In 1975 the American Psychiatric Association released a study of psychiatrists' religious characteristics, which found that psychiatrists were more likely than the rest of the population to be nonreligious or Jewish and less likely to be Protestant or Catholic (
1 ). In 1968 Marx and Spray (
2 ) had found a similar pattern among a sample of mental health professionals working in Chicago, Los Angeles, and New York. And in a 1985 survey, Bergin and Jensen (
3 ) found that psychiatrists less frequently attended religious services, tended not to base their lives on any religion, and less often tried to live their lives according to their religious beliefs. The consistency of these results is curious, because psychiatry in the United States is by no means a monolithic body of thought and there are many instances of cooperation between psychiatry and religion (consider Oskar Pfister [
4 ], the Emmanuel Movement [
5 ], and the Gallahue Conference on Religion and Psychiatry [
6 ]).
Although empirical studies suggest that psychiatrists in earlier decades were relatively nonreligious, several factors raise questions about whether the same is true of psychiatrists practicing today. Many of the professionals then surveyed have long since retired, and several signs suggest that psychiatry has been moving toward a greater appreciation of religion and spirituality. A substantial body of empirical research has pointed to a salutary influence of religion on patients' psychological health (
7,
8,
9 ). The fourth edition of the
Diagnostic and Statistical Manual of Mental Disorders modified the language of previous editions to acknowledge that religiosity may go awry but is not intrinsically maladaptive (
10 ). And the new legitimacy of religion and spirituality within the profession is perhaps most clearly indicated by the 1995–1996 edition of the
Graduate Medical Education Directory, which required psychiatric residencies to include didactic sessions on issues of religion and spirituality (
11 ).
With our survey we sought to overcome some of the limitations of prior studies and assess the religiosity and spirituality of today's psychiatrists. Whereas earlier studies included few measures of religiosity, this study examined several well-validated measures of psychiatrists' religious and spiritual characteristics. Prior studies compared the religious characteristics of psychiatrists with public data regarding the general population, but this study compared psychiatrists and other U.S. physicians to determine whether the religious profile of psychiatrists is unique to the field of psychiatry or merely reflects that of physicians in general. Finally, this study went a step beyond comparing psychiatrists' and nonpsychiatrists' religious characteristics. It explored whether religious nonpsychiatrist physicians are less willing than other physicians to refer to psychiatrists a hypothetical patient with ambiguous psychiatric symptoms.
Methods
This study's methods have been described in detail elsewhere (
12,
13 ). In 2003 we mailed a confidential, self-administered, 12-page questionnaire to a stratified random sample of 2,000 practicing U.S. physicians age 65 or younger, chosen from the American Medical Association Physician Masterfile, a database intended to include all physicians in the United States. We oversampled psychiatrists to increase the power of analyses presented here. Physicians received up to three separate mailings of the questionnaire, and the third mailing offered $20 for participation. This study was approved by the University of Chicago Institutional Review Board.
Survey content
Primary criterion variables were measures of physicians' religious characteristics. We included constructs and measures that are well validated in other social science and psychological research (
14 ). Physicians' religious affiliations were categorized as none (includes atheist, agnostic, and none), Protestant, Catholic, Jewish, Hindu, Muslim, or other (includes Buddhist, Mormon, Eastern Orthodox, and other). Organizational (
14 ), or participatory (
15 ), religiosity was measured as physicians' frequency of attendance at religious services, which was categorized as never, once a month or less, or twice a month or more. Physicians were asked whether they believe in God and the afterlife (possible responses were yes, no, and undecided) and to indicate the extent to which they look to God for strength, support, and guidance to cope with major problems in their life versus trying to make sense of the situation and deciding what to do without relying on God (responses could range from "a great deal" to "not at all").
Intrinsic religiosity—the extent to which an individual embraces his or her religion as the "master motive" that guides and gives meaning to his or her life (
16 )—was measured as agreement or disagreement with two statements: "I try hard to carry my religious beliefs over into all my other dealings in life" and "My whole approach to life is based on my religion." Both statements are derived from Hoge's Intrinsic Religious Motivation Scale (
17 ) and have been validated extensively in prior research (
17,
18,
19 ). Intrinsic religiosity was categorized as low if physicians disagreed with both statements, moderate if they agreed with one but not the other, and high if they agreed with both.
