The share of mental health in total health spending is a topic of interest in international circles (
1,
2,
3 ), and the topic has been raised in Canada in several prominent government reports (
4,
5 ). Equality of funding across geographic populations has been a major policy objective for general health care in most Canadian provinces since the mid-1990s, when the provinces began integrating all health care services (except medical doctor services and outpatient drugs) under consolidated organizational structures called regional health authorities (RHAs). The formation of RHAs has been accompanied by the development of regional funding envelopes based on population characteristics. In Alberta, RHAs were formed in 1996, and a population-based formula that was based on regional population characteristics and that provided funding to RHAs was instituted several years later. Specialized mental health services were not integrated with general health services until April 1, 2003. An Alberta government report issued in 2001 recommended the enhancement of mental health services once the transfer of mental health services to RHAs was achieved (
6 ).
Until April 2003 a provincially designated Alberta Mental Health Board (AMHB) was responsible for providing almost all community mental health and psychiatric hospital services in the province. RHAs were responsible for emergency room care and general hospital acute care, some of which was for mental health care, such as acute inpatient services and outpatient centers. After the transfer, all of these services were the responsibility of RHAs. Both before and after the transfer, all mental health services were funded on a budgetary basis: that is, providers received an overall budget (rather than a per-unit payment, such as a fee per service or per day), and mental health service expenses had to be paid for within the budgets. RHAs had discretion as to how they allocated spending between mental and general health care, as long as it was within the overall budgets. During the entire period (before and after the transfer) all physician and covered outpatient pharmaceutical services were separately funded by the province.
An RHA is a bureaucratic organization, and Corrigan and Watson (
7 ) have shown that a variety of factors—availability of resources, perceptions of need, program effectiveness, and personal responsibility—will have an impact on the expenses that administrators will allocate to mental health. In a United Kingdom study, Schneider and colleagues (
8 ) showed that all health care costs were greater in a model with targeted funding for mental health services than they were in a model with integrated funding; however, they did not address the question about the monetary share of mental health services in relation to all health expenditures.
Recent research has shown that it is feasible to directly measure total mental health service costs that were provided by AMHB (before the transfer) and RHAs (
9 ) and to compare these to total health expenditures, as has been done in a number of other constituencies (
1 ). By using this approach, we can develop measures of mental health care's share of the expenses for total health care over several years, and thus we can determine how integrating mental health and general health services in Alberta affects mental health's share of total health expenditures. The purpose of the study was to determine the relationship between mental health and total health care spending after the integration of mental health services in Alberta.
Methods
The research question is whether the integration of mental health and general health services had an impact on mental health care's share of total health care expenditures. The economic "actors" in our analysis are the Alberta RHAs and AMHB (before integration). Our measure of mental health's share of total health care expenditures is the combined cost of providing mental health services by the two organizations, expressed as a percentage of the combined RHA and AMHB spending on all health care services, including mental health. We measured this ratio annually for four years before, and three years after, the integration date of April 1, 2003.
Services included in our mental health cost measure are psychiatric hospital services, community mental health services, general acute hospital services, emergency room services, and other ambulatory or outpatient services for mental health provided by the regions. All health services provided by the regions and AMHB were included in the total health care cost measure.
The measurement of mental health costs for the fiscal year (FY) 2003 has been reported in Block and colleagues (
9 ). We based our methods on that study.
Inpatient cost data for general acute care hospitals was based on average costs for case-mix groups. These case costs were developed for relatively homogenous clinical conditions such as "bipolar mood disorders" and "depressive mood disorders with electroconvulsive therapy" with differing levels of resource intensity. Details regarding this methodology are available through the Health Costing in Alberta reports issued by Alberta Health and Wellness. All individuals discharged from acute care hospitals whose primary diagnosis was coded as a mental health admission were included.
For outpatient services provided within acute care hospitals and other general health facilities, all mental health cases were identified on the basis of the diagnosis attributed to the visit. These cases are grouped according to the Alberta Ambulatory Care Classification System Grouper developed by Alberta Health and Wellness and are reported in the Health Costing in Alberta reports. This grouper combines conditions that have similar resource intensities (that is, costs). Visits to all outpatient centers were included where the main reason for the visit was for mental health services. This method extracted the cases from mental health outpatient centers, as well as cases from areas that are not dedicated solely to mental health care, such as emergency rooms. Each relevant case was multiplied by the corresponding unit cost, using the Alberta Ambulatory Care Classification System costing data.
Inpatient services within psychiatric facilities were assigned costs based on per diem amounts. The per diem was determined by the FY 2003 budget and was adjusted by 3% annually, which is approximately the rate of inflation in the province. The per diem cost was then multiplied by the number of patient days generated.
