The prevalence of diabetes mellitus has been steadily increasing in the U.S. population. Self-reported prevalence in successive national surveys has risen from 5.3% in 1988–1994 to 6.5% in 1999–2002 (
1 ). A survey of inpatient databases suggests that this trend is amplified among psychiatric patients, with a prevalence of 6.9% in 1997 and 14.5% in 2004 (
2 ). Several second-generation antipsychotics were introduced into the United States over the period overlapping these surveys—clozapine in 1989, risperidone in 1993, olanzapine in 1996, quetiapine in 1997, ziprasidone in 2001, and aripiprazole in 2002. There has been growing concern about treatment-emergent hyperglycemia and diabetes associated with these medications (
3 ).
In response to these concerns we decided to assess our practice population. After conducting a cross-sectional study to determine the prevalence of diabetes mellitus among antipsychotic-treated patients, we attempted to estimate the prevalence of undiagnosed diabetes and measure the degree of glycemic control among patients with a diagnosis of diabetes. We intend to use the results to identify best practices for improved detection and management of glucose dysregulation in our population.
Determining prevalence
We began with a cross-sectional study of outpatients maintained on antipsychotics at the Connecticut Mental Health Center (CMHC) in New Haven. Evaluations were conducted from March 2002 to January 2004.
The CMHC serves a population of about 200,000 persons eligible for public-sector care from the Greater New Haven area, with an average daily census of 2,500 active outpatients. Most patients are treated by teams of prescribing psychiatrists and nonphysician clinicians in once- or twice-monthly individual or group sessions.
The sample was drawn from patients recruited for a study that screened for tardive dyskinesia. To identify potential participants, we queried the CMHC information management system and performed chart reviews. We attempted to recruit all individuals currently receiving treatment with antipsychotic medications who had been receiving such treatment for at least three months. We excluded only those who could not be reliably examined for tardive dyskinesia because of primary neurological disease (N=4). We report on the resulting 494 participants whom we were able to contact and who represent 40% of the 1,250 CMHC patients being treated with antipsychotic medications at the time.
The main outcome variable for this analysis is self-reported diabetes prevalence measured at the screening interview. Research interviewers asked patients if they had been told by a physician or health professional that they had diabetes, and if so, whether they were being treated with diet alone, oral agents, or insulin. Participants who reported a diagnosis of diabetes were asked to return for a serum hemoglobin A1C (HbA1C) level. Appropriate glycemic control was defined as a single HbA1C less than 7.0% (
4 ). The remaining patients were asked to return for a morning fasting plasma glucose (FPG) level. Undiagnosed diabetes was defined as an FPG level of greater than or equal to 126 mg/dl (7.0 mmol/L), and impaired fasting glucose was defined as an FPG level between 100 mg/dl to less than 126 mg/dl (5.6 mmol/L to less than 7.0 mmol/L) (
5 ).
The sample for this analysis was described in a previous report (
6 ). It was balanced for gender: 268 patients (54%) were male, and the mean±SD age was 43.7±10.7 years. Almost half the sample (243 patients, or 49%) was Caucasian. A total of 189 patients (38%) were African American, and 46 (9%) were Hispanic. A total of 375 patients (76%) had a schizophrenia spectrum diagnosis, and most of the rest (103 patients, or 21%) were being treated for an affective disorder. First-generation antipsychotics were prescribed to 142 patients (29%), and 352 (71%) were taking one or more second-generation antipsychotic medications at screening: olanzapine, 166 patients (34%); risperidone, 91 patients (18%); clozapine, 50 patients (10%); and quetiapine, 23 patients (5%). No patients were taking ziprasidone or aripiprazole. The mean body mass index was 32.6±8.0 kg per m
2, and 307 patients (62%) were smokers.
Of the 494 participants, 86 (17%) reported a diagnosis of diabetes (95% confidence interval [CI]=14.2–21.1%). The diabetes of 24 of these patients (28%) was managed with insulin with or without oral agents, 46 (54%) took oral agents but not insulin, and 11 (13%) managed with diet alone. Five patients (6%) did not know the nature of their diabetic treatment. HbA1C levels were collected for 55 of the 86 patients who reported a diagnosis of diabetes, of whom 37 (67%; CI=53.3–79.3%) met American Diabetes Association (ADA) guidelines for appropriate glycemic control (HbA1C less than 7.0%).