In recent years, there has been a trend toward the preference of the study of spirituality rather than religion (
20,
21,
22 ). There is still disagreement as to what spirituality means (
22,
23 ), but it has been proposed as "broader" than religion such that many persons who are not religious may still be spiritual (
20 ). In this study we allowed physicians to define themselves by asking, "To what extent do you consider yourself a spiritual person?" We grouped that question with the parallel question, "To what extent do you consider yourself a religious person?" Responses were dichotomized into those who answered "very" or "moderately" and those who answered "slightly" or "not at all."
Secondary criterion variables included measures of agreement with the following statements: "My religious beliefs influence my practice of medicine," "For me, the practice of medicine is a calling," "My experiences as a physician have caused me to question my religious beliefs," and "I find it challenging to remain faithful to my religion in my work as a physician."
Finally, to explore the ways the religious characteristics of other physicians mediate their willingness to refer patients to psychiatrists, we included the following brief vignette: "A patient presents to you with continued deep grieving two months after the death of his wife. If you were to refer the patient, to which of the following would you prefer to refer first? (a psychiatrist or psychologist, a clergy member or religious counselor, a health care chaplain, or other)." The vignette was designed to present ambiguous symptoms of psychological distress in order to elicit fundamental tendencies and biases and avoid the impression that respondents were being tested on whether they recognize DSM-IV criteria for a particular disorder. Physicians' age, gender, race and ethnicity, non-U.S. versus U.S. medical school graduation, and region of residence were included as control variables.
Statistical analysis
Case weights (
