Individuals with serious mental illness experience higher mortality rates than the general population, to an extent that is not explained by unnatural causes such as suicide or accidents (
1 ). Multiple studies document a higher prevalence of chronic illnesses, such as diabetes (
2 ), respiratory disease (
3 ), hepatitis B and C, and HIV (
4 ), in this population compared with the general population. These high rates of chronic medical illness among individuals with serious mental illness may be due to a number of issues, including lifestyle factors (such as smoking and substance abuse), side effects of treatment (for example, weight gain associated with psychotropic drugs), reduced receipt of preventive medical services (
5 ), or diminished quality of care compared with those with similar medical illness but no mental disorder (
6,
7 ).
General medical services may have the potential to improve health outcomes among individuals with serious mental illness (
8 ). With regard to schizophrenia, two expert panels have published recommendations for increased efforts in physical health monitoring by mental health providers in collaboration with primary care physicians (
9,
10 ). As a result, identifying and quantifying levels of access to medical care and perceived barriers to access among persons with serious mental illness would be important to informing the development of interventions to improve the health of this population. Although there is a substantial body of literature on the quality of service received by persons with serious mental illness who access care (
6,
7,
11,
12,
13,
14,
15 ), there is limited population-based research about persons with serious mental illness and their access to medical services.
Previous attempts to quantify medical care access among individuals with mental disorders have shown mixed results. For example, one study of outpatient medical service use by veterans discharged from Veterans Affairs (VA) psychiatric hospitals (
16 ) reported that diagnoses of schizophrenia, posttraumatic stress disorder, and substance abuse all predicted lower outpatient VA medical service utilization. Another study (
17 ), based on the 1994 National Health Interview Survey (NHIS) data, reported no difference in insurance status or having a primary care providerbetween individuals with a mental disorder and the general population; however, individuals with mental disorders were more likely to delay care or to be unable to obtain care. In another study, investigators evaluated general medical utilization of 200 patients with serious mental illness (100 with psychotic disorders and 100 with affective disorders) (
18 ) who were in treatment at two outpatient psychiatric centers and compared them with matched samples of persons who completed several national surveys. The authors reported that individuals with mental disorders used general medical services at higher rates than the general population, despite higher perceived barriers. Other studies confirm that type of psychiatric diagnosis is related to use of health services for general medical problems (
19 ). Further, several studies have examined the impact of major depression on morbidity and mortality within a primary care context (
19,
20,
21,
22,
23,
24,
25 ).
It is possible that the discrepancies among these studies are a result of differences in study populations and methods used to assess service use outcomes. Specifically, when the populations have involved patients with serious mental illness, the samples have not been nationally representative (
18 ). Conversely, when samples have been nationally representative, the studies have not focused specifically on medical care access for people with serious mental illness (
17 ). As a result, the aim of this study was to fill this gap in the literature by using data from the NHIS and its disability component (NHIS-D) (
26,
27 ) to examine medical care access and barriers among individuals with serious mental illness, compared with those without these conditions. For the purposes of this study, we defined serious mental illness as psychotic spectrum disorders, bipolar disorder, and major depressive disorder. On the basis of our synthesis of the existing literature and clinical experience, we hypothesized that individuals with serious mental illness would report a regular source of primary care less often than individuals without a mental disorder and that individuals with serious mental illness would report perceived barriers to medical care more often than those without a mental disorder.
Methods
Sample
We combined the 1994 and 1995 NHIS and NHIS-D (
26,
27 ) data sets to provide a sample of 156,475 individuals over age 18 years. The NHIS is a nationally representative survey sponsored by the Centers for Disease Control and Prevention and is conducted to provide information on various health-related issues in the noninstitutionalized U.S. population. The surveys conducted in 1994 and 1995 included a detailed section on access to care and a disability component (NHIS-D), which included questions on psychiatric diagnoses and symptoms. The information on psychiatric diagnoses and access to medical care that could be obtained by combining these data sets allowed examination of our study hypotheses. Further, none of the subsequent NHIS surveys contained all of these elements. In these surveys, individual-level data used in the analyses were provided by one household member. Response rates for the 1994 and 1995 NHIS Core Survey and the NHIS-D phase I were high (92.5%–94.1%). Both surveys have been described in detail elsewhere (
26,
27,
28 ).
