Patients with severe mental illnesses have higher rates of common medical conditions and worse health outcomes associated with those conditions than the general population (
1,
2,
4,
5,
6,
7,
8,
9 ). Recent studies also show that patients with severe mental illnesses have high rates of HIV infection (
10,
11,
12 ) as a result of risky sexual behavior, sexual victimization, and substance abuse (
13,
14,
15,
16,
17,
18,
19,
20,
21 ), although little is known about the HIV care these patients receive or their health outcomes.
Research on patients with severe mental illnesses and medical conditions other than HIV suggests their worse outcomes partly reflect unique barriers to care and poorer quality of care. This group is at risk of worse medical care because they are often poor and unemployed and have limited or no access to health care. Also, they often have cognitive deficits and poor interpersonal skills that interfere with access to medical care and adherence to medical regimens (
20 ). For example, they may not verbalize concerns (
22,
23,
24,
25 ), or they may deny illness (
26 ), be reluctant to see doctors other than their psychiatrists (
27 ), or accept inadequate medical care (
28 ). Navigating the medical entitlement and insurance systems may be particularly difficult for patients with severe mental illnesses. These problems are often exacerbated by poor coordination between mental and physical health care systems and providers (
24 ). Thus the complexity of treatment for HIV infection, with its needs for close monitoring, tight adherence, and frequent dosing of medications, may be particularly problematic for patients with severe mental illnesses and HIV.
Given the challenges associated with severe mental illness in treating medical illnesses, we sought to examine its impact on HIV care. To do this, we examined barriers to obtaining care, experience with outpatient care, problems with hospital care, extent of disability days, and functional health status for adults with severe mental illness and HIV in public mental health clinics in Los Angeles and New York City. We then compared these observations with similar data from a sample of adults who had HIV but not severe mental illness; this sample was part of the HIV Cost and Service Utilization Study (HCSUS) (
29 ). We also conducted secondary analyses comparing subsistence needs and access to case management services between the two patient groups because these factors may contribute to differences in care and outcomes (
30,
31,
32,
33,
34,
35 ).
Methods
Study population
Adults with severe mental illnesses and HIV were recruited from publicly funded mental health agencies in Los Angeles between September 1998 and August 1999 and in New York City between August 1999 and May 2002. To identify sites that cared for patients with severe mental illness and HIV, we surveyed freestanding mental health clinics and programs intended for people with mental illness in jails, hospitals, and other facilities. We then visited the sites to determine how many patients with severe mental illness and HIV were eligible for the study and to ask providers to refer them. Severe mental illness was defined as having a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, or major depressive disorder with psychotic features. Patients whose psychiatric diagnoses were secondary to HIV or substance abuse were excluded. After explaining the study to eligible patients, informed consent was obtained. Consenting patients were interviewed, and blood samples were drawn within a few months of the interview. The study protocol was approved by local institutional review boards as well as by RAND's.
In Los Angeles, 96 agencies were contacted and responded. Forty-nine reported caring for patients with severe mental illness and HIV, but only 25 agencies had eligible patients. We identified 252 eligible patients in Los Angeles, and we interviewed 155 patients (62%) from 23 agencies. In New York City, 434 agencies were contacted. Of 199 agencies that responded, 65 reported caring for patients with severe mental illness and HIV, and 57 had eligible patients. We identified 178 eligible patients in New York City, and we interviewed 140 patients (79%) from 56 agencies.
HIV patients who did not have severe mental illness ("HIV only") were drawn from the HCSUS cohort, a national probability sample of HIV-positive adults receiving treatment (
29 ). We selected patients by using a three-stage sampling design, in which geographical areas, medical providers, and patients were sampled successively (
36,
37 ). Surveys were conducted in three waves, the last of which involved 2,267 patients (79% of the original sample) and occurred between August 1997 and January 1998. To make the timing of the interviews as comparable as possible with the other groups, we used HCSUS respondents from this final wave as our sample of HIV-only patients. Blood samples from these respondents were obtained in 1998.
Because the HCSUS sampling design was intended to produce national and regional—rather than state or regional—estimates of utilization and costs, HCSUS data are not strictly comparable with the data obtained from the two metropolitan areas. Nonetheless, the HCSUS data provided reasonable benchmarks to help identify potential disparities in access to or experience of treatment. We compared the HCSUS subsamples from the Western and Eastern regions of the United States with patients with severe mental illness and HIV from Los Angeles and New York City, respectively. Of the HCSUS respondents who participated in the second follow-up interview, 762 (35%) were from the West, and 532 (24%) were from the East.
