Alcohol and drug use patterns among psychiatric outpatients have been underinvestigated in contrast to substance abuse and dependence (
1 ). Yet there is significant potential for subdiagnostic alcohol and drug use to exacerbate psychiatric problems. For example, even moderate alcohol use may have a negative impact on antidepressant response (
2 ) and increase the risk of side effects.
Although treatments for substance problems (including alcohol) are most successful at early stages, most people do not seek treatment until their condition is severe. Instead, many individuals with alcohol or drug problems, especially women, first seek psychiatric services (
3 ). In these settings, providers often fail to recognize drug use or heavy drinking (
4 ). As a result, potential substance use problems go untreated.
To better identify alcohol and drug use, computerized screening may be a useful innovation. Self-administered systems could increase patient comfort and self-report validity for sensitive questions on quantity and frequency of alcohol and drug use, compared with face-to-face interviews (
5 ). However, little is known about the feasibility of self-administered screening systems. To address these issues, we report on the implementation of routine electronic assessment in a psychiatric outpatient clinic. Using the electronic patient records generated by consecutive admissions, we investigated the prevalence of alcohol and drug use, including gender differences, to inform potential interventions.
Methods
Study participants were men and women seeking outpatient services at the Langley Porter Psychiatric Institute of the University of California, San Francisco (UCSF), who completed an electronic intake survey. The outpatient program includes both adult and geriatric clinics. Patients are mainly referred by their insurance carrier or are self-referred. There are no formal services for patients primarily seeking chemical dependency treatment or who have co-occurring alcohol or drug dependence in addition to a mental disorder.
Demographic questions included date of birth, gender, ethnicity, education, employment, and marital status. For each substance (alcohol, cannabis, cocaine, amphetamines, hallucinogens, ecstasy, sedatives other than as prescribed, opioids other than as prescribed, and tobacco) participants were asked if they had ever used that substance during their lifetime (responses were yes, no, or refuse to state). Participants who responded yes were asked about their most recent use. Questions covered usual quantity (in standard drinks), frequency of use in the prior 30 days, and number of days when five or more drinks were consumed on an occasion (
6 ).
All patients had scheduled appointments for initial evaluation at the Langley Porter Psychiatric Institute Adult Psychiatry Clinic at UCSF. Patients arrived one hour early to fill out paperwork, including demographic data and billing forms, and to complete the Electronic Health Inventory (EHI) as part of clinical intake procedures. Individuals were screened by telephone before intake. Patients with serious alcohol or drug problems (who self-identified as having a primary substance problem or a substance problem co-occurring with a mental disorder, requested chemical dependency treatment, or reported dependence symptoms) were referred to programs elsewhere in the community.
The EHI is a self-administered computerized questionnaire developed by clinical and information technology staff in cooperation with researchers in the UCSF Department of Psychiatry. Patients completed the instrument on private computers in the clinic intake area. Although not reported here, the inventory also covers medical history, pain, depression, and functional measures. This inventory is designed with the Ultimate Survey Web-based program (
7 ), which has a simple user interface with primarily multiple-choice questions and a branching structure. Participants indicating risk of prior-year alcohol problems based on usual quantity (three or more drinks), frequency (three or more times per week), or heavy drinking (five or more drinks on one occasion at any time in the prior year) were directed to complete the Short Michigan Alcoholism Screening Test (SMAST), a valid and reliable 13-item self-administered scale to detect lifetime alcohol problems (
8 ).
The clinic's front desk staff provided patients with a log-in number to protect security and assisted them with logging in or navigation if needed. Patients unable or unwilling to use the computer were given a paper version to be completed with their provider. For example, patients arriving late and patients from the geriatric clinic were more likely to be offered the paper version. The computerized system was presented to patients as a standard component of clinical intake. Once the inventory was completed, front desk staff printed out an EHI report for use in evaluating the patient.
The study team obtained permission from the UCSF Committee on Human Subjects to examine deidentified records of patients who had an initial clinic visit between September 30, 2005, and October 31, 2006. This approval included exemption from informed consent procedures.
Using t tests and chi square tests, we compared demographic characteristics of participants completing the EHI with characteristics of other clinic patients. Among those completing the EHI, we compared gender differences on alcohol and drug measures. Analyses were conducted with SPSS.
Results
During the study intake window, 422 patients ages 18 to 91 completed the EHI, representing 75% of new outpatients. Compared with the other 25% of patients (N=138), patients completing the EHI were younger, with a mean±SD age of 42.9±15.0 years compared with 55.6±17.5 years for those not completing the EHI (t=8.27, N=588, df=1, p<.001), but there were no other demographic differences.