Measures
We studied groups of dependent variables that were available in NHIS as they related to our study hypotheses. We defined "regular source of primary care" as having a primary care physician as a regular source of medical care. Participants were asked a series of questions leading to a designation about whether they had the following: a single regular source of care; multiple regular sources, but see one source most often; multiple regular sources, but no one source seen most often; or have no current regular source of medical care. We dichotomized these designations; the first two indicated that participants had a regular source of medical care, and the other two indicated that participants did not have a regular source of medical care. Those who reported having a regular source of medical care were asked which type of provider they saw. We considered family doctor, general practitioner, internist, pediatrician, and obstetrician-gynecologist to be primary care physicians. Respondents who identified specialists as their regular source of medical care were considered to not have a regular source of primary care. Finally, regarding reported barriers to medical care, we examined responses to items about being unable to get medical care when it was needed, delaying medical care due to concerns about cost, and being unable to get a needed prescription medication.
Our independent variables were mental disorder diagnostic category, age, gender, race, education, income, and health insurance status. Respondents in this survey were asked a series of questions about mental disorders over the past 12 months. We included all those who answered in the affirmative to having had schizophrenia or paranoid or delusional disorder, other than schizophrenia (grouped together as psychotic disorders, N=592); manic episodes or "manic depression," also called bipolar disorder (N=511); or major depression (N=1,828). The question about major depression included the following definition: "Major depression is a depressed mood and loss of interest in almost all activities for at least 2 weeks." The reference category was defined as negative answers to all questions about any mental disorders, including psychotic disorders, bipolar disorder, major depressive disorder, dementia, personality disorders, or other mental disorders seriously impairing functioning. Individuals who reported taking medicines for mental or emotional conditions also were excluded from the referent group. Presence of alcohol use disorder or drug use disorder was used as a covariate. Insurance coverage, age, and education were dichotomized as presence or absence of any type of health insurance, being or not being older than 42 (median age for adults in the sample), and having or not having a high school diploma or equivalent, respectively. Family income was divided into three categories: $0–$14,999, $15,000–$34,999, and $35,000 and above. Race was categorized as white, black, or other.
Analysis