Measures
To compare HIV care, we used items on the HCSUS already administered to that sample to interview the New York and Los Angeles patients with severe mental illness and HIV (www.rand.org/health/projects/hcsus/questionnaires.html). On the basis of results of two pilot tests, we modified some items to make them more understandable to patients with severe mental illness and HIV. To collect the data, RAND staff conducted computer-assisted interviews. Blood samples were used to determine CD4 cell counts, a measure of a specific type of immune cell that decreases as HIV progresses.
We measured barriers to care, experience with care, and health outcomes, all of which can be reliably and validly measured among patients with severe mental illness (
38,
39,
40 ). Barriers to care and experience with outpatient care were both measured by single items, which were, respectively, "During the last six months, did you ever need physical health care but could not get it?" and "Would you recommend your usual source of HIV care to other people with HIV?"
Patients' experience with a recent hospital stay for physical health care was measured with a ten-item hospital problem score derived from the Picker Survey (
41 ). These items were as follows: one main physician was in charge of care, it was easy to talk to staff about things that worried the patient, the patient received timely help, answers to questions were understandable, the patient was treated with respect and dignity, pain was controlled, physicians and nurses did not contradict each other, worries about the condition or treatment were addressed, tests were explained understandably, and the patient could contribute to treatment decisions. The hospital problem score was the percentage of items indicating a problem.
There were several additional measures. Functional health status and disability days were derived from the 36-item Short-Form Health Survey of the Medical Outcomes Study (
42 ). The health status scale included nine items (
α =.87 and .92, respectively, in samples of HIV patients with and without severe mental illness) regarding the extent to which, in the past four weeks, the patient's health limited vigorous activities, climbing one flight of stairs, walking more than one mile, walking one block, bathing or dressing, preparing meals or doing laundry, shopping, getting around at home, and feeding oneself. Scores were calculated as the average across items and were standardized on a scale from 0 to 100 points, with higher scores indicating better health. Disability days were measured as days in the past month in which at least half of the day was spent in bed because of health problems. We also collected data regarding age, sex, race and ethnicity, income, route of HIV exposure, recent drug use, case management, and CD4 cell count.
Statistical analyses
Separate weighting schemes were used to account for the different design characteristics of the HIV samples with and without severe mental illness (
43 ). Because the sample with severe mental illness represented the universe of patients with severe mental illness and HIV known by public health agencies and willing to be interviewed at the time of the study, a weight of 1 was assigned to each patient with severe mental illness. Observations of the sample without severe mental illness were weighted to reflect probability of selection across subpopulations, attrition over time, provider and participant nonresponse, and number of providers. All analyses were conducted with Stata software, version 7.0.
Because patients and systems of care differed across the two sites, we separately analyzed data for patients from the two metropolitan areas. We compared unadjusted measures for patients with and without severe mental illness by using Student's t test for continuous variables and Pearson's chi square test for categorical variables. For multivariate analyses of care and outcome measures, we used logistic regression for dichotomous measures and linear regression for continuous measures. All models adjusted for demographic and clinical factors, including age, sex, race and ethnicity, income, route of HIV exposure, recent drug use, and CD4 cell count. We did not adjust for whether patients had a case manager because case management and psychiatric status were highly correlated; 267 patients (91%) with severe mental illness and HIV had a case manager, whereas 569 patients (44%) without severe mental illness had one.
We also conducted several sensitivity analyses. First, to detect bias resulting from patients in the HIV-only HCSUS samples who might have had severe mental illness, we developed a three-item index based on use of psychiatric hospital services and medications to identify these persons. Thirty-nine patients (3% of HCSUS unweighted sample) were identified with this criterion. This low number was consistent with the HCSUS focus on nonpsychotic disorders, such as panic disorder, dysthymia, generalized anxiety disorders, and major depression (
29,
36 ). When we excluded these 39 patients from the analyses, results were unchanged.
