious mental illness did not differ from those without mental illness in gender or education. However, as
Table 1 shows, the former group was younger (difference in mean age of three years) and more likely to be Caucasian (49% compared with 31%; p=.005). Although HbA1c values for both groups exceeded those recommended by the American Diabetes Association (
16 ), the group with serious mental illness had significantly lower HbA1c values, as previously reported (
14 ). However, no differences were found between groups in length of time since diabetes diagnosis, proportion receiving insulin, and numbers of diabetes-related outpatient visits in the past six months. Rates of current smoking were significantly higher in the group with serious mental illness (53% compared with 34%).
For the restricted sample of 220 patients who were receiving services in hospital- and community-based primary care clinics, the group with serious mental illness was also younger (difference in mean age of 2.5 years) but not significantly different from the group without mental illness on any other patient or service variables. For this restricted-sample analysis, rates of smoking were also significantly higher in the group with serious mental illness (55% compared with 34%).
Quality of processes of diabetes care
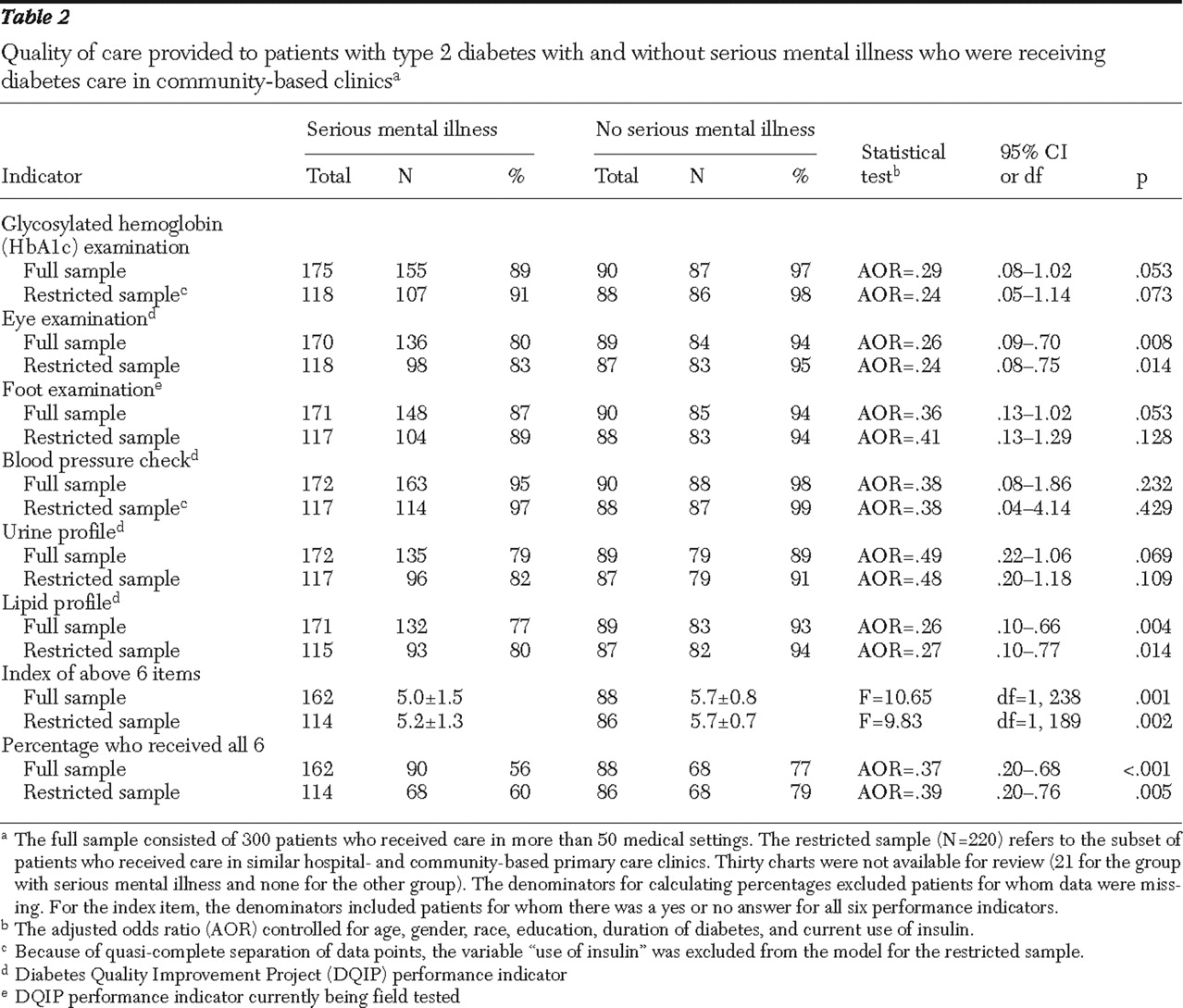
For the full sample, the group with serious mental illness received significantly fewer of the six recommended services than did the comparison group. As shown in
Table 2, persons with serious mental illness in the full sample were also less likely to meet all six performance measures (56% compared with 77%) and less likely to meet recommended performance measures regarding receipt of a retinal examination (80% compared with 94%) and lipid profile analysis (77% compared with 93%).
