In recent years the interest in more research on the international comparison of mental health care has increased because of the global burden of mental illness, the existing gap between "disease" and "resource" information in mental health, the lack of data from low- and medium-income countries, and the imbalance of resource availability between mental health and other health sectors (
1 ). The assessment of unmet needs is particularly important in Latin America because of the gap between mental health treatment needed and mental health treatment received that has been identified in this region (
2 ). Chile is an upper-middle-income country that provides an excellent case for study. Chile's experiences in designing and implementing care could be helpful to neighboring countries with less developed mental health systems.
In Chile mental health reform was planned and carried out in the 1990s, community care was organized by sectors, and mental health care was incorporated into primary care. The Chilean mental health system and the utilization of services have been described in previous studies (
3,
4 ); information available at the macro-level on care indicators has been compared with other countries in Latin America (
2 ) and with the global context (
5,
6 ). The comparison between Chile and Spain is particularly relevant because the health care system in Spain (a high-income country) was instrumental in the design of the health care reform in Chile. The mental care system of Andalusia (Southern Spain) was one of the models for designing mental health care reform in Chile.
There is a debate on how to improve international comparisons to provide relevant information for policy and planning in mental health. Most of the available information is provided at the macro-level (countries or regions). However, information gathered at the meso-level (municipalities, health areas, or districts) may diverge from data aggregated at higher territorial levels. The importance of meso-level information was shown in a previous comparison between Italy and Spain (
7 ), in which our meso-level results differed from the macro-level results provided by national health officers of the
World Mental Health Atlas (
6 ).
In mental health the name of a specific service does not define its main activities, and it is necessary to use an internationally agreed upon glossary of terms for classifying services. An agreement of terms is necessary in order to define exclusion and inclusion criteria for decisions about which services to include in the assessment and in order to provide clear guidelines to measure utilization. The European Psychiatric Care Assessment Team research network has developed a framework for international comparisons of service availability and utilization (
8 ). The European Psychiatric Care Assessment Team comparison focuses on the meso-level, includes operational definitions of both the target population and the catchment areas, takes as a unit of analysis the "main types of care" instead of individual services, incorporates inclusion and exclusion criteria, and provides a set of instruments for describing care indicators at the area level. The comparison also includes a standard description of activities within a given service and the mapping of main types of care and services within an area by using the European Service Mapping Schedule (ESMS).
The aim of this study was twofold. First, this study aimed to assess the usability of the ESMS in an upper-middle-income country (Chile). And second, this study aimed to compare mental health care in Chile and Spain by using the European Psychiatric Care Assessment Team approach, with indicators developed in a previous operational model of basic mental health community care and with data obtained from five catchment areas in the two countries.
Methods
Selection of small health areas
We selected areas with marked differences in organization and provision of services within each country following the prospect model of previous studies (
9 ). Urban areas with a population density ranging between 130 and 1,300 persons per square kilometer were selected for this study. Therefore, macro-urban and rural areas defined by population density were excluded in this study. In Spain, one urban area was selected in the North (Gavá, Catalonia), and another urban area was selected in the south (Granada Norte, Andalusia) because of the socioeconomic and health disparities found in other studies (
10 ) and because previous studies (
7,
9 ) have shown that these two regions have different organization models for their mental health services. Another urban area was selected in the region of Navarre (Rochapea). Rochapea was selected because it has been identified as a benchmark area for community care in Spain (
11 ). Two adjacent urban areas with different methods of service provision and service organization were selected in southern Chile: Concepción and Talcahuano. The organization of services in Concepción is more traditional and dates from the 1960s, whereas services in Talcahuano were completely reorganized during the mental health care reform in the 1990s.