Pearson's chi square analysis was used to compare categorical demographic characteristics. Logistic regression was used to examine the relative association of each outcome to categorically defined mental disorders. Unadjusted odds ratios for each diagnostic category for the presence or absence of each outcome variable were calculated, as well as odds ratios with adjustment for each of the covariates described above. SAS version 8.2 was used for the initial analysis. SUDAAN statistical package 8.0.0 (
29 ) was used for the final analyses to account for appropriate weights of the stratified sample design, by using the methods described on the National Center for Health Statistics Web site (
30 ). The purpose of this method was to approximate a nationally representative sample.
Results
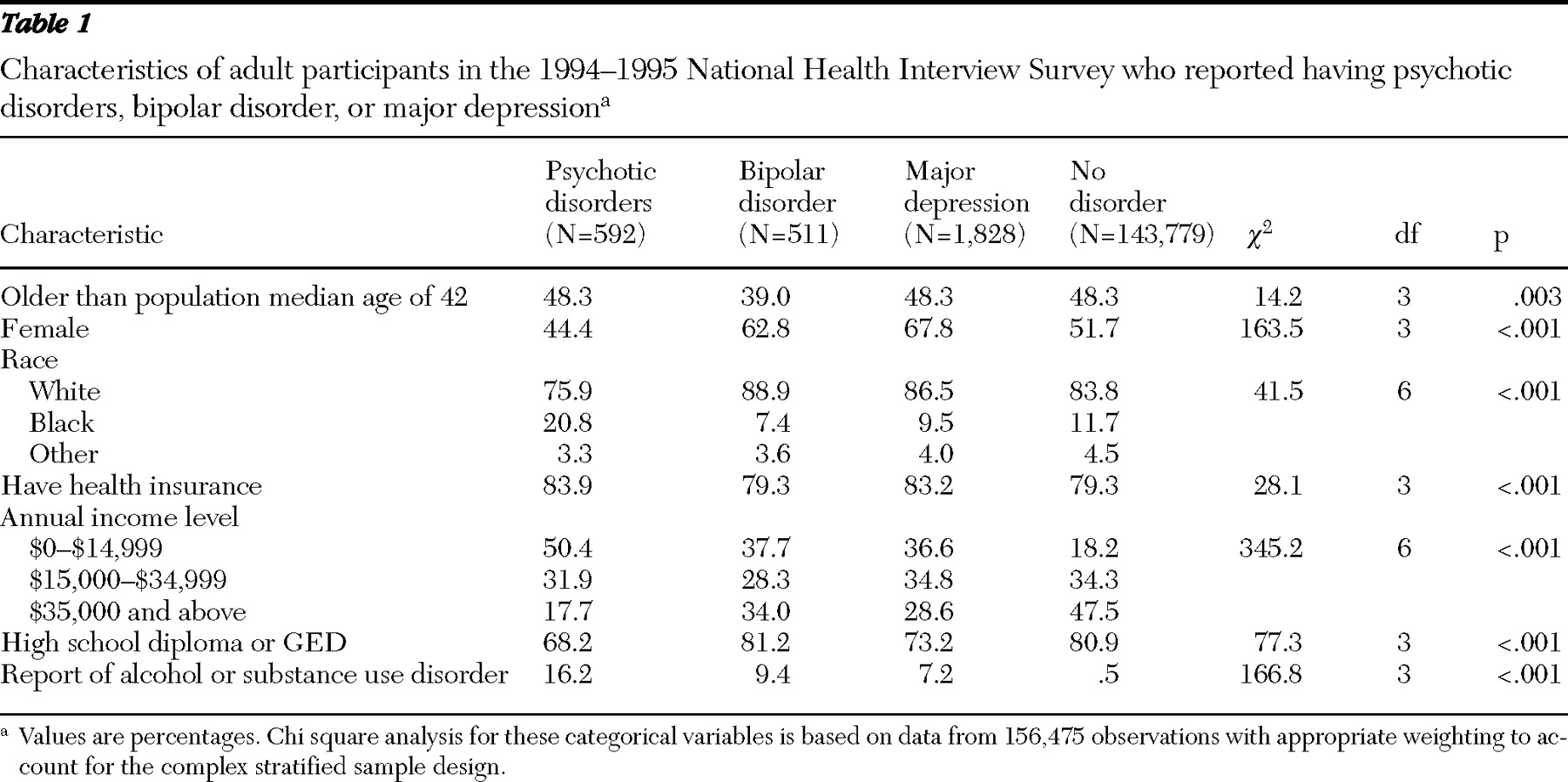
Table 1 shows the demographic characteristics of the study sample. Significant differences were found among the four study groups for all of the examined demographic variables. The median age among all adults in the NHIS sample was 42. In the psychiatric disorder groups that we studied 48.3% of those with a psychotic disorder were above this population median age, as were 39.0% of those with bipolar disorder, 48.3% with major depression, and 48.3% with no psychiatric disorder. As expected, respondents with mood disorders were more often female. Black respondents were somewhat overrepresented in the psychotic disorder diagnostic group. Although statistically significant, differences in rates of having some type of health insurance coverage were similar among the four psychiatric disorder groups, ranging from 79% to 84%.
Distributions of income showed that compared with those with no psychiatric disorder, respondents with serious mental illness more often fell into the lowest income category, with markedly fewer earning an annual income of $35,000 and above. Persons with psychotic disorders and major depression, but not those with bipolar disorder, less often reported having a high school diploma or GED than those with no psychiatric disorder. As expected, those with serious mental illness more often reported substance use problems. We also calculated the prevalence of each of our diagnostic categories using appropriate weighting. The 12-month prevalence of each diagnostic category was as follows: psychotic disorder, .43%; bipolar disorder, .39%; and major depression, 1.39%.
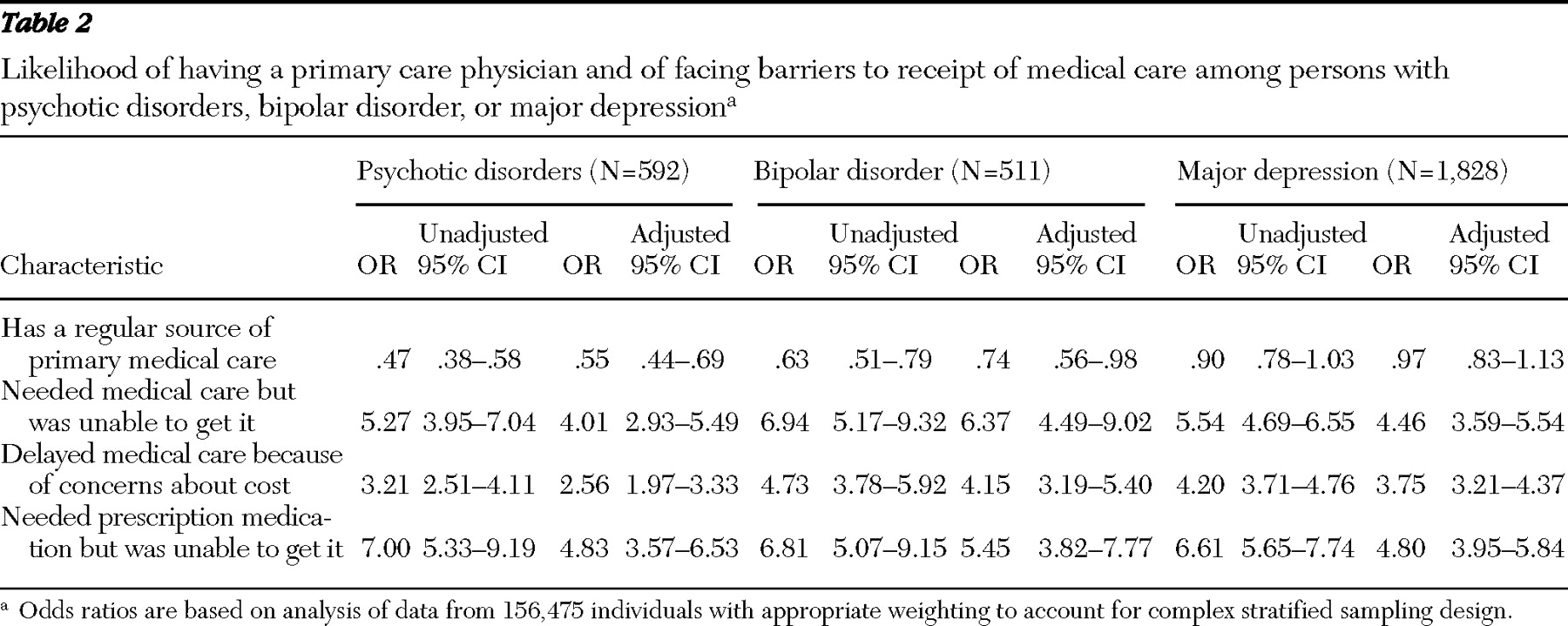
Table 2 shows the effect measures for having a regular source of medical care and various measures of reported barriers to medical care access. In both the adjusted and unadjusted analyses, individuals with psychotic disorders and bipolar disorder, but not those with major depression, were less likely to report having a regular source of medical care. In regard to reported barriers to medical care, for all three outcomes in both the adjusted and unadjusted analyses, respondents with psychotic disorders, bipolar disorder, or major depression were far more likely than the reference group to report difficulties in accessing care, with odds ratios ranging from about 2.5 to 7.0. In these analyses, adjustment for age, sex, race, education, income, health insurance status, and presence of an alcohol or drug use disorder changed the magnitude but not the direction of associations or presence of statistical significance at