24 ) were assigned and included in analyses to account for the sampling strategy and modest differences in response rate by gender and non-U.S. medical graduation. We first generated population estimates for psychiatrists' and other physicians' responses to the criterion measures. We then used the Pearson chi square test to examine the differences between psychiatrists and nonpsychiatrists on each religious characteristic. Finally, we used multivariate logistic regression to examine the relationship between physicians' religious characteristics and their referral preferences, after we controlled for physicians' other demographic characteristics. All reported p values are two-sided and not adjusted for multiple statistical testing. All analyses take into account survey design and case weights by using the survey commands of Stata SE, version 9.0.
Results
Survey response
Of the 2,000 potential respondents, an estimated 9% were ineligible because their addresses were incorrect or they were deceased. Details of ineligibility estimation are reported elsewhere (
12 ). Among eligible physicians, our response rate was 63% (1,144 of 1,820) and did not differ for psychiatrists and other physicians. Overall, non-U.S. medical graduates were less likely to respond than U.S. medical graduates (54% versus 65%, p<.01) and men were slightly less likely to respond than women (61% versus 67%, p=.03). These differences were accounted for by assigning case weights. Response rates did not differ by age, region, or board certification. Characteristics of survey respondents are included in
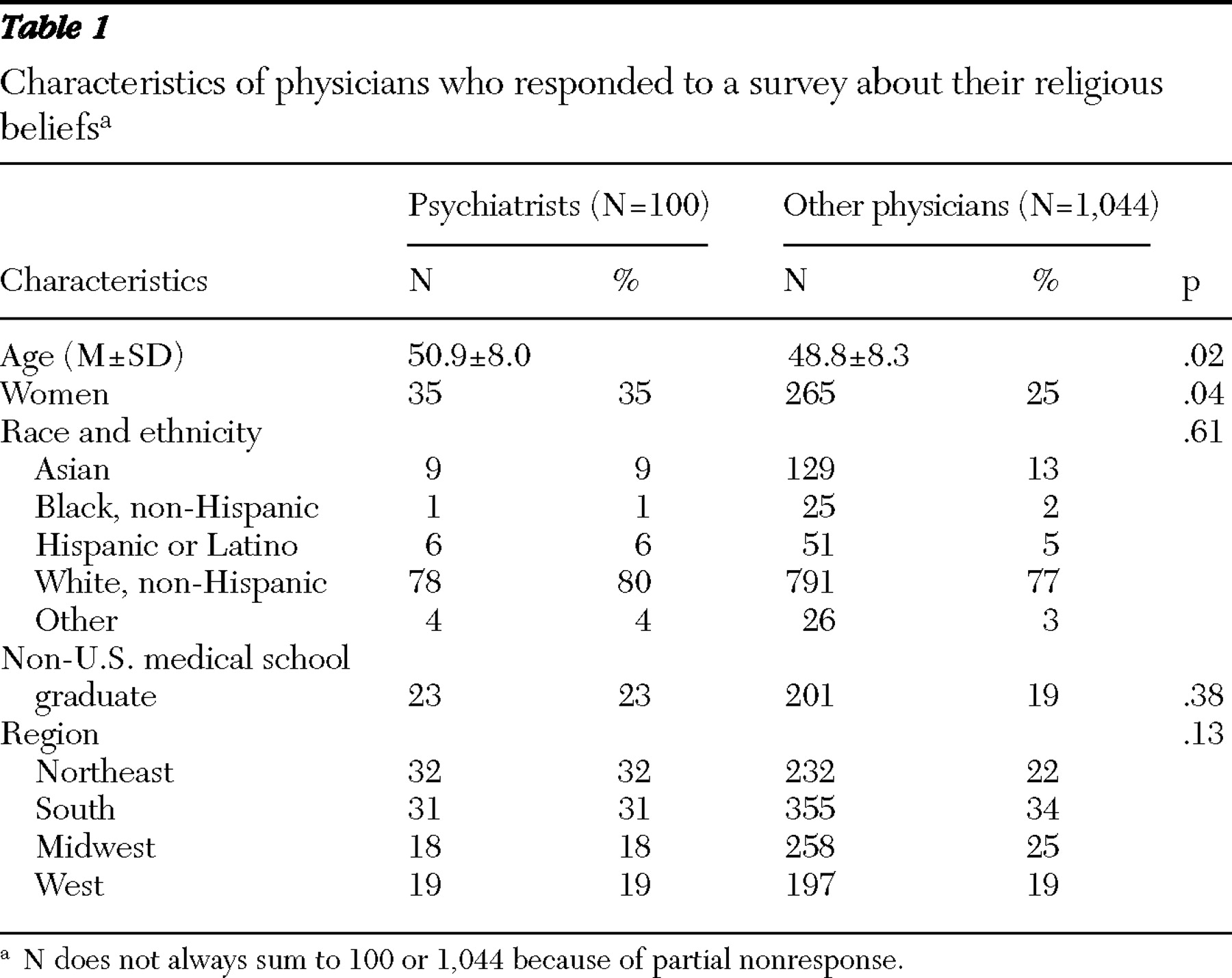
Table 1 . As shown in the table, psychiatrist respondents were slightly older than and more likely than nonpsychiatrists to be women. Psychiatrists did not differ from other physicians with respect to race and ethnicity, graduation from a non-U.S. medical school, or region.
Religious characteristics of psychiatrists
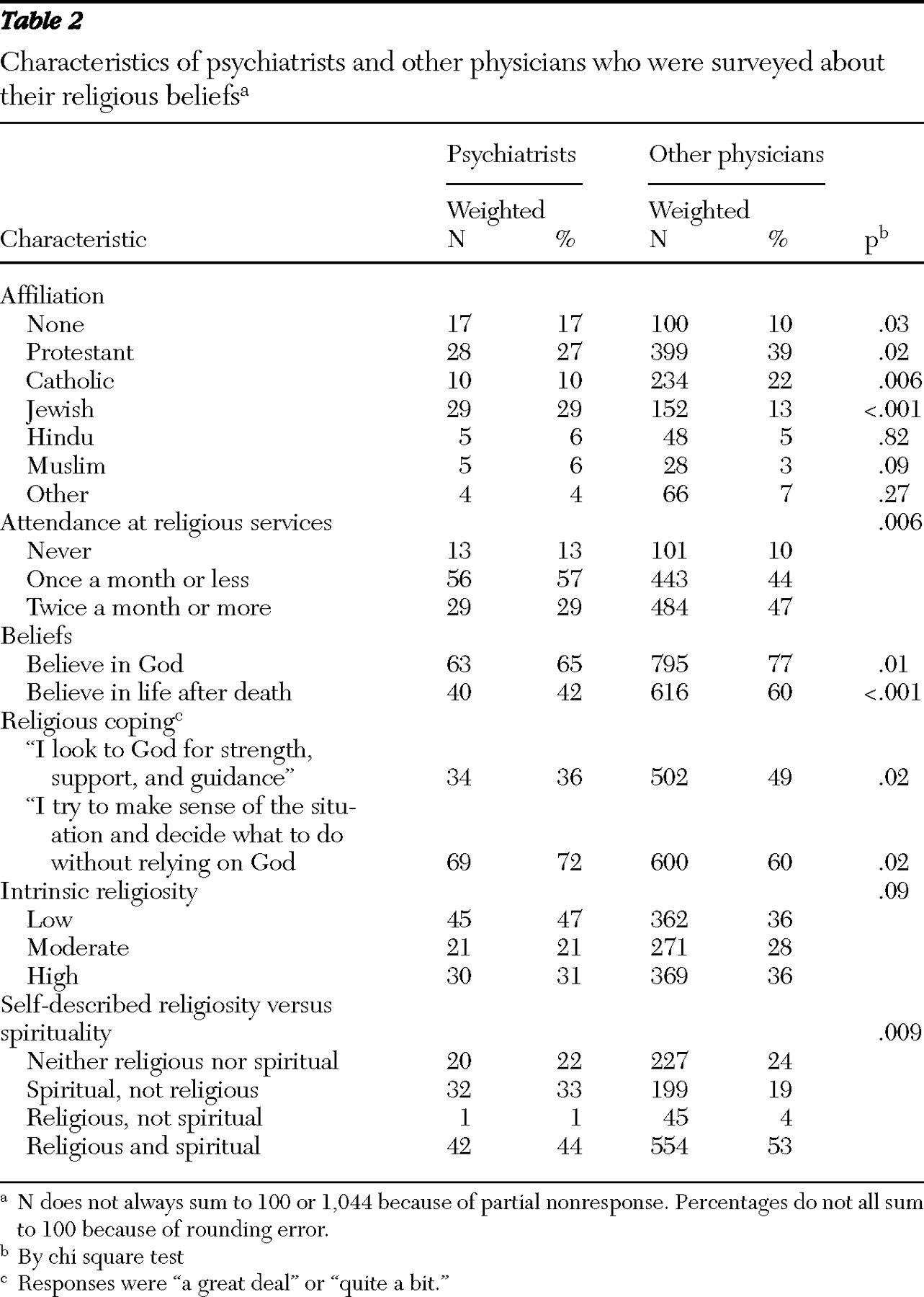
As shown in