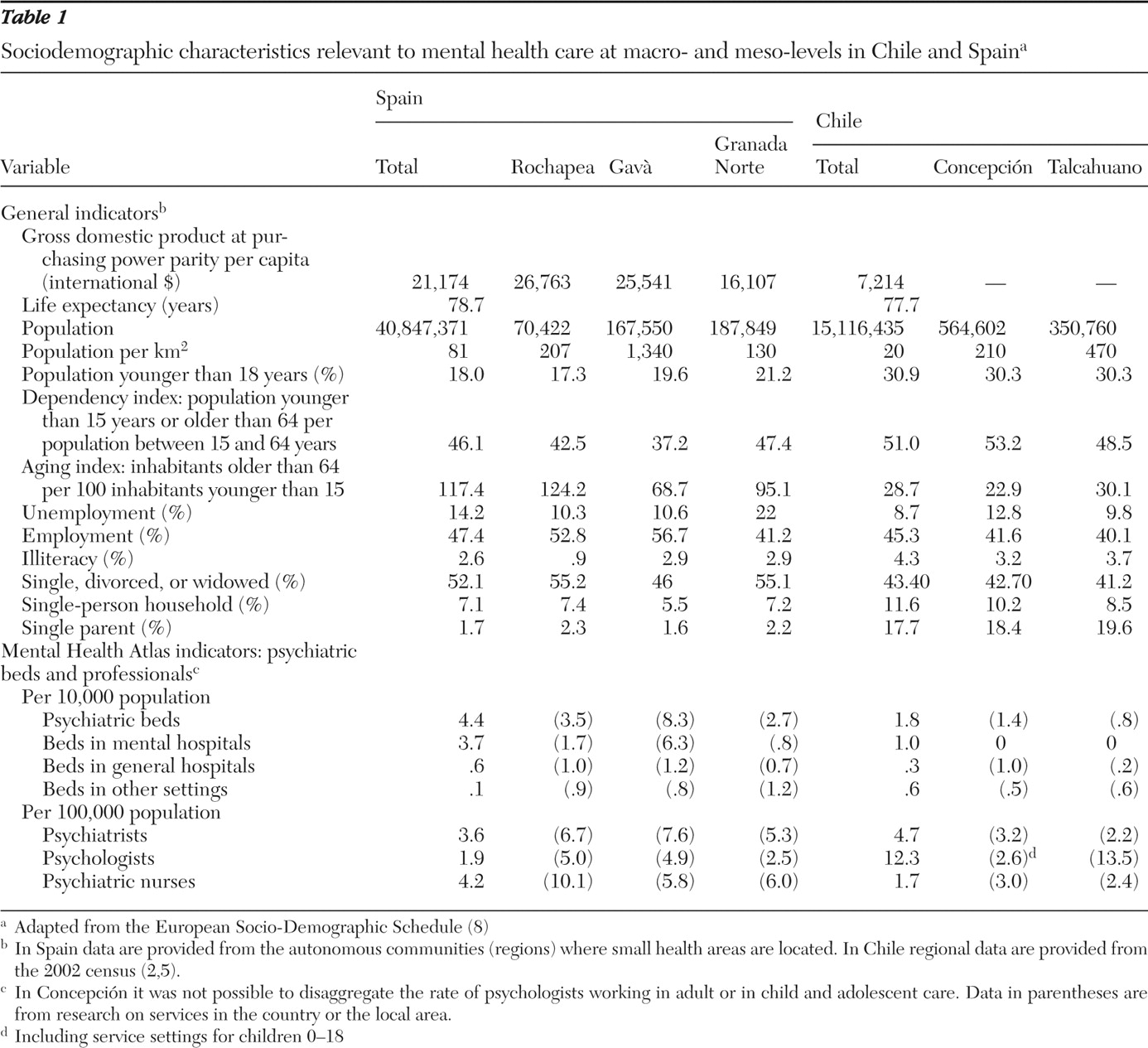
Description of catchment areas
The European Socio-Demographic Schedule was used along with other health indicators to describe the sociodemographic characteristics of each area (
8 ). Variables were selected on the basis of availability of data and evidence of relevance to mental health service utilization in previous studies (
12 ).
