With a county population of 3.5 million in 2003, Houston (Harris County) has extensive medical services, with more than 60 hospitals, scores of specialty health clinics, and high numbers of physicians per capita, well above the state and national average. Notwithstanding this seemingly bountiful supply, the large number of persons without insurance, estimated in 2003 at 32% of persons younger than 65 (
1 ), creates access problems for a significant portion of the population, particularly regarding behavioral health services.
The primary safety net provider in the county is the Harris County Hospital District (HCHD). The fourth largest publicly funded health care provider in the United States, HCHD operates three hospitals, 11 community health centers, eight school-based centers, a dental center, a program of health care for the homeless, and a center for patients with HIV-AIDS. Until 2004 all HCHD behavioral health services were provided at one hospital-based psychiatric outpatient clinic with an average waiting period of six months for new appointments.
In July 2004 HCHD launched a pilot project to place behavioral health staff into community health centers in order to better meet the behavioral health and primary care needs of a growing population of uninsured people in the county. The integrated care model being followed has been shown to be effective in managing behavioral health problems (
2,
3,
4,
5,
6 ). Successful programs have a high level of direct involvement of behavioral health specialists, well-defined treatment protocols targeted at specific populations, and structured follow-up and monitoring of patient treatment adherence and outcomes (
7,
8 ).
On the basis of the success of the pilot, in July 2005 the program was expanded and the Harris County Community Behavioral Health Program (CBHP) was formally created to provide behavioral and medical care services at all centers. By colocating behavioral and medical providers and by furthering the scope of behavioral interventions of primary care physicians at the centers, CBHP intends to provide behavioral services to more patients, shorten waiting periods for behavioral health appointments, and reduce transfers to hospital-based behavioral health services. In recognition of the effectiveness of this project, it received a 2007 American Psychiatric Association Achievement Award in the category of community-based programs (
9 ). Consistent with the best practices theme of providing pertinent and timely information about the effectiveness of new programs, this column describes the features and preliminary impact of the integrated care model implemented on a large scale in Houston.
The CBHP model
CBHP integrated behavioral health staff into the daily patient care process at 11 community centers. Psychiatrists were hired to provide psychiatric services one to two days per week, and master's-level behavioral health specialists were hired to provide psychotherapy throughout the week at each community center. A director was hired, and some hospital-based psychiatrists were reassigned to provide services in the community centers. CBHP delivers behavioral health and substance abuse screening, counseling, and treatment at each community center in close collaboration with the existing primary care staff.
CBHP's services include evaluation and treatment of scheduled patients, walk-in services for patients in crisis, and curbside consultations to primary care physicians in order to support behavioral health interventions implemented by primary care physicians themselves. Any center provider can refer patients to the behavioral health specialists or psychiatrists for screening, assessment, and treatment.
By co-locating behavioral and medical providers and by furthering the scope of behavioral interventions by primary care physicians, CBHP intended to provide behavioral services to more patients, shorten long waiting periods for behavioral appointments, and cut down on transfers to expensive hospital-based behavioral services.
Evaluation of the program
A preliminary evaluation of the program was required by the funding sources to document whether the initial objectives of the program were achieved.
Daily patient service logs were used to document the total number and characteristics of patients seen and the types of behavioral services provided. On the basis of these data a total of 2,894 patients were seen during the first 11 months of the program (July 2005 through May 2006). The total cost of the program was $774,791, or $267.63 per patient treated.
Psychiatrists saw 801 patients, behavioral health specialists saw 1,824 patients, and both saw 269 patients, for a total of 6,532 sessions. Frequent reasons for referrals to the program included depression, anxiety, bipolar disorder, and substance abuse problems. A majority of patients were female (2,075 patients, or 71.7%), and most were aged 19 to 64 years (2,376 patients, or 82.1%). Hispanics accounted for 42.3% (N=1,224); African Americans, 28.8% (N=833); and whites, 26.0% (N=752). About two-thirds (1,939 persons, or 67.0%) were totally uninsured, and another 20.1% (N=582) were beneficiaries of Texas' Medicaid or State Children's Health Insurance Program.