For outpatient services in psychiatric facilities, an average cost per new enrollment was calculated by using the FY 2003 costs and adjusted 3% annually. The average inflation rate for the province during this period was about 3% (
10 ). This cost was then multiplied by the number of new enrollments.
We assigned costs to community mental health clinics on the basis of the average cost per service event. The service event volumes were multiplied by average costs, based on the 2002–2003 costs and adjusted by 3% annually.
Tele-mental health services were assigned costs based on the FY 2003 costs and adjusted by 3% annually. The activity measure identified each year was the number of clinical consultations. Other costs included provincial activities, such as the AMHB, and in years before FY 2003, administrative and overhead costs.
Total RHA expenditures (actual) were obtained from Alberta Health and Wellness annual reports. We note that before FY 2004, mental health expenditures in psychiatric facilities and community mental health centers were not included in RHA budgets, so we had to include them to obtain a consistent measure of the cost of all (actual or potential) regional health services over the entire six years.
We report our results by using two statistics. The first is total current-Canadian dollar expenditures by type of services for each year. The second statistic is the annual ratio of mental health care costs to total health care costs. This is expressed in current dollars, because it measures the proportion of the total annual costs that were incurred in mental health in each year. Doctors' services and outpatient drugs were excluded, because they are derived from a different (provincewide) budget and are not under the control of the regions or AMHB.
The study received approval from the University of Alberta Health Research Ethics Board.
Results
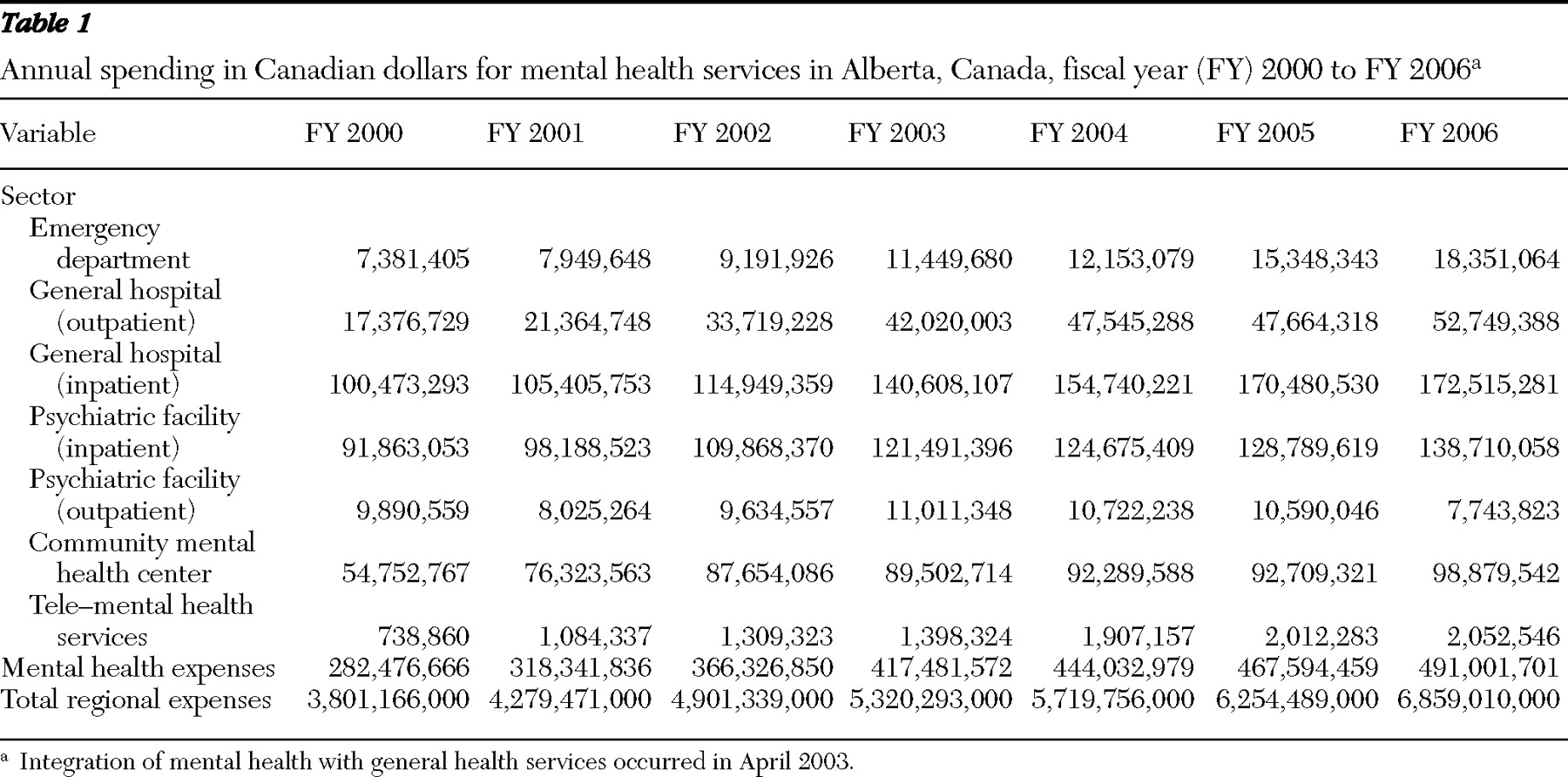
The evolution of RHA and AMHB mental health costs, by category, and in total, is shown in
Table 1 . In total, over the period FY 2000 to FY 2006, mental health care costs increased from $282 million to $491 million. This was an increase of $209 million, or 74%. Total health care costs increased by 80%. From FY 2000 to FY 2003, the period before the transition, mental health care costs increased by 47% and total health care costs increased by 40%. From FY 2003 to FY 2006, mental health care costs increased by 18% and total health care costs increased by 29%.