The ESMS
The ESMS (
13 ) is an instrument that serves three purposes. First, the ESMS is used to compile an inventory of adult mental health services of a catchment area. Second, it describes and compares the structure and range of mental health services between catchment areas. And finally, it measures and compares between catchment areas the levels of provision of major types of mental health services. The ESMS classifies services according to a number of descriptors, such as care typology, intensity, time of stay, and mobility. These atheoretical descriptors provide a classification based on the "main types of care," including residential care (ESMS branch code R), day care (ESMS branch code D), and outpatient and community care (ESMS branch code O). ESMS has four modules: introduction, service mapping (coding of main types of care at the small-area level), service counting (utilization of main types of care at the small-area level), and a listing of service characteristics. The full listing of ESMS codes (main types of care) can be found in previous studies (
13,
14 ). [An appendix showing the full listing and description of ESMS codes, along with the original questionnaire, is also available as an online supplement at ps.psychiatryonline.org.]
Three major contributions of ESMS are the use of an international terminology, its mapping structure, and its focus on main types of care instead of services. The ESMS glossary ruled out the use of culturally laden words (for example, rehabilitation) and common names of services that cannot be compared across territories (for example, day center). The ESMS tree divides care into several main branches according to whether the patient sleeps in the setting, receives care in a day care facility, or has face-to-face contact with a health professional. Then care is subdivided into secondary and tertiary branches on the basis of other characteristics, such as intensity, time of stay, and mobility. Individual services may be coded with one, two, or more main types of care. Local arrangements impede service comparisons across territories; however, this problem can be overcome by comparing main types of care at the meso-level instead of comparing services at the meso-level. Psychometric properties of the Spanish version of ESMS and its expanded version for disability services are described elsewhere (
14,
15 ).
Procedure