Second, we reran the primary analyses without controlling for history of HIV exposure (such as use of injected drugs) or recent drug use, because adjusting for these measures could mask important differences in the experience of HIV patients with and without severe mental illness. Again, results were unchanged. Third, to determine whether the extended data collection period for patients with severe mental illness and HIV in New York City biased results, we ran separate analyses on that group in which the year of interview was included with other covariates. Although respondents interviewed in 2002 (9% of the sample) were less likely to report being unable to obtain care than those interviewed in 2000, year was not associated with other measures.
Results
Characteristics of respondents
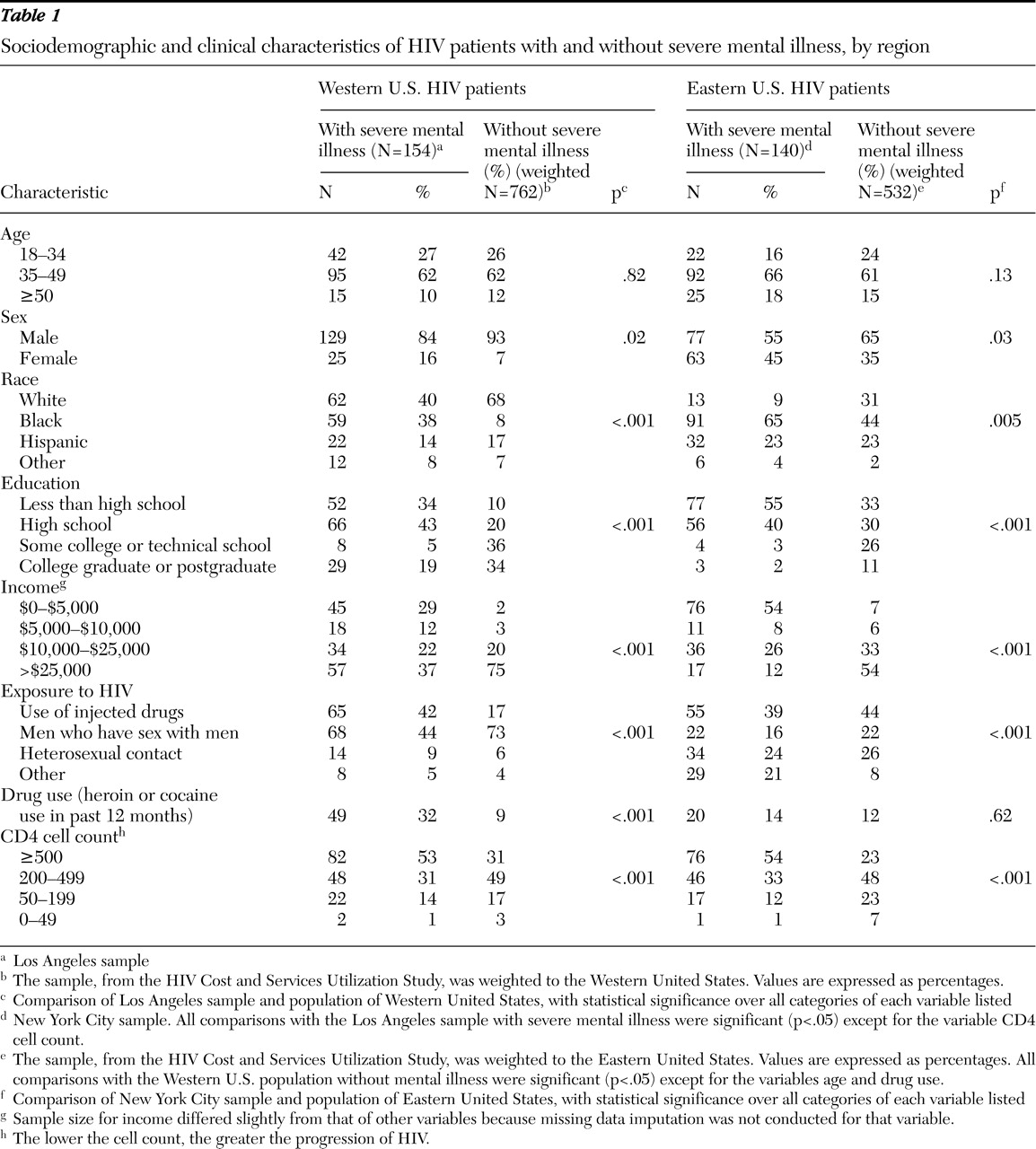
Patients' characteristics differed by metropolitan area and region (
Table 1 ). Among patients with severe mental illness and HIV, more in Los Angeles than in New York City were young, male, white, and college educated; had high income; were exposed to HIV through homosexual male contact; and recently used heroin or cocaine. Among HIV patients without severe mental illness, more in the West than in the East were young, male, white, and college educated; had high income; were exposed to HIV through homosexual male contact; and had CD4 cell counts of 500 or above.
