During the past 40 years psychotropic drugs have assumed great importance in the treatment of psychiatric disorders. Most of the psychotropic drugs used fall into one of four drug groups: antipsychotics, antidepressants, mood stabilizers, and anxiolytic-hypnotic agents.
The prevalence rates for psychotropic drug use vary widely across countries, ranging from 5.5% to 12.3% (
1,
2,
3 ). One study reported that use of second-generation antipsychotics has been increasing during the past decade (
4 ). Meanwhile, use of second-generation antidepressants has been increasing since the 1990s (
5 ). The costs and benefits of second-generation antipsychotics and antidepressants deserve further study (
6 ).
In March 1995 Taiwan implemented the National Health Insurance (NHI) program, a comprehensive, unified, universal health insurance program for all citizens of Taiwan. Up to 96% of residents of Taiwan have joined the NHI program since 1996. In this report, we used NHI data between 1997 and 2004 to examine temporal changes in the use of psychotropic agents in Taiwan. We also examined trends in the use of first- and second-generation antipsychotics and first- and second-generation antidepressants.
Methods
The National Health Research Institutes (NHRI) provided a database of medical claims from 200,432 randomly selected persons, about 1% of the population, for use in health insurance studies. These 200,432 persons were followed throughout the study period. There were no statistically significant differences in age, sex, and health care cost between the sample group and all enrollees. The data consisted of inpatient and ambulatory care records, including all health service data and prescription drug data, as well as registration files of the insured. The study was approved by the Jianan Mental Hospital Institutional Review Board.
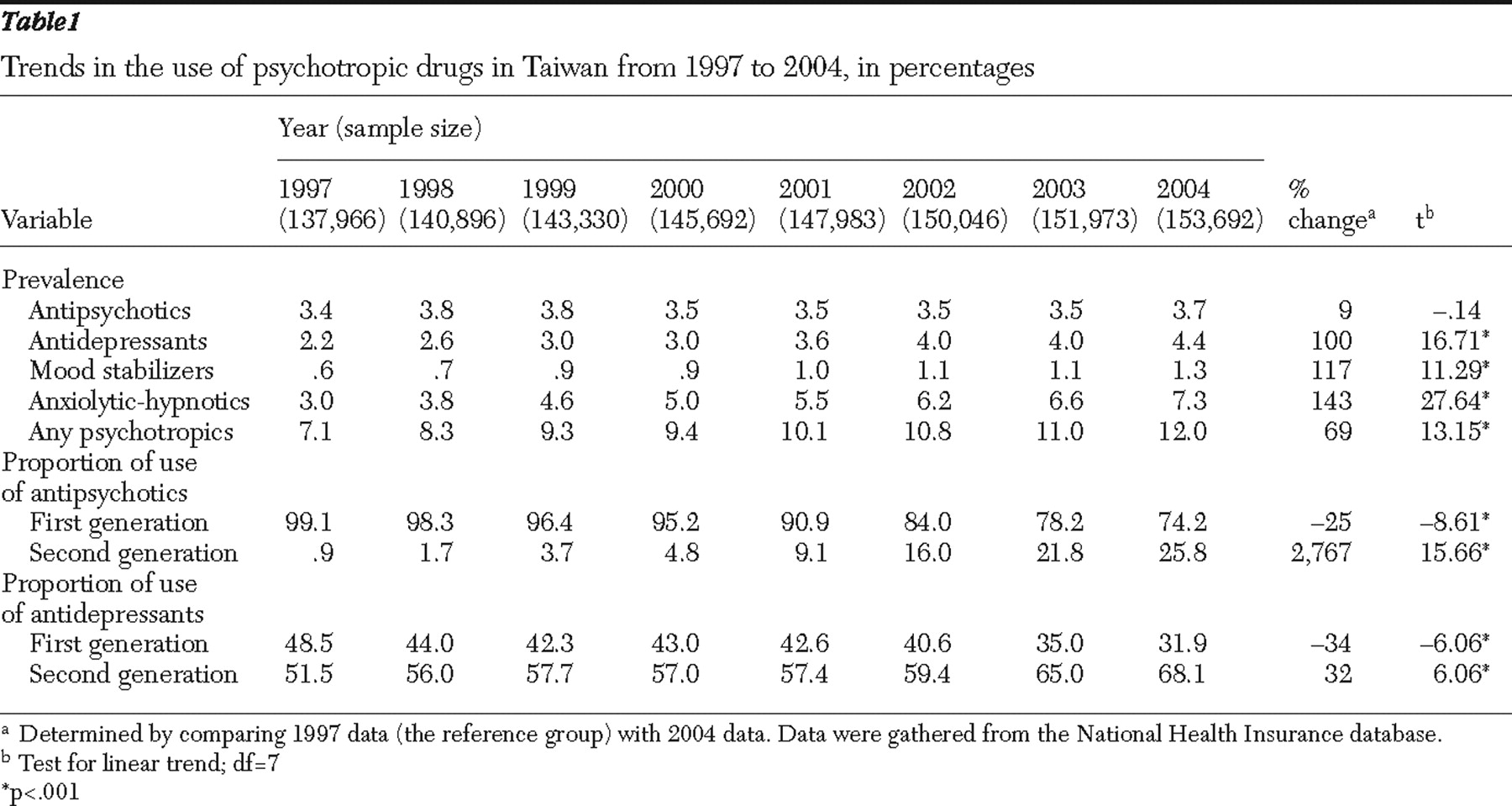
We conducted a population-based, random-sampling study by using data on psychotropic drug use from January 1, 1997, to December 31, 2004. A dynamic cohort was used in the study presented here. The persons in the study sample were limited to those aged 18 years or older on July 1 of each year, and we excluded persons who died during the course of the study. Thus 137,966, 140,896, 143,330, 145,692, 147,983, 150,046, 151,973, and 153,692 enrollees, respectively, were studied in this cohort from 1997 to 2004. These enrollees had universal access to prescription drug coverage, ambulatory care, and hospital care.
All persons who had any record of using psychotropic medications either in ambulatory care or in hospital care were identified in each year. Psychotropic drugs were recorded on the basis of the Anatomical Therapeutic Chemical (ATC) classification system (