In the restricted sample patients with serious mental illness also received significantly fewer of the six recommended services and were less likely to meet all six performance measures (60% compared with 79%). Regarding specific performance measures, the restricted serious mental illness group was significantly less likely than those without mental illness to meet performance measures regarding receipt of a retinal eye examination (83% compared with 95%) and a lipid assessment (80% compared with 94%)
Diabetes education and cues
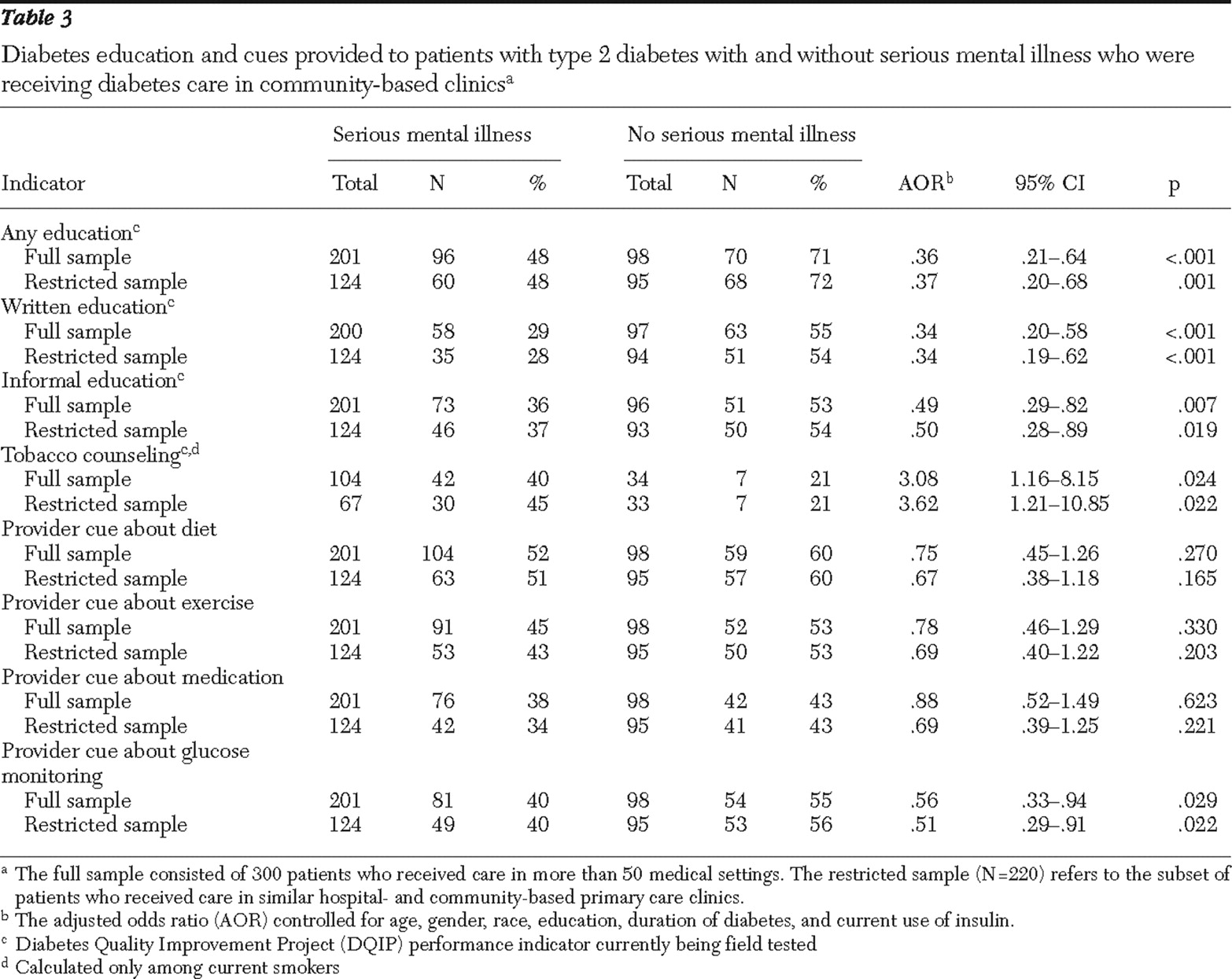
For both the full and restricted samples, patients with serious mental illnesses were significantly less likely to meet DQIP field-tested performance measures for receipt of any type of diabetes education, including any offered in either a written or a more informal format (
Table 3 ). However, current smokers with serious mental illness in both sets of analyses were significantly more likely to meet the performance measures for tobacco counseling. Analyses for both the full and restricted samples indicated that those with serious mental illness were less likely to receive cues from providers about glucose monitoring. No differences between the groups were found in receipt of cues from providers about adherence to diet, exercise, and medication.