Compared with HIV patients in the West who did not have severe mental illness, fewer Los Angeles HIV patients with severe mental illness were male, white, and educated beyond high school; had high income; or were exposed to HIV through homosexual male contact. Also, more of this group were exposed to HIV through use of injected drugs, had recently used heroin or cocaine, and had CD4 cell counts of 500 or above. Compared with HIV-only patients in the East, fewer New York City patients with severe mental illness and HIV were white and educated beyond high school; had high income; and were exposed to HIV through homosexual male contact. Also, more patients of this group had CD4 cell counts of 500 or above.
Barriers, patient experience, and health outcomes
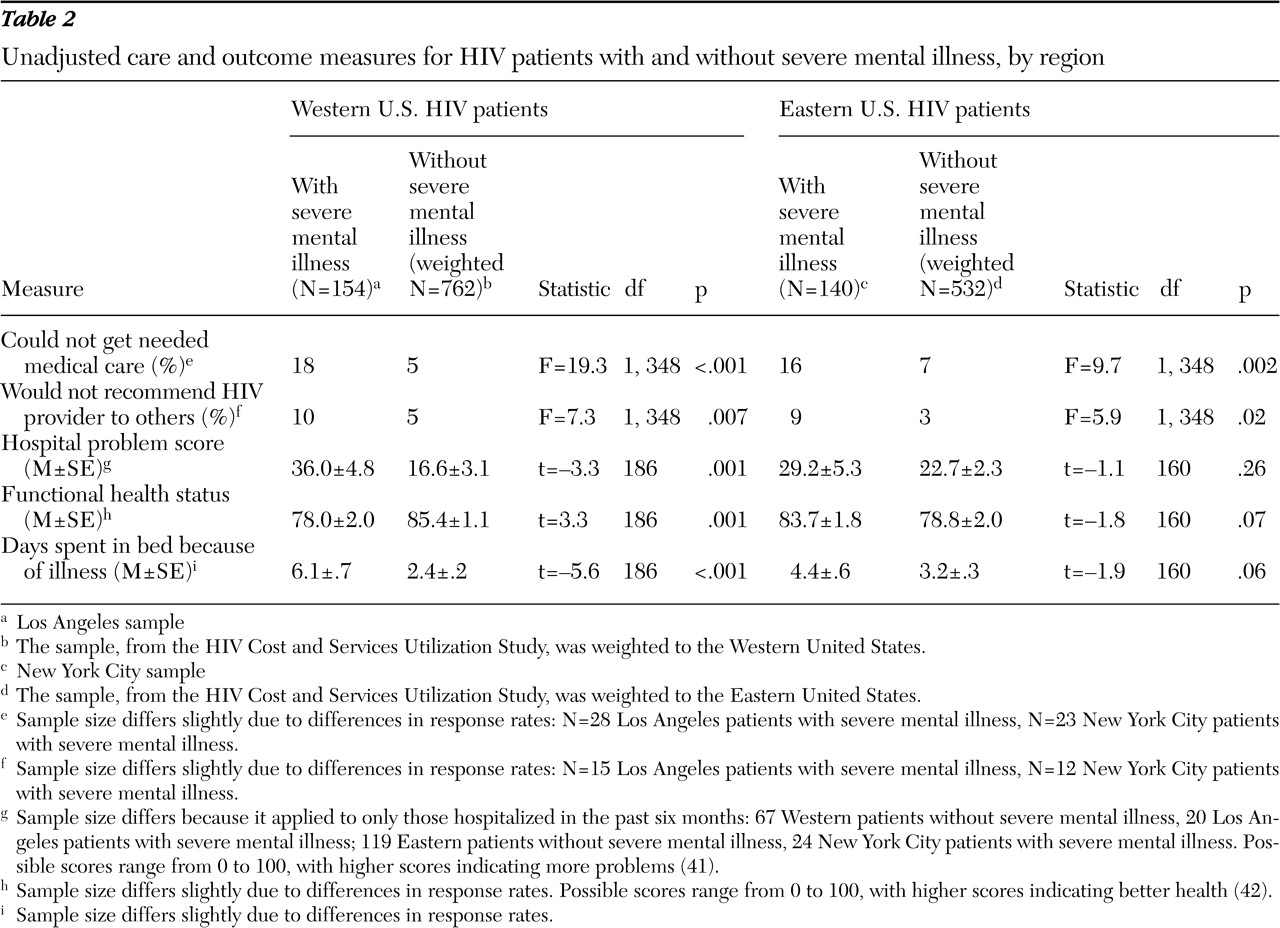
Los Angeles HIV patients with severe mental illness were more likely than patients without severe mental illness in the West to report being unable to obtain care (18% versus 5%; p<.001) (
Table 2 ). They also had higher hospital problem scores (36% versus 17%; p=.001); there were more frequent problems on six of ten items, including having more than one physician in charge of care, not receiving needed help, not receiving understandable answers, physicians and nurses contradicting one another, tests not explained in an understandable way, and lack of involvement in treatment decisions. Patients with severe mental illness were also less likely to recommend their outpatient HIV provider (10% versus 5%; p=.007) and had worse functional health status (78.0 versus 85.4; p=.001) and more disability days (6.1 versus 2.4; p<.001).