10 ). Data presented in this brief report were limited to four main drug categories: antipsychotics (including first- and second-generation antipsychotics, such as clozapine, olanzapine, quetiapine, risperidone, ziprasidone, amisulpride, and aripiprazole), antidepressants (including tricyclics and second-generation antidepressants, such as monoamine oxidase inhibitors, serotonin norepinephrine reuptake inhibitors, and selective serotonin reuptake inhibitors, including citalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline), mood stabilizers (including lithium, carbamazepine, valproate, gabapentin, topiramate, and lamotrigine), and anxiolytic-hypnotic drugs (including benzodiazepines and nonbenzodiazepine compounds).
In this study, we examined temporal changes in the use of antipsychotics, antidepressants, mood stabilizers, and anxiolytic-hypnotic agents from 1997 to 2004. Three parameters were assessed: prevalence of use of psychotropic drugs, proportion of use of first- and second-generation antipsychotics, and proportion of use of first- and second-generation antidepressants. When we estimated the prevalence of psychotropic drug use, the denominator used was the total number of persons in the study sample in each year and the numerator was the number of persons in each year who had any record of using psychotropic medications.
Percent change was determined by comparing data from 2004 with those from 1997. Time-series analysis was performed. Linear models were used to assess trends in the prevalence of use of psychotropic drugs. Linear models were also used to assess the trends in the proportion of use of first- and second-generation antipsychotics and first- and second-generation antidepressants. The models were fit to the data by using SAS/ETS for Windows, version 9.1. In this study, the significance level was set at .05.
Discussion
There has been no report about trends in psychotropic drug use in Taiwan. Our study is the first to analyze NHI data to detect trends in the use of psychotropic drugs in Taiwan. Our results revealed that from 1997 to 2004 the prevalence of psychotropic drug use increased by 69%, from 7.1% to 12%, a finding consistent with studies showing similar increases in other countries (
5 ).
The study presented here found that the prevalence of antipsychotic use increased by only 9%, from 3.4% to 3.7% between 1997 and 2004; this increase was not significant. The prevalence of antipsychotic use in Taiwan was higher than in other countries—.7% in the United States, .5% in Canada, and 1.2% in Europe (
1,
3,
9 ). The prevalence of antipsychotic use was also higher than the treated prevalence of major psychiatric disorders in Taiwan (1.37%), which included
ICD-9-CM codes 290–298 (
11 ). One possible explanation for this discrepancy is that more people with psychotic disorders seek treatment in the NHI program; another explanation is that there may be more off-label use of antipsychotics in Taiwan. Antipsychotics may be used in the treatment of nonpsychotic disorders, including manic state without psychosis, dementia without delusion, nonpsychotic major depression, severe anxiety disorder, and severe insomnia (
12 ).