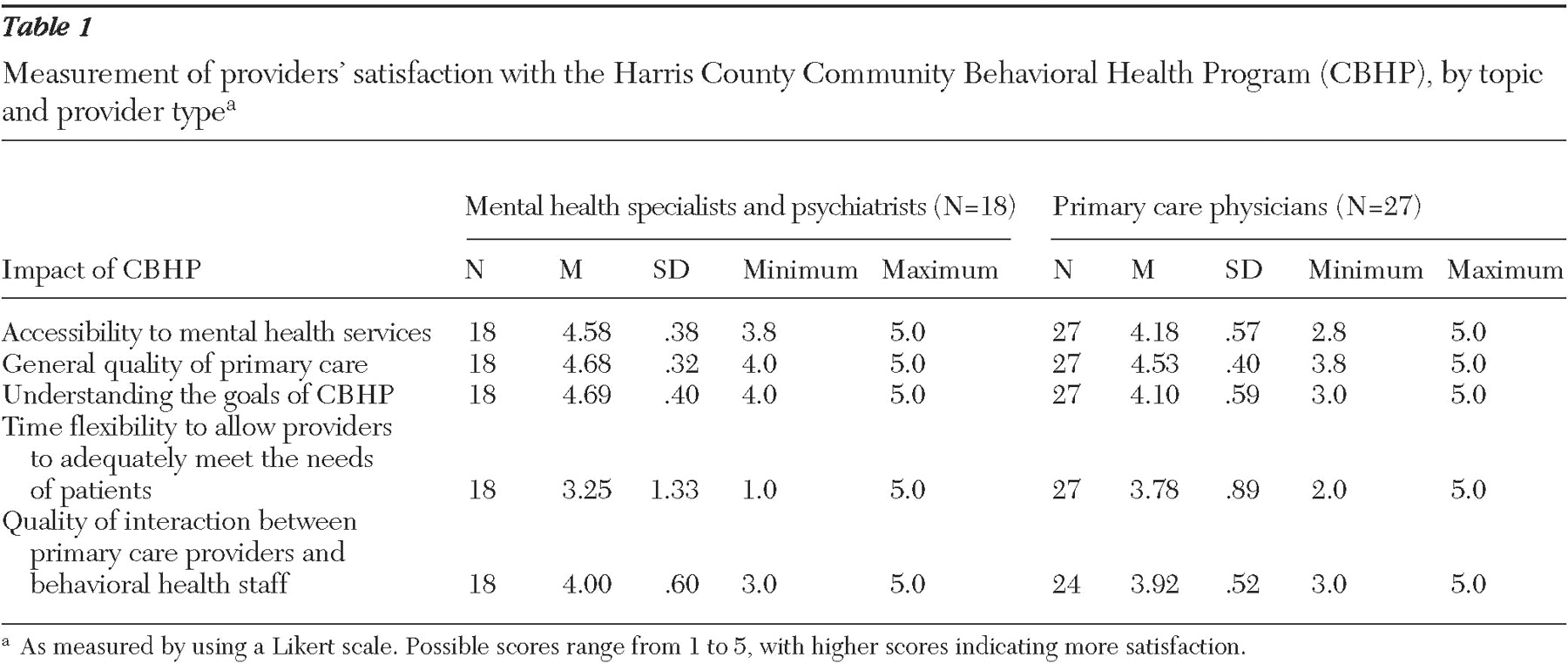
A questionnaire was developed to assess provider satisfaction with the program. One hundred questionnaires were distributed, and 45 were returned by 11 of the 11 behavioral health specialists, seven of the 11 psychiatrists, and 27 of the 124 primary care physicians. As shown in
Table 1, both the behavioral health staff and primary care physicians believed that CBHP achieved its objective of increasing accessibility to community-based behavioral health services. Providers also perceived that CBHP has improved significantly the general quality of primary care at community health centers.
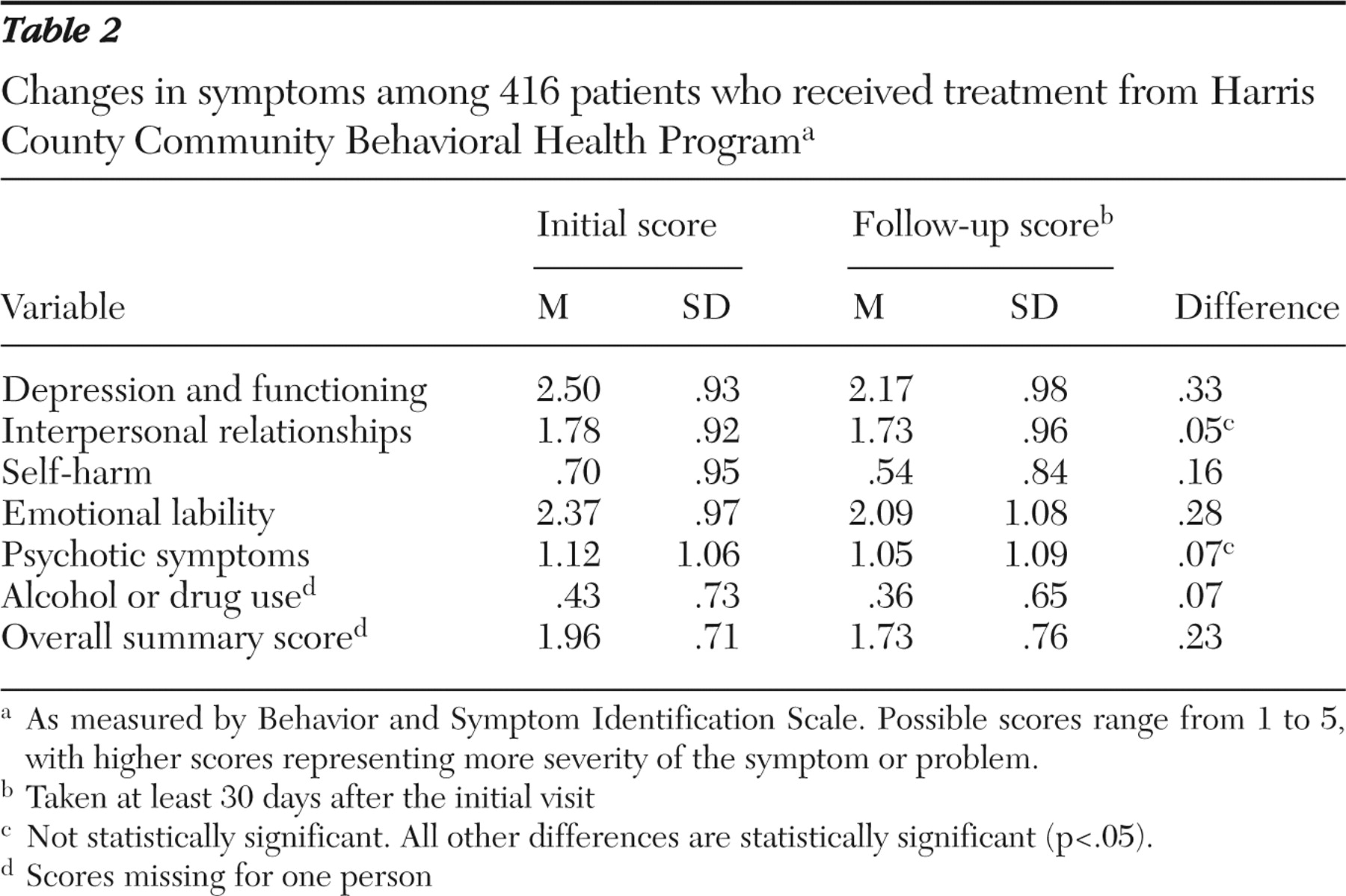
To examine the quality of services being provided, we monitored changes over time in the symptoms of treated patients by using the Behavior and Symptom Identification Scale (BASIS-24). The BASIS-24 measures a broad range of mental health functioning (
10 ). CBHP staff administered the BASIS-24 to patients on the first visit and follow-up visits.
From July 2005 through May 2006, BASIS-24 data for the initial visit and at least one follow-up visit were available for 416 patients. This number represents 72% of the 579 patients who were eligible to receive the follow-up BASIS-24 because they were seen by a CBHP provider more than once during the study period, with a follow-up visit occurring at least 30 days after the initial visit. Statistically significant improvement was detected in terms of the overall score and four out of six domain scores, including depression and functioning, self-harm, emotional lability, and alcohol or drug use (
Table 2 ). The effect size between baseline and follow-up was .23 in the overall score, and subscale effect sizes ranged from .07 to .33. Because the interventions are generally short-term, changes in the BASIS-24 scores indicate how patients feel before and after receiving treatment.