Of the 408 patients without a history of diabetes, 108 returned for fasting blood tests. Three patients (3%; CI=.6%–7.9%) were found to have undiagnosed diabetes, and 28 patients (26%; CI=18.0%–35.3%) had impaired fasting glucose.
Discussion
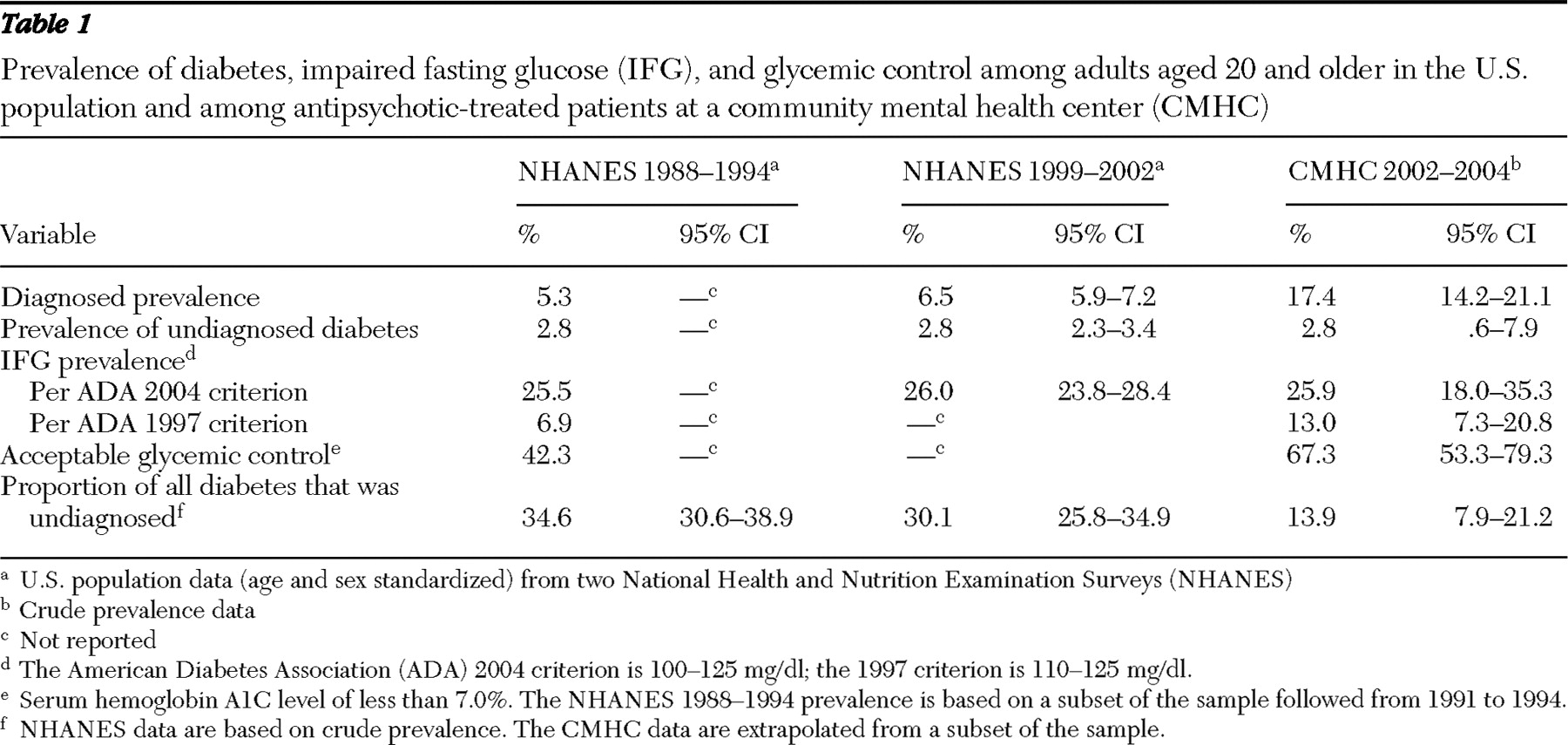
The National Health and Nutrition Examination Surveys (NHANES) are probability samples of the civilian, adult, noninstitutionalized U.S. population (
1 ). The surveys assess both diagnosed and undiagnosed diabetes. For comparison with our findings, NHANES data from the two relevant survey periods are presented in
Table 1 . Diabetes was more than two-and-a-half times as prevalent in our antipsychotic-treated population as in the general population. This is broadly consistent with estimates from populations with schizophrenia (
7,
8 ). Notably, the prevalence of impaired fasting glucose in our study was comparable to that in both NHANES samples only when the broader 2004 ADA definition was used (100–125 mg/dl), but when the 1997 ADA criterion was used (110–125 mg/dl) it was twice the first NHANES estimate (13.0% compared with 6.9%).