Two trained researchers in Chile and five in Spain conducted the assessments. One international coordination meeting was organized, and monitoring was carried out online from the Spanish coordinating center. The data gathering was done in Spain in 2003 and in Chile in 2004 and 2005. In Chile sociodemographic data were obtained from national statistical sources and local officers, as well as other sources. In Spain mental health officers at the three regions (or autonomous communities, as they are called) were also contacted. An external interviewer made contact with every mental health unit in the five catchment areas. Data collection for the ESMS began in each area with a face-to-face interview with both the head of the community mental health center and the reference hospital setting. A map of the services within the area was made at these meetings, and the main local data sources were identified. Further information was obtained from interviews with managers and staff of other services. Where there were gaps, a one-month prospective survey of utilization of the relevant services was carried out by the local researcher.
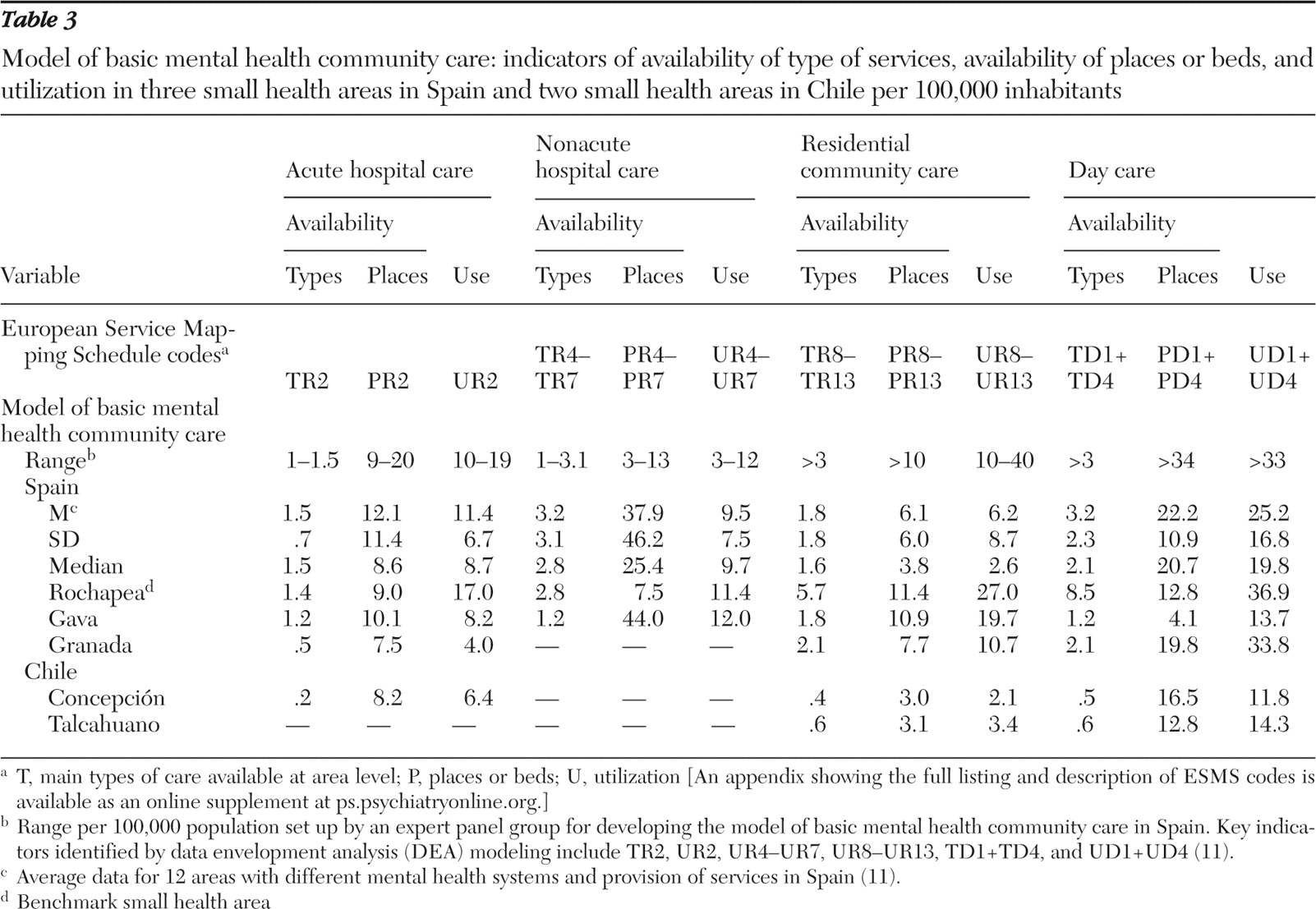
Twelve indicators derived from ESMS data were used to assess basic mental health community care in the five areas. "Basic mental health community care" is an operational model that provides a minimum indicator set to be collected prospectively in small mental health areas where information is poor or unreliable. It was developed by hybrid qualitative and quantitative techniques (a knowledge engineering approach combined with a data envelopment analysis) (
11 ).
The indicators used in this model included service availability, places, and utilization of residential care (ESMS branch code R) and basic day care services (ESMS branch code D—D1 for day services and D4 for structured services). Three main variable categories were considered: T for types of care (that is, availability of main types of care in residential and day care facilities within the area), P for places (that is, places and beds available per 100,000 population), and U for utilization (service utilization in residential and day care per 100,000 population). These variables (T, P, and U) were considered in each ESMS group of codes to provide the number of services available, places available, and use by every ESMS main type of care. According to the model, efficient small health areas should have a high availability and use of acute care (TR2, PR2, and UR2), avoiding overuse; they should also have low availability and use of hospital nonacute care (TR4 to TR7, UR4 to UR7, and PR4 to PR7); and they should have high availability and use of both residential nonhospital care (TR8 to TR13, UR8 to UR13 and PR8 to PR13) and basic day care (TD1 plus TD4, UD1 plus UD4 and PD1 plus PD4). [An appendix showing the full listing and description of ESMS codes is available as an online supplement at ps.psychiatryonline.org.]