Discussion
The results of this investigation replicated those of previous studies suggesting that persons with serious mental illness and type 2 diabetes receive poorer quality of diabetes care than persons with type 2 diabetes who do not have mental illness (
17,
19 ). However, the study differed from two of the VA-based studies (
18,
20 ), which found no differences between those with and without serious mental illness. Unlike these two studies, which were conducted in a health care system in which psychiatric and somatic medical services are integrated, our study extends previous findings by focusing on a more demographically heterogeneous sample of patients and on care received in community primary care settings.
The disparity in quality of diabetes care between groups was most prominent in terms of the likelihood of meeting the full set of performance measures related to care processes and the likelihood of receiving education about diabetes. The disparities were found for both the full sample and for the restricted sample that received care in similar hospital- and community-based primary care clinics. Notably, the performance measure that was more frequently met among patients in the serious mental illness group—receipt of smoking cessation counseling—was likely a response to the markedly higher rates of smoking in this group and may reflect greater sensitivity among providers to smoking rates for those with serious mental illness.
Overall, our findings suggest that although limited access to care may be problematic for some persons with serious mental illness (
25,
26,
27,
28 ), even patients with documented access to care and receipt of diabetes services, such as those in our study, may receive poorer quality of care than those without serious mental illness who also have such access.
Our previous study of patients in this sample found that those with serious mental illness were less likely than diabetes patients without serious mental illness to be prescribed cholesterol-lowering statin medications, angiotensin-converting enzyme inhibitors, and angiotensin receptor-blocking agents, which are treatments demonstrated to reduce cardiovascular events among patients with diabetes, reflecting less aggressive treatment for cardiovascular risk in the group with mental illness. In that study, we also observed that those with serious mental illness fell short of meeting goals recommended by the American Diabetes Association for cholesterol levels and adequate blood pressure control (
15 ). Our finding in the study reported here that persons with serious mental illness were also less likely than those without mental illness to receive recommended annual lipid testing parallels our previous findings and raises serious concerns given this population's known elevated risks of morbidity and mortality related to cardiovascular disease (
8 ).
Moreover, recent findings of an analysis of baseline data from participants in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study echo these concerns by suggesting that suboptimal management of cardiovascular risk extends well beyond patients with serious mental illnesses and a co-occurring diagnosis of diabetes. Specifically, Nasrallah and colleagues (
29 ) reported that among CATIE participants with elevated fasting lipid levels, 88% were not receiving lipid-lowering medications and of those meeting criteria for hypertension, 62% were not receiving any hypertensive medications.
Because antipsychotic medications are an important component in the management of many serious mental illnesses, and given the fact that the increased use of second-generation antipsychotic medications has been associated with reports of dramatic weight gain and derangements in both glucose and lipids (
13,
30,
31,
32 ), the American Diabetes Association, the American Psychiatric Association, the American Association of Clinical Endocrinologists, and the North American Association for the Study of Obesity convened and released a consensus statement calling for careful baseline and follow-up monitoring of weight, body mass index, waist circumference, blood pressure, fasting plasma glucose, and fasting lipid profiles for individuals receiving antipsychotic medications (
30 ). The results from both the recent CATIE study (
29 ) and our own work emphasize the need for increased monitoring and treatment of cardiovascular risk factors among this vulnerable population and perhaps even suggest adoption of more aggressive monitoring than is currently recommended in the consensus statement.