On the other hand, among persons given prescriptions for antipsychotics, the proportion of second-generation antipsychotic use increased from .9% to 25.8% between 1997 and 2004, consistent with trends in other countries (
4,
5 ). However, among persons given prescriptions for antipsychotics, the proportion of second-generation antipsychotic use in Taiwan (25.8%) was still lower than that in the United States (84%) (
4 ). Perhaps the implementation by the NHI program in Taiwan of a global budget to control health care expenditures in 2002 limited the growth of second-generation antipsychotic use. Although second-generation antipsychotics have some advantages over first-generation antipsychotics, such as causing extrapyramidal syndromes or sedation less frequently, the increased risk of metabolic effects, including diabetes, hyperlipidemia, and obesity, associated with the use of second-generation antipsychotics warrants further attention (
6 ).
Increasing trends in the rate of treatment of depression were reported in some national studies (
13 ). A 100% increase (2.2% to 4.4%) in the prevalence of antidepressant use in Taiwan occurred over the period of this study, which was consistent with a finding of trends in the United States (
13 ). The prevalence of antidepressant use in Taiwan was higher than in the United States (2.3%) (
3 ) and was close to the prevalence in Canada (4.7%) and Europe (3.7%) (
1,
9 ). The prevalence of antidepressant use was higher than the prevalence of major depressive disorder (1.14%), as determined by a community survey in Taiwan (
14 ). One reason for this difference may be that the prevalence of major depressive disorder was underestimated in the study, which was conducted in the 1980s. Another explanation is that antidepressants are used extensively for conditions other than depression; they may be used for general anxiety disorder, panic disorder, phobic state, neurotic depression, obsessive-compulsive disorder, eating disorder, migraine, or insomnia. Thus the prevalence of antidepressant use was higher than the treated prevalence (.36%) of major depressive disorder in Taiwan (
11 ). Among persons who used antidepressants, the proportion of use of second-generation antidepressants increased from 51.5% to 68.1% in Taiwan, consistent with trends in other countries (
5 ). Second-generation antidepressants may produce fewer side effects than conventional antidepressants, but more precise economic analysis is needed to justify the use of second-generation antidepressants.
The prevalence of mood stabilizer use increased by 117%, from .6% to 1.3% between 1997 and 2004, which was higher than the prevalence found in the United States (.1%), Europe (.1%), and Canada (.6%) (
1,
3,
9 ). This phenomenon could be explained by the use of different data sources and definition of drug utilization. For example, the U.S. study calculated only antimanic use, and it may have examined fewer types of mood stabilizers than other studies (
3 ). In addition, use of mood stabilizers for both psychiatric and medical conditions should be considered, including treatment of aggression, augmentation in the treatment of schizophrenia, and treatment of other medical problems (
7 ).
The prevalence of anxiolytic-hypnotic drug use increased 143% (3.0% to 7.3%) over the eight-year period. The prevalence was lower than that found in Europe (9.8%) (
1 ) but higher than that found in the United States (3.2%) and in Canada (3.1%) (
3,
9 ). The increasing trend in the use of anxiolytic-hypnotic drugs in Taiwan was due to the higher prevalence in recent years of psychiatric disorders, such as general anxiety disorder, neurotic depression, and insomnia (
14 ). However, the prevalence of anxiolytic-hypnotic drug use in the United States was based on the Nutrition Examination Survey, 1988–1994, so it would be useful to observe trends in the United States over the past decade. Moreover, to obtain accurate comparisons, we should further differentiate occasional users of anxiolytic-hypnotic drugs from chronic users (
15 ).
There are several advantages to using insurance data for the study of psychotropic drug use, including the availability of a large national database for analysis, saving of time and money needed to perform community surveys, availability of longitudinal data to detect trends in the use and cost, and avoidance of recall bias. In this study, we used a population-based random sample to prevent selection bias. However, we must consider some limitations. First, a global budget plan was thoroughly implemented in the NHI program after 2002, and this may have had a substantial effect on subsequent use of high-cost agents, such as second-generation antipsychotics. Second, the prevalence of psychotropic drug use does not reflect the actual prevalence rate of psychiatric disorders, because not all persons with psychiatric disorders seek treatment and because off-label use of psychotropics is common. Third, we need to consider more information, including psychotropic dosage, duration of psychotropic treatment, and indications for use (
9 ). Fourth, several of these mood stabilizers are also used for non-mental disorders or other medical conditions, such as migraine and diabetes-related neuropathic pain. Fifth, the different study design, sampling method, characteristics of study subjects, and observational period limit comparison with other studies. Finally, there are differences between the health care systems in Taiwan and the United States. First, the NHI program in Taiwan is a compulsory health insurance system with a high percentage of the population enrolled (96%), whereas the United States contains different public and private health insurance systems. Second, it seems that the NHI program, which has a low copayment, would encourage more persons to seek treatment, resulting in higher health service utilization.