In combination with the higher prevalence of diagnosed diabetes in our sample, this suggests a "rightward shift" away from the general population in terms of a continuum of disease progression (
5 ) from normoglycemia through impaired fasting glucose to frank diabetes. Reassuringly, as shown in
Table 1, the ratio of undiagnosed to total diabetes at our center was 14%, which compares favorably with that in the first NHANES sample (34.6%) and the second NHANES sample (30.1%). However, only 108 (27%) of our undiagnosed patients returned for fasting glucose measurement. We must assume that they were more generally adherent to medical follow-up and do not adequately represent the rest of this group.
Glycemic control, which was assessed for 55 of 84 CMHC patients with a diabetes diagnosis (64%), was acceptable (HbA1C less than 7%) for a majority (37 patients, or 67%). This level of control compares favorably to that in the first NHANES sample (42.3%) and in other nonpsychiatric populations (
9 ). Possible explanations include heightened awareness among clinical staff and patients since the publication of the first NHANES study in 1998. A more specific possibility is the salutary effect of the chronic care model employed at CMHC. Our patients who are maintained on antipsychotic medications probably make contact with clinicians at a greater frequency than the general population. Also, since 2000, psychiatrists at CMHC have been required to document adequacy of general medical follow-up at six monthly treatment review meetings held with patients and their clinicians. Although our HbA1C results are probably skewed by data from patients in our sample who followed medical recommendations most reliably, the large percentage of patients evaluated and the high rate of acceptable control support the conclusion that once diabetes is diagnosed, treatment can be as effective among seriously ill and economically disadvantaged psychiatric patients as in the general population.
Conclusions
The findings were discussed at a weekly best-practices meeting of psychiatrists at CMHC. Several practice improvement goals were formulated and are summarized below.
Diabetes mellitus is common among patients prescribed antipsychotics at our center: as many as one in six may have this disease. A preliminary estimate of undiagnosed disease is reassuringly small, but as many as a quarter of the undiagnosed sample had impaired fasting glucose, which raises concern for a substantial population who may be at risk of diabetes and cardiovascular complications (
10 ).
Glucose dysregulation is best conceptualized within overall metabolic status. The poor cardiovascular risk profile of persons with serious mental illness was confirmed in the largest available national cohort of schizophrenia patients, with high rates of nontreatment for diabetes (30.2%), hypertension (62.4%), and dyslipidemia (88.0%) (
11 ). We estimate that 61% of our sample was obese (body mass index of 30 or greater) with a mean body mass index greater than 32 and a high frequency of tobacco use (62%). Close attention must be paid to all cardiovascular risk factors for purposes of screening, referral, and psychotropic medication choice.
Screening and monitoring of care for glucose dysregulation are two conceptually and practically distinct tasks that need to be addressed in our population. For screening of asymptomatic individuals, adherence to the ADA consensus guidelines for second-generation antipsychotics (
3 ) was proposed as a practice improvement goal. Such an effort has already been informally under way for the past year in the Psychosis Program at our center, where most patients requiring antipsychotics are treated. Factors that are periodically assessed include personal and family history, body mass index, blood pressure, FPG, and fasting lipid profile. Patients in the program, like those in the study, have had difficulty complying with morning fasting glucose measurements. Although HbA1C alone has inadequate sensitivity (
12 ) for screening, further exploration of its use in conjunction with random blood glucose measurement was deferred to a working group (see below). In regard to monitoring, most of our diagnosed sample demonstrated adequate glycemic control. Although this finding is somewhat reassuring, there is evidence that careful control of other risk factors, such as blood pressure and cholesterol, are at least as critical in preventing the macrovascular complications of diabetes (
13 ). This underscores the need for comprehensive monitoring of cardiovascular risk. A local Veterans Affairs hospital–based integration of medical and psychiatric care has significantly improved such monitoring (
14 ). Learning from this experience to improve communication between CMHC and primary care clinicians was identified as an important priority.
A working group of CMHC psychiatrists and an internal medicine consultant has been formed to advance efforts in the Psychosis Program, review guidelines (
15 ), and develop centerwide recommendations for diabetes screening and monitoring in the context of overall cardiovascular risk.