Table 2, in comparison with other physicians, psychiatrists were significantly less likely to be Protestant or Catholic and more likely to be Jewish or have no religious affiliation. Psychiatrists were less likely to attend religious services frequently, believe in God or the afterlife, or cope by looking to God. In addition, psychiatrists were less likely to classify themselves as religious and more likely to classify themselves as spiritual but not religious (33% versus 19%).
Compared with other physicians, psychiatrists were equally likely to report that their religious beliefs influence their practice of medicine (50 psychiatrists, or 51%, versus 583 physicians, or 56%), the practice of medicine is a calling (72 psychiatrists, or 75%, versus 717 physicians, or 70%), their experiences as physicians have caused them to question their religious beliefs (16 psychiatrists, or 16%, versus 154 physicians, or 15%), and they find it challenging to remain faithful to their religion in their work as a physician (17 psychiatrists, or 18%, versus 209 physicians, or 21%). In post hoc analyses, we observed that whether psychiatrists find it challenging to remain faithful to their religion is related to their religious affiliation (nonreligious, 0%; Jewish, N=2, 8%; Protestant, N=9, 33%; Catholic, N=4, 43%; other, N=2, 15%; p=.01).
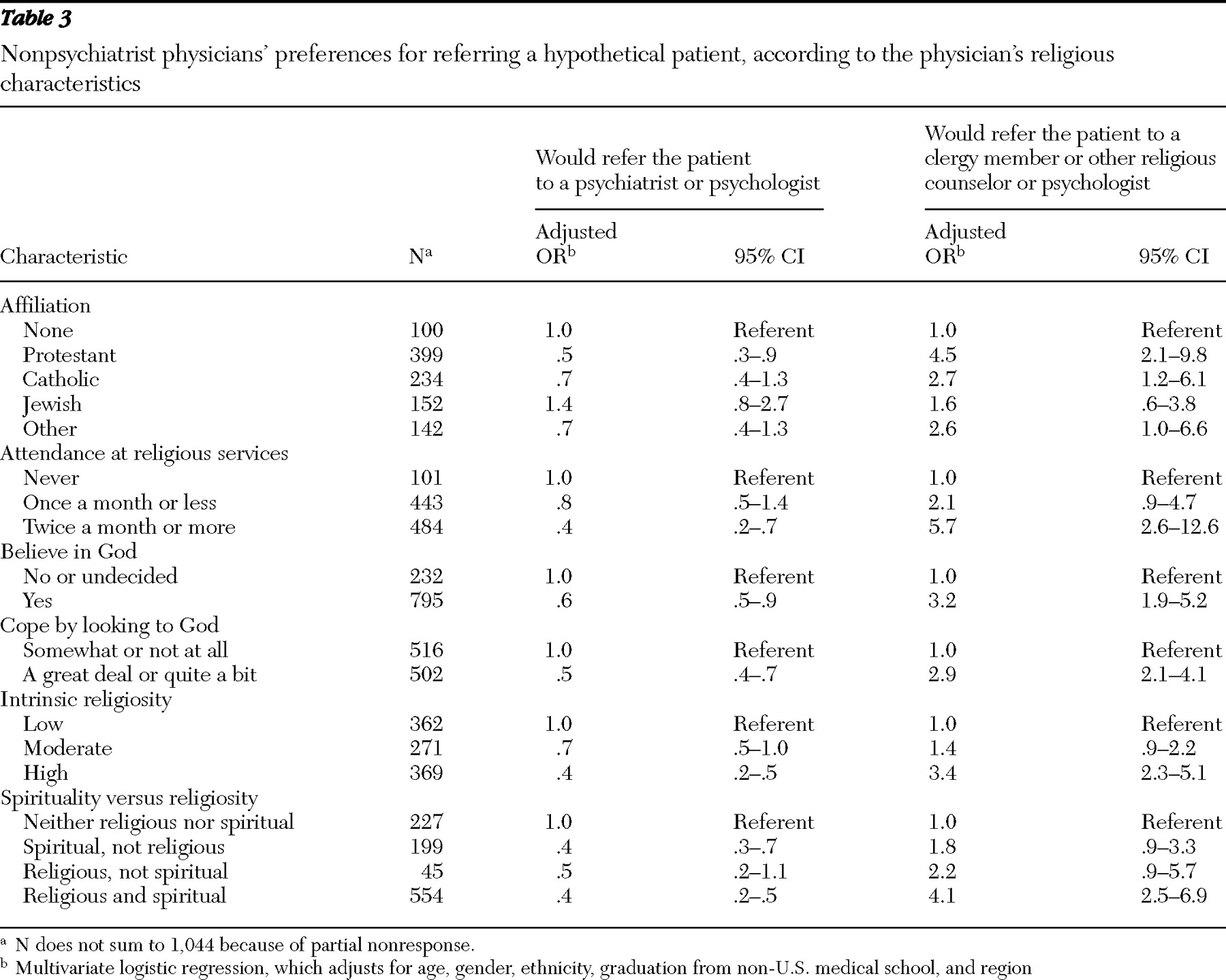
Religion and physicians' referral preferences
Table 3 presents the associations between nonpsychiatrist physicians' religious characteristics and their referral preferences for a hypothetical patient who presents with continued deep grieving two months after the death of his wife. Overall, 56% of physicians indicated that they would refer such a patient to a psychiatrist or psychologist, 25% to a clergy member or other religious counselor, 7% to a health care chaplain, and 12% to someone else (other). After adjustment for physicians' demographic characteristics, Protestants were half as likely as those with no religious affiliation to refer