New York City HIV patients with severe mental illness were more likely than patients in the East without severe mental illness to report being unable to obtain care (16% versus 7%; p=.002) and less likely to recommend their HIV provider to others (9% versus 3%; p=.02) (
Table 2 ). However, patients with severe mental illness and HIV did not differ on other measures from the Eastern U.S. group without severe mental illness.
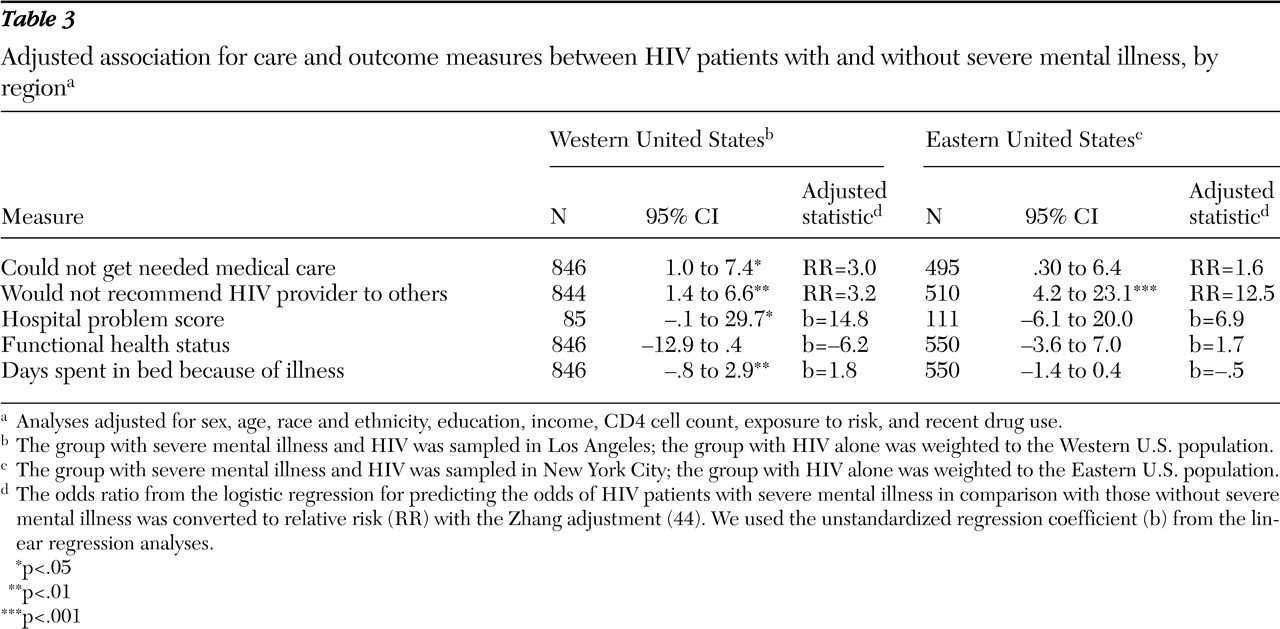
After we adjusted for demographic and socioeconomic factors, exposure history, drug use, and CD4 cell count (
44 ) (
Table 3 ), we found that Los Angeles patients with severe mental illness and HIV were more likely than patients in the West without severe mental illness to have difficulty obtaining care (relative risk [RR]=3.0, p<.05) and experience problems with hospitalization (b=14.8, p<.05), were less likely to recommend their outpatient provider (RR=3.2, p<.01), and reported more disability days (b=1.8, p<.01). However, the relationship between the presence of severe mental illness and functional health status was reduced to borderline significance (b=-6.2, p=.07). New York City patients with severe mental illness and HIV remained less likely to recommend their outpatient provider than HIV patients in the East without severe mental illness (RR=12.5, p<.001), but the relationship between the presence of severe mental illness and barriers to care was no longer significant.