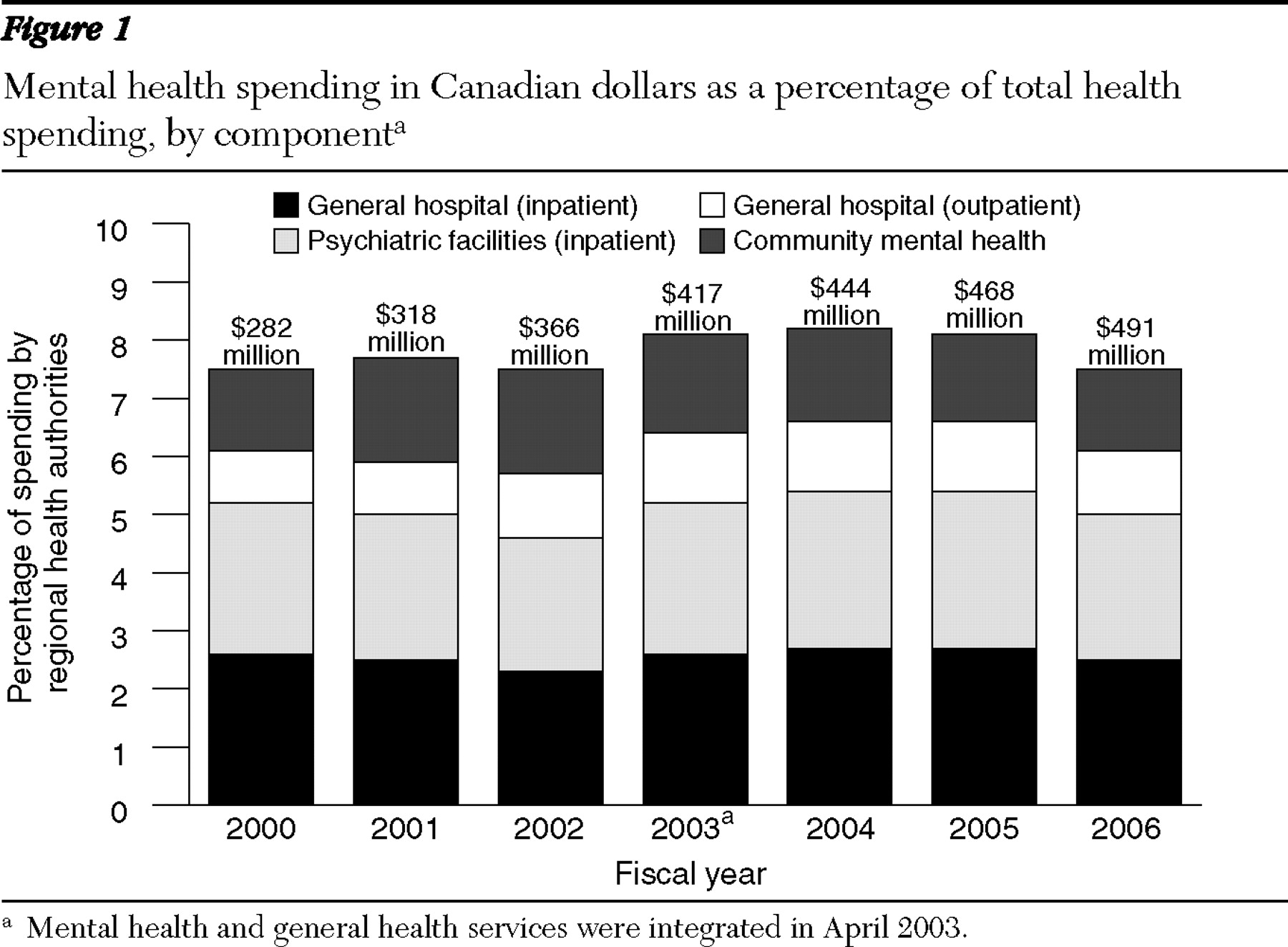
The analysis of mental health share is shown in
Figure 1 . The share between FY 2000 and FY 2003 increased from 7.6% to 8.2% of total health care costs. Following the transition, the mental health share flattened to the pre-FY 2003 levels, to 7.6% by FY 2006. All mental health service expenditures flattened in terms of the share of the total costs. The inpatient cost ratio, both in psychiatric and general hospital facilities, fell by about .1% of total health expenditures after the transition, to the pre-FY 2003 levels. However, the cost ratio in community mental health centers fell by over .2% of the total, also roughly equal to the levels up to 2001–2002.