the patient to a psychiatrist or psychologist (odds ratio=.50). Furthermore, with respect to every other religious characteristic, those who were more religious were more likely to want to refer the patient to a clergy member or other religious counselor and less likely to want to refer to a psychiatrist (
Table 3 ).
Discussion
This study showed that, in comparison with other physicians, psychiatrists are less religious in general, are less likely to be Protestant or Catholic, and are more likely to be Jewish or nonreligious. These results are similar to findings from two and three decades ago (
1,
2,
3 ) but are in contrast with a 1993 study in which psychiatry residents were found to be more religious than the profession as a whole (
25 ). Thus the question arises about how long the field of psychiatry will display a religious profile that is not shared by other medical specialties. However, the persistence of this religious profile over multiple decades suggests that movements toward integrating religion, spirituality, and psychiatry are rooted in psychiatrists' recognition that religion is important to patients, rather than changes in psychiatrists' religious characteristics.
The finding that religious physicians are less likely to want to refer patients to a psychiatrist or a psychologist parallels earlier studies. Larson and colleagues (
26 ) reported that clergy members refer patients more often to religious psychiatric clinics, whereas psychologists and psychiatrists more often refer patients to psychoanalytic and hospital outpatient settings. Similarly, Koenig and colleagues (
27 ) found that psychiatrists refer patients to chaplains less frequently than to other professionals. In response to mild or moderate symptoms of mental distress, religious and nonreligious physicians appear to look for help in different places, with the result that the religious characteristics of physicians determine to some extent whether their patients receive evaluations from psychiatrists.