The EHI sample (N=422) included 292 women (69%), 128 men (30%), and two transgender individuals (1%); 202 single (48%), 169 married or partnered (40%), 34 divorced or separated (8%), and 15 widowed individuals (4%). Ethnic composition included 302 white patients (72%), 39 Asian (9%), 26 black (6%), one Native American (0%), 31 Hispanic (7%), and 25 other (6%). For highest education level, 53 patients were high school graduates or nongraduates (13%), 53 had some college (13%), 134 were college graduates (32%), and 172 had some graduate training (41%). The sample included 223 patients employed full-time or part-time (53%), 49 unemployed (12%), 53 students (13%), 54 retired (13%), 34 on disability (8%), and nine unknown (2%) (data not shown).
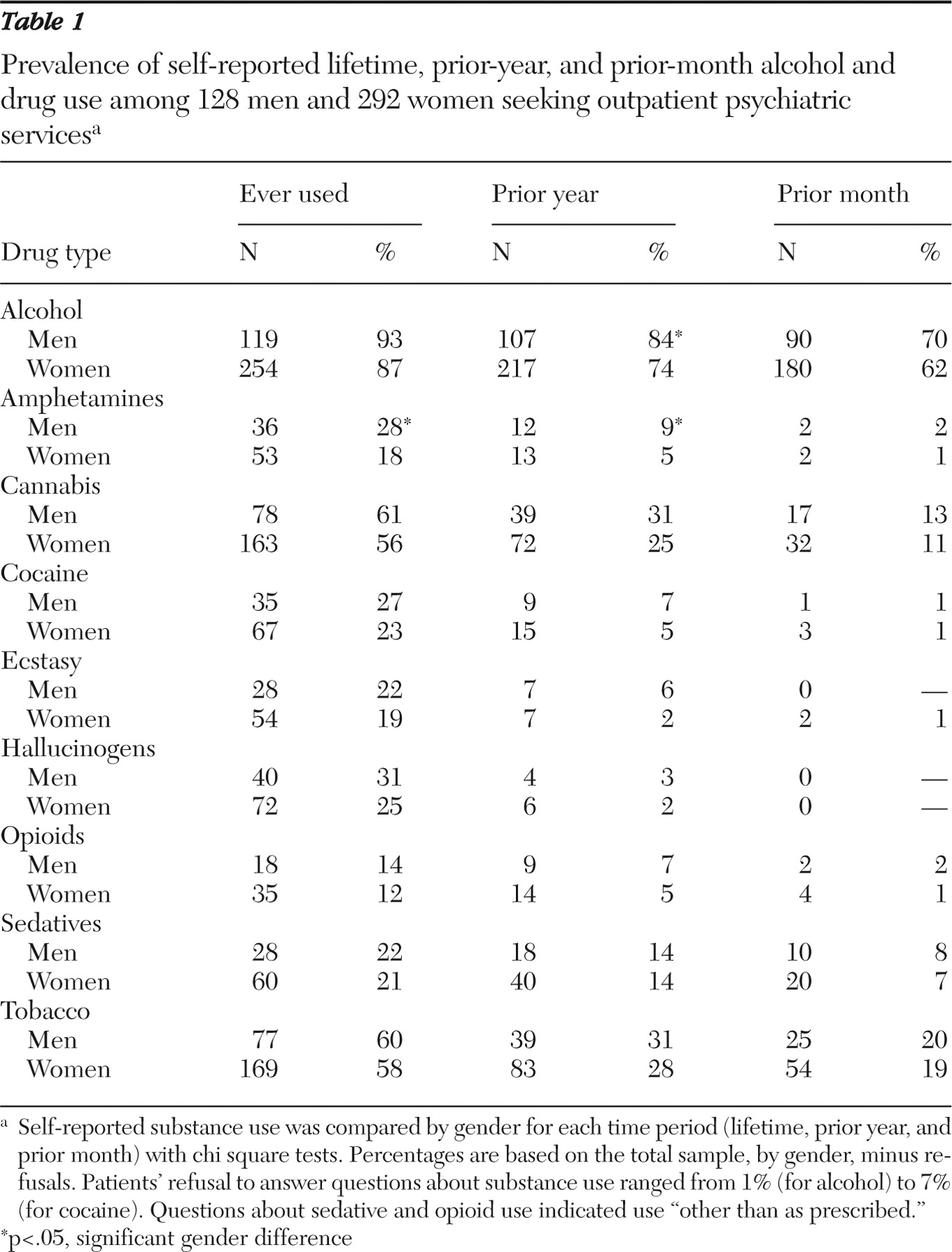
Lifetime, prior-year, and prior-month substance use are reported by gender in
Table 1 . Prior-year alcohol use was reported by 84% of men versus 74% of women (p=.023), lifetime amphetamine use by 28% of men compared with 18% of women (p= .011), and prior-year amphetamine use by 9% of men compared with 5% of women (p=.044). Heavy drinking in the prior month (five or more drinks on at least one occasion) was reported by 37 men (29%) and 41 women (14%) (p<.001) (data not shown).