The indicators used in this study were derived from a data envelopment analysis (DEA) model described elsewhere (
11 ). In summary, the data envelopment analysis model selected a minimum indicator set composed of six indicators: two inputs and four outputs that describe technical efficiency at small health areas. This model was previously tested in 12 small health areas in Spain, and it included both nontransformed and transformed variables. In a classical data envelopment analysis model, a small health area with high input values and with low output production would be considered as less efficient than one with low input values and high output production. However, this may not be the case of some positive inputs, such as high availability of acute care, community residential care, and day care. If the original values of these variables are maintained, the efficiency of the corresponding small health area will yield an incorrect classification. In order to manage this situation, transformed values were obtained for a subset of variables. The original values were subtracted from a subjective value close to and over their maximum; this mathematical transformation only implies a scale variation for adapting the algebraic model to expert knowledge about the variable behavior.
Inputs selected were availability of acute care (transformed TR2) and day and structured care (transformed TD1 plus transformed TD4). The four outputs were use of acute care (UR2), use of long-term hospital care (transformed UR4 to transformed UR7), use of long-term residential community care (UR8 to UR13), and use of day care (UD1+ UD4). This indicator set was used to test technical efficiency, to identify benchmark areas, and to quantify inefficiency in small mental health areas in Spain (
11 ).
Data analysis
Service utilization data were analyzed via visual inspection, because of their exploratory nature, the purposive basis of sampling, and the small number of areas inspected. The qualitative rating of the small health areas was provided by a four-member expert panel using basic mental health community care as a reference tool and descriptive data from every area (
11 ). The basic mental health community care model is available from the authors.
Discussion
The comparison of national data on mental health care has been a major advance in service research. Of course, comparisons between Spain and Chile should take into account the significant differences in economic growth and in the overall development of the health care systems. Spain is ranked 24th and Chile is ranked 56th in the list of countries of the world sorted by their gross domestic product at purchasing power parity per capita (
16 ). The health system in Spain was ranked seventh in the
World Health Report 2000, and the one in Chile was listed 33rd (
17 ). Although the percentage of the gross national product expenditure on health is similar in the two countries, the share of the health expenditure on mental health is 2.14% in Chile (
2 ) and from 5% to 8% in Spain, depending on the region (
18 ). However, national data may hinder the detection of significant differences because of the ecological effect, problems in data collection and aggregation, and care practice variability, as well as other causes (
19 ).
ESMS was designed to perform meso-level comparison in Europe. It has been applied in over 20 European countries, and its usability has been tested in comparisons among upper-income countries (Denmark, Italy, Spain, the Netherlands, and the United Kingdom) (
7,
20 ) and between upper- and upper-medium income countries (Norway and Russia) (
21 ). In North America, ESMS has been used for describing mental health services in Quebec (Canada) (
22 ).