Discussion
In April of 2003, the beginning of FY 2004, mental health community clinics and psychiatric facilities were transferred to the RHAs in Alberta. Costs for operating these services were paid for out of a single regional budget. The regions themselves (that is, at their discretion) allocated resources for the various service units, and they had to provide for these services within their budgets. We estimated per capita costs for mental health and general health services, and we developed a measure of mental health's share of total spending, which was mental health spending as a percentage of total health spending by the regions, including designated expenses of the AMHB before integration. In the three years after the transfer, the share of mental health spending as a percentage of total health care spending returned to preintegration levels. In a large part, this came about because of the reduced share of community mental health centers, which offset increases elsewhere.
Our study provides a concrete way of measuring the populationwide mental health spending share in a Canadian province. Mental health spending equity has been referred to in government reports as a concept of interest in mental health policy. But it has not been measured. Our measure fits well with this concept, because it can be linked to RHA economic behavior regarding support for mental health. RHAs have discretion to assign costs between mental and general health care.
However, RHAs do not have complete control over their service volumes, especially in the shorter run. Some services can be totally demand generated, and RHAs can only react to this demand. This will be true of emergency visits and nonelective hospital admissions. Some mental health services would fall into these categories. However, for other services, especially community health services, budgets can be adjusted more readily. It is here where the largest reductions occurred.
Our results indicate that the share of mental health in general health spending did not increase when mental health care was taken over by the regions. These results are consistent with the concern expressed by the Canadian government reports cited earlier over the lack of RHA support for mental health care; they provide evidence that support for mental health care has not been increasing relative to non-mental health care spending. The federal government reports (
4,
5 ) both appeared in 2002, and yet an increase in support for mental health care has not been evidenced.
Our estimates are based on unit costs and utilization statistics. Utilization data, especially for hospital services, are based on established data collection instruments, developed by the Canadian Institute for Health Information, and are of very high quality. Data for community visits are less well developed. Inpatient unit cost estimates are based on methods developed using the Management Information System, which has not been fully assessed. There were no major changes in how cost and utilization variables were calculated over this period that would otherwise account for the reduction in mental health services that we observed. In addition, there were no major changes, such as bed closings after the transfer, that would have reduced mental health care costs.
An issue should also be raised about the interpretation of the findings in terms of service units. If the cost-effectiveness of mental health services had increased considerably after transfer, relative to that of general health services, then a relative reduction in mental health spending might still favor mental health care. This is because increased productivity of mental health services would permit relative service levels for mental health to be maintained, even with relative reductions in mental health spending. We could not determine any changes in productivity of mental health services, relative to general health services, over this short period. Relative (between psychiatric and general patients) hospital input costs per day in general hospitals did not change, nor did average lengths of stay. This indicates that relative inpatient mental health cost-effectiveness remained the same. In sum, relative expenditure reductions in mental health care did not reflect reductions in services that were provided to recipients of mental health care.
These results are important to policy makers. Many analysts have expressed concern about the sustainability of current spending levels of general health services because of increased demands resulting from, among other things, the aging populations. This pressure may hold back attempts to address needs for mental health care even more than those for general health care.
Conclusions
The integration of specialized mental health services, formerly organized independently, with the health regions was expected to improve mental health funding in Alberta. The share for mental health care increased overall from FY 2000 (7.6%) to FY 2003 (8.2%), but returned to preintegration levels in the three years after the transfer (7.6%). The integration of mental health services with other health services did not result in an increase of the share of expenditure for mental health care.
Acknowledgments and disclosures
The authors report no competing interests.