In additional bivariate analyses to assess whether competing subsistence needs (
45,
46 ) differentially affected barriers to HIV care, we compared the patients with and without severe mental illness on the following item: "In the past six months, have you ever had to go without health care that you needed because you needed the money for food, clothing, housing, etc.?" Los Angeles patients with severe mental illness and HIV were more likely than comparable patients without severe mental illness to forgo care because of costs (20% versus 6%; F=18.83, df=1 and 348, p<.001). However, the same comparison between groups in New York City was not significant.
Access to case managers also differed between HIV patients with and without severe mental illness. Although all patients in the study had a regular source of care, only 44% of HIV patients without severe mental illness had a case manager compared with 91% of HIV patients with severe mental illness (F=147.4, df=1 and 348, p<.001). Patients with severe mental illness and HIV in New York City were more likely than those in Los Angeles to have a case manager (95% versus 88%, χ 2 =4.90, df=1, p=.03).
Discussion
In this study, we sought to determine the impact of severe mental illness on HIV care. We found that compared with HIV patients without severe mental illness, HIV patients with severe mental illness had more difficulty obtaining medical care, were less satisfied with their outpatient HIV care, had more problems during hospitalization, had worse functional health status, and had more disability days. These differences were present for all five measures in Los Angeles and for two measures in New York City and were only partially explained by potential confounders. Our findings are consistent with prior studies of patients with severe mental illness with conditions other than HIV (
3,
4,
6,
8,
26 ).
These results are likely a conservative estimate of barriers to and problems with HIV care for patients with severe mental illness and HIV. In our study, this group had access to case managers and related services through mental health agencies. Many people with severe mental illness, however, receive no mental health care (
47 ) or case management services, so their HIV care might be substantially worse. Case management can help address problems with subsistence needs, access to HIV care, attendance at appointments, and adherence to antiretroviral therapy (
48 ). With adequate case management, many patients with severe mental illness and HIV achieve adherence rates equal to or better than HIV patients without severe mental illness (
49 ).
The relatively modest differences between HIV patients with and without severe mental illness may also be a consequence of the relatively high rates of case management available to the former in our sample. The HIV patients without severe mental illness had a regular source of care, but the proportion assigned to case managers was less than half that of HIV patients with severe mental illness. Although we did not assess quality of case management or medication use, patients with severe mental illness and HIV in our sample had higher adjusted CD4 cell counts. In a separate report focused on clinical process of care in the Los Angeles sample, we found that patients with severe mental illness received rigorous antiretroviral therapy and monitoring of their CD4 cell counts and viral loads at rates that were at least equal to those of HIV patients without severe mental illness (
50 ).
Differences in care tended to be smaller and to occur on fewer measures in New York City than in Los Angeles. This pattern of results could occur if a greater proportion of both groups of patients in New York City received their HIV care from HIV specialists or specialized HIV clinics. Such providers may have more experience caring for HIV patients from vulnerable populations than a primary care provider who sees relatively few HIV cases. Even without detailed knowledge of the organization of care, however, it was clear from our findings that more resources are devoted to providing services for HIV patients and for seriously mentally ill patients in New York City than in Los Angeles. At the state level, New York has the highest expenditures per reported AIDS case, received the highest "mental health generosity" score, and ranks highest in mental health expenditures (
31,
51 ). California spends far less on its AIDS cases and ranks 31st among all states in mental health expenditures (
34,
51 ). New York State also implements more specialty assessment and treatment services for HIV patients with severe mental illness. Patients with severe mental illness and HIV in New York City were more likely than those in Los Angeles to have a case manager and had better scores on several indicators influenced by case management (
48 ). Given the relatively small differences in case management rates, however, it is unlikely that case management, per se, accounted for all differences between the two metropolitan areas.