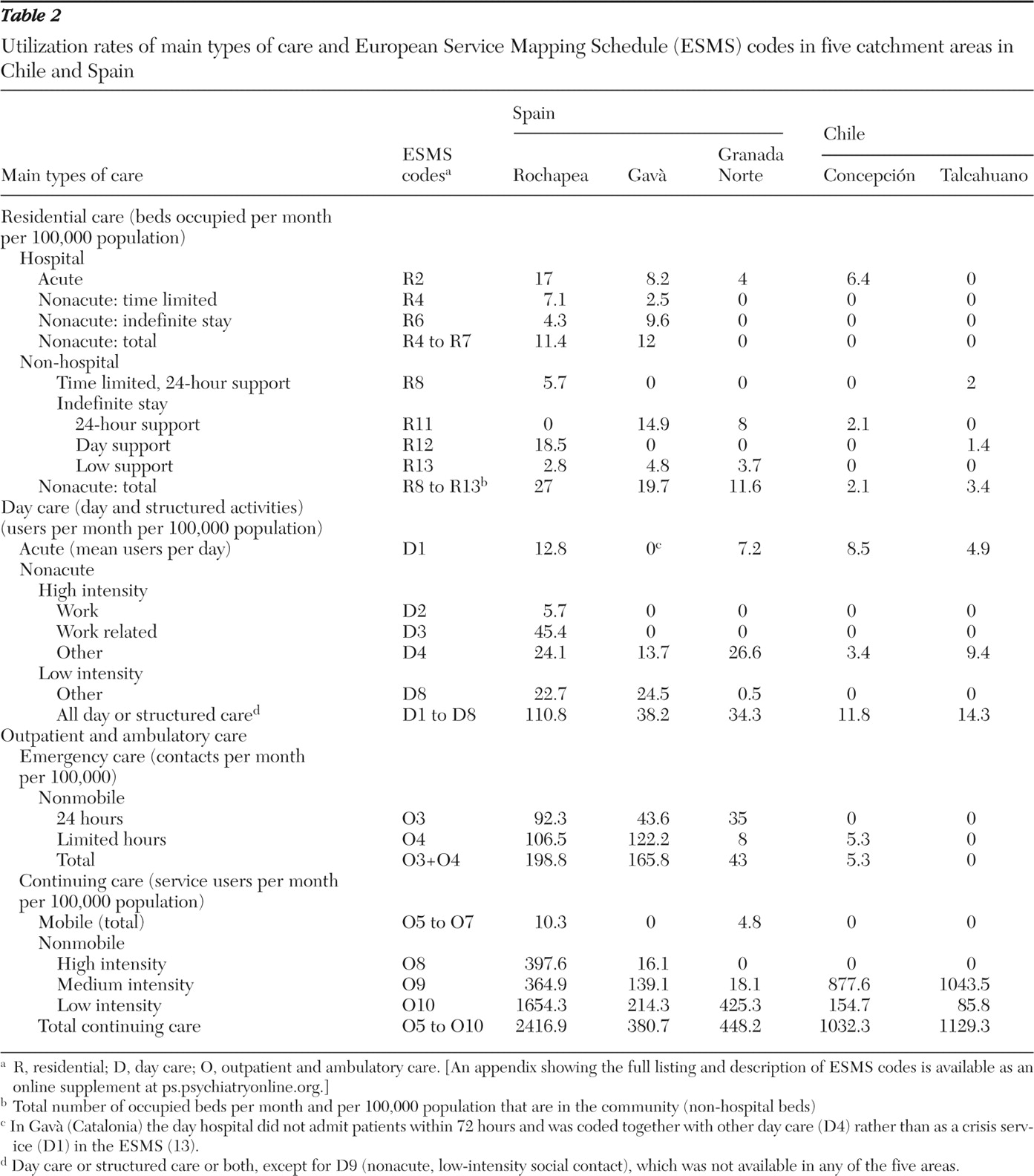
The study presented here shows that ESMS may also be used to compare services between countries in different International Monetary Fund groups and in different world regions, at least where care is organized in sectors. Our results must be interpreted with caution, given their exploratory nature and the purposive basis of sampling. In any case these results suggest trends that are evident upon visual inspection of the data in
Tables 1,
2, and
3 . As expected, differences were found between national rates of psychiatric beds and professionals and in the meso-level information gathered in the five local areas. These differences go beyond local variability. In Spain the data provided by national officers to the World Health Organization (WHO) (
6 ) were outdated and clearly below the actual numbers. Our study found higher rates of beds in settings other than psychiatric hospitals and general hospitals in the two local areas in Chile, compared with other studies that examined national data. This difference may be explained by differences in registering and updating this information at the national level. The large differences in the rate of available psychologists between Chile and Spain indicated by macro-level data were not as large when local-level data were examined. This finding illustrates the distinct pattern of outpatient care in Chile.