Psychiatry's unique religious profile has implications for efforts to provide culturally competent care for patients. For several years psychiatry has recognized that the cultures of both the patient and the physician affect how mental health concerns are described and evaluated, and cultural differences may hinder communication, the ability to make correct diagnoses, and the development of trusting relationships (
28 ). However, providing culturally competent care and tailoring therapies to the religious patient's worldview may be especially challenging for psychiatrists. First, differing religious characteristics may introduce a cultural obstacle from the start. Second, cultural factors may have unique significance in psychiatry, because psychiatrists more frequently encounter patients struggling with emotional, personality, and relationship problems. Patient care might therefore improve to the extent that psychiatric training emphasizes providing culturally competent care for patients with differing religious characteristics.
Another implication of these data is that religious patients who prefer to see like-minded psychiatrists (
29 ) may have difficulty finding a match because their religious group is underrepresented among psychiatrists. There is some indication that nonreligious therapists can effectively integrate religious components into treatments (
30 ), but psychiatrists who are not religious themselves might not accurately predict when therapies will conflict with religious worldviews (
30 ). In addition, some patients may find it difficult to trust their psychiatrists for fear they will suggest changing deeply held religious beliefs (
26 ), and others may avoid treatment altogether if they view seeking psychiatric treatment as a failure to trust God (
31 ). These data underscore the need to train psychiatrists to work with patients who may have religious views that are quite different from their own and raise questions about what contributes to physicians' choosing psychiatry as a specialty.
Because our data set is a cross-sectional survey, we can only speculate about why religious physicians may opt for nonpsychiatric careers and may be disinclined to refer patients to psychiatrists. Psychiatric residency program directors report they are not deterred by a candidate's religiosity and consider religion to be irrelevant to the recruitment process (
32 ). Yet something about psychiatry may dissuade religious medical students from applying to psychiatric residencies. Perhaps psychiatry's historical ties to psychoanalysis (
33 ), especially the antireligion statements of Freud and the liberal political views of many influential psychoanalysts of the 1950s–1960s (
34 ), continue to influence religious physicians' views toward the field. Alternatively, while psychiatry's prior focus on psychoanalysis has given way to a renewed interest in somatic etiologies of mental illness and pharmaceutical therapies (
33 ), religious physicians might still shy away from psychiatry if they believe psychiatry now overemphasizes biological processes. The training of psychiatrists or the cultural environment within psychiatry might also be factors if they affect psychiatrists' religious worldviews by providing competing explanations and understandings.
This study has several limitations with respect to the hypothetical clinical vignette. Physicians' referral preferences were measured only in reference to a single clinical scenario with an ambiguous presentation of grief and depression, and we would expect that preferences would vary less in reference to clinical situations with more severe and unambiguous psychiatric illness. The vignette did not specify the religious characteristics of the hypothetical patient, and it is possible that religious physicians and religious patients self-aggregate to such an extent that differences in referral preferences reflect differences in the religious characteristics of physicians' patient populations. In addition there is some ambiguity about whether the results reflect a relative unwillingness among religious doctors to refer patients to psychiatrists and psychologists or reflect a relative affinity for referring patients to religious professionals. Furthermore by lumping psychiatrists and psychologists into one response category for referral, we may have introduced a certain amount of survey error. Although the response rate was better than average (
35 ) and we did not find substantial evidence to suggest response bias (
12,
13 ), religious and other characteristics may have systematically affected in unmeasured ways physicians' willingness to respond. Finally, we do not know how physicians' self-reported preferences translate into their actual practices. Future studies should use experimental vignettes that cover a broader spectrum of clinical presentations that are relevant to clinical psychiatry.
Acknowledgments and disclosures
This work was funded by grant support (Integration of Religion and Spirituality in Patient Care Among U.S. Physicians) from the Greenwall Foundation and by grant K23-AT002749 from the National Center for Complementary and Alternative Medicine and by the Robert Wood Johnson Clinical Scholars Program (Dr. Curlin, Dr. Chin, and Dr. Lantos). The funding agencies did not have any role in the design, conduct, analysis, and interpretation of the study, nor in the preparation of the manuscript. The authors are indebted to the University of Chicago Templeton Network for their feedback on a draft of this article.
The authors report no competing interests.