To determine whether the program increased access, we examined data on the frequency of behavioral services received by patients with existing psychiatric diagnoses referred to CBHP. The data were obtained from HCHD's medical records database from July 2004 through May 2006. A mirror analysis was performed comparing the use of behavioral services in the 12 months before and the 12 months after receipt of CBHP services. A comparison of the utilization of 260 patients who were treated in the HCHD system for a diagnosed behavioral problem before the implementation of CBHP and who received services from CBHP during the study period showed an increase of .8 in the number of visits from the pre- to the post-CBHP periods (1.7 to 2.5 visits) (p<.003).
Conclusions
CBHP is demonstrating the application of the integrated care model in community health centers in order to improve access to behavioral health services for the growing population of uninsured persons in Houston (Harris County). A number of successful demonstrations of the model in different settings throughout the United States have been reported (
11,
12 ), but this is the largest that we are aware of specifically targeting persons without insurance. At an annual cost of about $800,000 per year, behavioral health services have been placed throughout the HCHD system and diagnostic and treatment services have been provided to approximately 3,000 people during the year. There was high provider satisfaction, and symptoms of treated patients improved. On the other hand, behavioral health staff reported that their full work schedules do not allow them to consult extensively enough with each other at the centers.
A more systematic evaluation is needed to determine how integrated services in community centers improve patient outcomes. This can be accomplished by using relevant outcome measures systematically applied to random samples of patients and control groups.
Acknowledgments and disclosures
Financial support for this project came from the Hogg Foundation for Mental Health and the Houston Endowment. The authors thank Paul Shank, the Harris County Community Health Center staff at Strawberry Community Health Center, Jose Bayona, M.D., M.P.H., and Tom Gavagan, M.D., M.P.H., for their assistance with this study and their contributions to the column.
Dr. Ostermeyer is on the speakers bureau of Eli Lilly and Company and AstraZeneca. The other authors report no competing interests.