Among those who consumed alcohol in the prior month (N=270), usual quantity was 2.4±1.5 drinks for men and 1.8±1.0 drinks for women, (p<.001), frequency was 9.9±8.7 days for men and 8.6±7.9 days for women (comparison not significant), and heavy drinking was reported by 37 men (41%) and 41 women (23%) (p= .001). Of 49 patients using cannabis in the prior month, frequency was 10.8±11.8 days for men and 12.1± 11.0 days for women (comparison not significant).
Of the 422 participants, 70 of 128 men (55%) and 108 of 292 women (37%) were administered the SMAST because of their drinking patterns. Sixteen men (23%) and 22 women (20%) scored 3 points or higher out of 13 points, suggesting a possible lifetime alcohol problem (
8 ) (data not shown).
Discussion
Because of our interest in the potential impact of substance use on psychiatric services, we conducted this study to examine patterns of alcohol and drug use in an outpatient psychiatry clinic, which were based on an electronically self-administered instrument. Results showed that alcohol and drug use, especially heavy episodic drinking and use of cannabis, were prevalent. With the exception of heavy episodic drinking, women's rates of use were similar to men's on most measures. These findings have implications for the development of appropriate substance use interventions, which are integral to effective psychiatric services (
9 ).
The levels of substance use in our results, similar to those found in a primary care sample with depression (
10 ) and an emergency services sample (
11 ), indicate that a substantial number of patients were at risk. The results suggest that providers in psychiatric settings should conduct screening and offer treatment as needed. For example, brief motivational interventions could effectively supplement other psychiatric services (
12 ) and prevent escalation of alcohol and drug problems. The recent Screening, Brief Intervention, Referral, and Treatment initiative launched by the Substance Abuse and Mental Health Services Administration (
13 ) is actively promoting early intervention with nondependent patients in primary care, mental health care, and other settings; online resources and multiple training opportunities are available for providers. Effective January 2008, codes approved by the U.S. Centers for Medicare and Medicaid Services allow reimbursement for screening and brief intervention. These policy initiatives recognize that early alcohol and drug use identification and treatment are important medical services that can improve multiple health outcomes.
As a mechanism to facilitate identification, we found that the computerized system was acceptable to most patients, consistent with a prior study of computerized depression assessment (
14 ). Alcohol and drug use questions also were acceptable (few patients declined to answer), although we note that patients with serious alcohol and drug problems had previously been screened out. One limitation was that older adults appeared less willing or able to use the computer, but this may have been due in part to disabilities (including cognitive impairment) of patients seeking geropsychiatric services or to assumptions of reception staff regarding disabilities. Service issues for further investigation include staff training, optimal procedures to ensure confidentiality (
15 ), software options for alcohol and drug screening, and computer-based interventions (
16 ). Potential benefits of computerized systems include the ability to collect more detailed information than is easily obtained by paper forms, greater validity for sensitive questions, and more time-efficient assessment. The records obtained from patients are useful for treatment planning at a program level and as a resource for clinical and services research.
These findings need to be interpreted with the limitations of the study. Because patients completing the electronic intake were younger on average than those who did not complete it, our substance use findings are less representative of older adult patients. Prevalence findings from a single location (San Francisco Bay Area) may not generalize to other regions. Our results may not generalize to psychiatry clinics that do not prescreen patients with serious alcohol and drug problems before intake. It would have been preferable to use a lower heavy-drinking cutoff for women than men (that is, four drinks rather than five on one occasion) because women are more sensitive to alcohol. Our use of the higher cutoff indicates that our findings regarding heavy drinking by women may be conservative. Although computerized measures are considered valid, underreporting of alcohol and drug use by patients would also make our prevalence rates conservative. Thus substance use in the sample may be even greater than our results indicate.
Conclusions
Computerized self-administered assessment can be effectively integrated into an outpatient psychiatric setting to improve alcohol and drug screening. Our investigation based on electronic patient records found substantial prevalence of alcohol and drug use among men and women seeking psychiatric treatment, highlighting potential intervention needs.
Acknowledgments and disclosures
This study was supported by grants from the Steven Merrill Family Foundation, grant K23-AA015411 from the National Institute on Alcohol Abuse and Alcoholism, and grants R37-DA10572 and P50-DA09253 from the National Institute on Drug Abuse. Members of the Depression Center of the Department of Psychiatry, University of California, San Francisco, and the Drug and Alcohol Research Team at the Kaiser Permanente Division of Research provided valuable assistance in the development of the study. Information technology staff of the University of California, San Francisco, Department of Psychiatry (Ann Saggio, B.A., Cynthia Chappell, B.A., Julio Burroughs, B.S., Ben Estocapio, B.S., Catherine Dunne, M.S.), as well as Paul Fenimore, M.A., and Kim Terry, B.A., contributed to the study through design of the Electronic Health Inventory (EHI) and associated data management systems. Staff of the Langley Porter Hospital and Clinics integrated the EHI into clinical intake procedures.
The authors report no competing interests.