Unmeasured differences in the way patients with and without severe mental illness respond to questions about their care may explain some of our results. For example, patients with worse physical or mental health tend to report more problems and be less satisfied overall with their health care (
40,
52 ). However, sicker patients or patients with more complex illnesses, including those with co-occurring psychiatric conditions, also evoke more negative reactions from health care providers, which can, in turn, decrease patients' satisfaction with their care (
40,
53,
54 ). Similarly, the complex care required by these patients creates more opportunities for miscommunication and unexpected developments than exist for patients whose problems are less complex (
55,
56 ). Finally, the differences between Los Angeles and New York City, particularly the lower rate of reported barriers or problems, do not support the notion of a consistent reporting bias among patients with severe mental illness.
Our study had several limitations. First, our samples of patients with severe mental illness were drawn from two large metropolitan areas with relatively well-developed mental health and HIV services. Our results may not be generalizable to those with severe mental illness in areas with fewer services (
33,
34,
57,
58 ). Second, hospitalization was infrequent for HIV patients with and without severe mental illness, in part because by 1998, when the data collection for this study began, use of highly active antiretroviral therapy was widespread. Thus, although differences in rates of problems during hospitalization were statistically significant, estimated rates of hospital problems are not precise. Third, because respondents' health status and disability days before becoming infected with HIV were unknown, we cannot rule out the possibility that disparities on these measures were due to psychiatric status rather than to differences in HIV care. Indeed, we would expect general health status and disability to be somewhat worse for HIV patients with severe mental illness than for those without. Similarly, we cannot rule out the possibility that unmeasured differences related to sample timing, particularly for the New York City sample, could have influenced results, but sensitivity analyses suggest that any significant relationships caused by timing were small and unlikely to change our findings.
A final caveat is that because the comparison group without severe mental illness was obtained from a separate study with a different sampling design and other possible differences, our results should be viewed as only suggesting but not confirming disparities in care. Additional research using directly comparable data is needed to verify apparent disparities and clarify underlying causes.
Conclusions
The results from this study suggest that the presence of severe mental illness may negatively affect HIV care, given that patients with severe mental illness and HIV in our sample experienced more barriers to and problems with HIV care than did HIV patients without severe mental illness from a separate national probability study. Nonetheless, potential problems facing these patients may have been partially offset by case management services available to them, particularly in New York City. Although broader and more effective interventions are needed, these results suggest continued investment in special services for patients who have severe mental illness and HIV will help ensure adequate access to critical HIV services.
Acknowledgments and disclosures
This research was supported by grants R01-MH-55936-05 and P50-MH-54623 from the National Institute of Mental Health and by the Department of Veterans Affairs, Desert Pacific Mental Illness Research, Education, and Clinical Center. Additional support was provided by the Robert Wood Johnson Foundation, Merck and Company, Glaxo-Wellcome, Inc., the National Institute on Aging, and the Office of the Assistant Secretary for Planning and Evaluation in the U.S. Department of Health and Human Services. These views represent the opinions of the authors and not necessarily the supporting agencies. The authors thank Shirley Nederend, M.A., Karen McKinnon, M.A., and Francine Cournos, M.D., for help in creating the structured interview; Judith F. Perlman, M.A., and the RAND survey research group for data collection; Angela Miu, M.S., for programming in the initial portions of the study, and Maurice Weise, M.D., Dennis Murata, M.S.W., and Jessie Tait, R.N., M.S., of the Los Angeles County Department of Mental Health for support. The authors also thank Ella Kemp, for managing the data collection in New York and Dr. Cournos, Ms. McKinnon, and Jim Satriano, Ph.D., for assistance with the New York mental health system. Finally, we thank Jolene Galegher, Ph.D., and Chloe Bird, Ph.D., for their helpful comments.
The authors report no competing interests.