α =.05 (shown in
Table 2 by a 95% confidence interval that does not include 1).
Discussion
To our knowledge, this is the first study to use a large, nationally representative sample to examine medical care access and barriers among patients who have serious mental illness. Our analysis of this survey data shows that individuals who reported having psychotic disorders or bipolar disorder were significantly less likely to report having a regular source of medical care compared with those who did not report psychiatric disorders. Persons who reported major depression were as likely to report having a regular source of medical care as those who did not report psychiatric disorders. Our findings are in contrast to prior reports showing that persons with mental disorders reported either similar or greater access to primary and general medical services than those without mental disorders.
The differences in the populations sampled may account for these discrepancies. For example, in the previous analysis (
17 ) of the 1994 NHIS data, having a mental disorder was defined broadly to include all types of mental disorders, instead of focusing on persons with serious mental illness. The study by Dickerson and colleagues (
18 ) used a sample of persons with serious mental illness from clinical settings and then compared the data with data from population-based national surveys. This study from one general location demonstrated higher rates of general medical care access for individuals with serious mental illness who were receiving mental health services. Because of the restricted treatment- seeking sample, the study does not reflect a population-based comparison of health service use by and barriers to care for those with and without serious mental illness. A major strength of our study is the use of a large, nationally representative, population-based sample provided by the 1994 and 1995 NHIS and NHIS-D.
Variability in the definitions of serious mental illness among authors in this subject area limits the comparability of this study with others. Although we chose to define serious mental illness as including psychotic disorders, bipolar disorder, and major depression, the inclusion of major depression was complicated because the definition in the survey of "depressed mood and loss of interest in almost all activities for at least two weeks" allows for a variety of mild, nondisabling conditions that are subthreshold to a full diagnosis. Consistent with previous reports, our analyses showed that individuals with psychotic disorders, bipolar disorder, or major depression reported higher levels of perceived barriers to medical services compared with those without psychiatric illness. Even after adjustment for demographic factors, odds ratios ranged from over 2.5 to nearly 5.0 for outcomes of being unable to get needed care, financial issues delaying care, and being unable to get a prescription medicine.