The reasons for the differences in quality of care between patients with and without serious mental illness are not known with certainty. Hypotheses regarding variables at the patient, provider, and system levels are plausible. Although we did not aim to test mechanisms of poorer quality of care, our study provides clues to possible causes. In keeping with previous studies showing that poor communication skills compromise the quality of medical care (
28,
33,
34 ), our findings suggest that the problem may partly reside in the provider-patient interaction. We have previously reported that the patients with serious mental illness in our sample had significantly lower ratings of knowledge of diabetes and scored more poorly on a brief rating of neuropsychological functioning (
35 ). It is probable that patients with serious mental illness require more time and attention to solicit their cooperation and understanding in the provision of optimal diabetes care. These greater needs are clearly not being met, because we found that patients with serious mental illness were less likely than patients without serious mental illness to receive diabetes education and to receive cues from providers regarding the need for glucose self-management. As suggested by O'Day and colleagues (
36 ) in a recent qualitative study of perceived barriers to obtaining medical services among persons with psychiatric disabilities, these unmet needs may reflect primary care physicians' lack of knowledge about psychiatric illness and psychotropic medications. As others have noted, the possibility of discrimination or stigma on the part of medical providers toward people with serious mental illness may further contribute to the disparities in service receipt (
37,
38 ).
It should be noted that we did not analyze the data to determine whether quality of care was associated with psychiatric diagnosis. Although we considered this, we made an a priori decision to restrict our quality-of-care analyses to differences between those with and without mental illness. This decision was informed by the similarities across the two psychiatric groups in both diabetes illness outcomes (for example, similar HbA1c values and similar odds of meeting criteria for the metabolic syndrome) and diabetes service use patterns (for example, equivalent receipt of diabetes and other medical services, including receipt of cholesterol-lowering statin medications) reported in our first two published studies (
14,
15 ). Our decision was further supported by our review of the literature showing that disparities in quality of diabetes care between those with and without mental illnesses are evident across a wide range of mental disorders (
18,
19 ). Although some antipsychotic agents have been associated with negative metabolic effects (
13,
31,
32 ), we also did not analyze the data to determine whether quality of care was associated with receipt of a particular psychotropic medication. We made this decision because medication would likely be confounded with diagnosis and because such an analysis would be further precluded by the fact that our group without mental illness, by definition, was not receiving antipsychotic medication.
The implications of this study are best understood by appreciating both the adequacies and the deficiencies of diabetes care provided to persons with serious mental illness. On the one hand, the diabetes care of persons with serious mental illness fell short of that without serious mental illness, and deficiencies in monitoring of diabetes status and complications and education should clearly be remedied. On the other hand, a majority of patients received most of the required services, and of the six required services, patients with serious mental illness received a mean of about five. It is not unreasonable, then, to propose that at least for this more stable subpopulation of persons with serious mental illness, it seems sensible to build on the strengths of the current system by educating primary care providers, patients with serious mental illness, and mental health providers to promote more complete and high-quality diabetes care. It is also important to better integrate mental health and diabetes services as such efforts would likely result in improved quality outcomes.
Our study has several limitations. Our sampling strategy resulted in a somewhat different pattern of care in the sites in which patients with and without serious mental illness received diabetes services, although we attempted to adjust for this potential confound by conducting analyses for the limited sample of patients receiving care in similar treatment settings. Further, we relied on self-report of receipt of education and self-care cues, and we relied on chart records for receipt of other services. It is not possible for us to estimate the error associated with our reliance on chart records, but we have no evidence that the error would favor either of the groups (with or without serious mental illness). Strengths of the study include the representativeness and heterogeneity of the patient populations, the breadth of diabetes services evaluated, the range of providers from which patients received their diabetes care, and our use of data that extended beyond administrative claims.
Conclusions
The increased risk of type 2 diabetes and its prevalence among persons with serious mental illness underlines the importance of carefully evaluating the quality of somatic care that such patients receive in typical primary care settings. Future studies could build on the strengths observed in the service system by attempting to educate and empower patients with serious mental illness and by teaching them what to expect in their diabetes care and how to assert their need for care. Patients with greater deficits in care or greater illness-related deficits might require elements of on-site medical case management.
Acknowledgments and disclosures
The authors report no competing interests.