Despite our study's prospective nature, the meso-level data presented here indicate commonalities and differences between the care system in Spain and the one in Chile. Our study, which examined small areas, identified problems in mental health care that were not identified by the description provided by the WHO-AIMS at the national level (
5 ), such as the lack of 24-hour emergency services. It also identified the magnitude of the gap between mental health treatment needed and mental health treatment received described by previous papers in several indicators related to service utilization (
1,
2,
3,
4 ). The rate of outpatient continuous care in Chile (O8 to O10) is closer to that found in the benchmark area in Spain than in the two other areas in Spain. [An appendix showing the full listing and description of ESMS codes is available as an online supplement at ps.psychiatryonline.org.] This may be attributed to the addition of psychological mental health contacts in primary health care to specialized outpatient care in Chile. The high utilization of outpatient continuous care in the benchmark area of Rochapea may be related to a higher overall availability of services in this area and its impact on demand as well as to the clinical practice pattern in this area. The indicators used here are based on residential and day care because of the distinct care pattern provided by intermediate and residential service availability, in comparison with outpatient care (
23 ).
The study found large differences in the availability of day care and acute care between the benchmark area of Rochapea in Spain and all of the other areas examined. It is important to note the disparities between the availability of day care and the high utilization of these services within Granada Norte. This may be attributed to the fact that all day care services for a broad area of the Granada province were placed within the small area of Granada Norte. Therefore, users in this area have access to services originally planned for users from the other three areas within the Granada health district. In any case, delivery and use of mental health care in Chile was not so different from the pattern of care found in the catchment area of Granada Norte in Southern Spain, despite the large differences found in economic and macro-level indicators between the two countries.
The operational model of community care used here could be adapted to the characteristics of Chile, despite the lack of reliable monitoring systems and mental health databases. Of course, the ranges of the indicators of types of services suggested in Spain (
Table 3 ) are not applicable in Chile, but these values may drive a related model applicable in this country in the future. However, the mental health care imbalance described for Latin America merits further meso-level investigation, including ESMS description of health areas in other medium-income countries in the region.
The usability of the ESMS coding and mapping in the United States is beyond the scope of this article. However, the ESMS approach to service comparison shares many similarities with the proposals made by Walter Leginski and colleagues at the U.S. Department of Health and Human Services in the late 1980s (
24 ). The 2003 report of the President's New Freedom Commission on Mental Health found that fragmentation is a serious problem of the U.S. mental health system and suggested the implementation of Comprehensive State Mental Health Plans (
25 ). ESMS may provide a better understanding of the public mental health organization at the county level (
26 ) and on the geographical integration of care delivery (
27 ). Studies comparing service availability and use between Canada and the United States (
28 ) may also benefit from using a standard system for coding and mapping services at the meso-level.
Acknowledgments and disclosures
This research was partly funded by grant PAI: P06-CTS-01765 from the Andalusian Research Plan, by grant RD06-0018-0039 for the Network of Primary Care Research in Spain (Red de Investigación en Actividades Preventivas y Promoción de la Salud, Instituto Carlos III), and by grant AECI-A/013204/07 for the Spanish International Cooperation Agency (Secretaría de Estado de Cooperación Internacional) in Spain, by grant 1030605 from Proyecto FONDECYT, and by grant 80. 09.322 from Proyecto Universidad del Desarrollo in Chile. The authors thank the members of the Psicost Scientific Association (Juan Carlos García-Gutierrez, M.D., Susana Ochoa, Ph.D., Francisco Torres, M.D., Ph.D., and Vicente Madoz, M.D.), the Catalan Department of Health, the Maristán and the European Psychiatric Care Assessment Team (EPCAT), and the Mental Health Economics European Network (MHEEN-II) research networks, which provided support and advice to this study.
The authors report no competing interests.