We interpret this result to mean that persons with psychotic disorders, bipolar disorder, or major depression have greater difficulties navigating the health care system to get their medical needs met. This conclusion suggests that increasing access to the same sources of medical care in the general population will not necessarily lead to improvement in the health of individuals with psychotic disorders, bipolar disorder, or major depression. Specialized sources of primary medical services may be required to best meet the needs of this population. Rates of preventive medical services provided at psychiatric visits for patients with serious mental illness have been shown to be very low, about 11% (
11 ). Integrating psychiatric and general medical care at a single site (
31 ) or increasing the role of psychiatric providers in general and preventive medical services may be possible solutions to this problem. For example, research has found that integrating depression care into primary care has resulted in positive outcomes such as improved treatment adherence and improved access to care for patients (
32,
33,
34,
35 ).
There are several clinical implications of these findings. The data suggest that in addition to the actual medical condition, access to consistent medical care can also influence rates of high mortality among people with serious mental illness. To the extent that symptoms of serious mental illness might impede accessing medical care, mental health providers should consider both mental health and physical health outcomes associated with a patient's mental disorder. In other words, the current results signal that psychiatric services and psychotherapeutic interventions for people with serious mental illness need to seriously consider how a patient's mental illness affects the patient's overall utilization of health care services.
At times, the dramatic nature of symptoms of serious mental illness may eclipse the need to focus on basic health needs of patients. But the findings indicate that even if a patient is psychiatrically stabilized but does not appropriately access medical care, the patient still may not be being optimally treated. Furthermore, although accessibility of primary medical care is a necessary requisite to addressing chronic health conditions, timely receipt of appropriate and quality treatments are also critical to the proper management of these conditions. Given the low-income status of many individuals with serious mental illness, many people in this group may experience barriers to receiving high-quality care even when a source of primary medical care is available. This consistent lack of accessibility of appropriate care only exacerbates the untreated, chronic medical conditions that characterize this population. As such, mental health clinicians working with people with serious mental illness may need to ask patients about their medical doctors and medical conditions, even if the mental health clinicians are not medically trained (social workers and psychologists, for example). Although the excess mortality experienced by persons with serious mental illness is probably influenced by access to primary care and other types of health care, other factors, such as the higher rates of certain chronic health conditions like hepatitis and HIV, also lead to increased mortality in this group. Our findings bring to light the importance of integrating physical and mental health care for people with serious mental illness.
There are several limitations to this study. First, the reliability and accuracy of categorizing mental disorders by simply asking participants whether they have a given mental disorder are unknown. However, this method has been used to assign specific mental disorders in previous reports on these data sets (
36,
37 ). Using this method of diagnostic categorization led to calculated 12-month prevalence rates of mental disorders as follows: psychotic disorders, .43%; bipolar disorder, .39%; and major depression, 1.39%. By comparison, the National Comorbidity Study Replication (
38,
39,
40 ) reported somewhat higher 12-month prevalence rates of psychotic disorders, major depression, and bipolar disorder of .3% (for nonaffective psychosis), 6.7%, and 2.6%, respectively. This study provided no means of evaluating the validity of the diagnostic questions used as a means of assigning psychiatric diagnoses. Second, it is possible that persons with serious mental illness may be more likely to report perceived barriers, regardless of actual barriers. However, several studies have demonstrated reliable self-report of health care utilization data by persons with mental illnesses (
41,
42,
43 ).
Conclusions
These results point to the need to improve systems of health care delivery to individuals with serious mental illness, particularly those with psychotic disorders. In order to more accurately characterize medical care utilization by persons with serious mental illness, national health surveys need to have more sophisticated methods of determining the presence of mental disorders, with evaluations of the validity of the methods used. Surveys should also provide a clear means of distinguishing between types of medical services. Possible solutions to this problem of patients with serious mental illness accessing needed care could be to incorporate more primary care services into the practice of psychiatry and improve methods of coordinating mental health and general medical care.
Acknowledgments and disclosures
Dr. Bradford was funded for this project by the Robert Wood Johnson Clinical Scholars Program when he was at the University of North Carolina School of Medicine. Dr. Kim was funded, in part, by grant R24-HS-013353 from the Department of Health and Human Services Agency for Healthcare Research and Quality and by grant P60-MD-000239 from the National Institutes of Health's National Center on Minority Health and Health Disparities. Dr. Marx and Dr. Butterfield were funded by Veterans Affairs Advanced Research Career Development Awards. The authors acknowledge Carol Q. Porter for her contribution to this project in data management and analysis.
The authors report no competing interests.