Among children with autism spectrum disorders, participation in intensive behavioral intervention for 20 to 40 hours per week can significantly improve their developmental prognosis (
1,
2 ). However, such intervention is prohibitively expensive for most families, costing an estimated $41,295 per year for full-time intervention (
3 ). Public assistance to these families is limited, qualified providers are not widely available, and debate over best practices abounds (
4 ). As of early 2007, Wisconsin was one of four states (also including Colorado, Maryland, and Indiana) with Medicaid home- and community-based services waivers specifically designed to help families pay for intensive behavioral intervention for children with autism (
5 ). Total program expenditures in Wisconsin were $31.8 million in 2001–2002, averaging approximately $30,000 per child (
6 ). Several other states are considering applying for an autism waiver or already have an application under review. Understanding Wisconsin's experience can inform policy makers considering similar measures in other states.
Wisconsin's Medicaid program for intensive intervention underwent a major change on January 1, 2004, when funding was transferred from the state-administered Early and Periodic Screening, Diagnosis, and Treatment program (EPSDT) to a county-managed home- and community-based services waiver. Throughout this period, enrolled families were not necessarily below poverty levels. Most families became eligible via the state's Medicaid TEFRA (Tax Equity and Financial Responsibility Act) plan. TEFRA plans allow states to use Medicaid funds to aid nonpoor families if the child is at high risk of institutionalization and the cost required to provide care within the home is equivalent to or less than institutional alternatives (
7 ).
A proposal in early 2003 to no longer use EPSDT funds for autism intervention was driven by a directive from the federal Centers for Medicare and Medicaid Services (CMS), which stated that the services were habilitative in nature, not rehabilitative as permitted under Medicaid fee for service. The state initially understood the CMS directive to mean that these services could not be covered by Medicaid, and elimination of the funding was proposed in the state budget process. Legislators and administrators were also concerned about rapidly growing program costs and anecdotes of disproportionate utilization by affluent white families even though the prevalence of autism does not vary by race or socioeconomic status (
8 ). Creating a plan that would provide coverage by a Medicaid home- and community-based services waiver emerged as a solution for several reasons. CMS allows reimbursement for habilitative services under a waiver. With its ability to restrict total enrollment, a waiver can more easily contain program costs. Waiver support could be managed at the county level (families applied directly to the state under the EPSDT program), thereby increasing the geographic reach and accessibility to families in underserved communities and, in turn, decreasing demographic disparities.
We examined utilization patterns of Wisconsin's Medicaid benefit for intensive behavioral intervention for children with autism by answering the following question: how did enrollees' demographic characteristics compare with those of all families statewide before and after the transition to the home- and community-based services waiver on January 1, 2004? We analyzed data from three sources: state Medicaid administrative records from 2000–2006, geocoded enrollee demographic characteristics, and decennial census data.
Methods
Medicaid enrollment data for all 1,822 children with autism who received funding for intensive behavioral intervention from January 1, 2000, through November 30, 2006, were obtained from Wisconsin's Department of Health and Family Services. The number of new enrollees per year ranged from 224 in 2006 to 332 in 2003 (mean±SD=260±39). Eighty-one percent of enrollees for 2000–2006 (N=1,469) were male, and the age at enrollment was 5.2±2.2 years (range=2–14). Codes identifying race and ethnicity were missing for 1,177 (65%) enrollees. Family-level socioeconomic status indicators were unavailable.
As an alternative to using individual-level data, we used families' street addresses to geocode demographic characteristics from 2000 census tract-level data. Geocoding allows for linking individual data to area-level demographic indicators, which are highly correlated with individual-level characteristics (
9,
10 ). Area-level demographic indicators are very highly and consistently correlated with individual-level characteristics (
9,
10,
11 ). We examined three tract-level characteristics: the percentage of families with children that had incomes ≥200% of the federal poverty level, the percentage of women 25 and older with at least a high school degree, and the percentage of individuals who were white (in the "white-alone" category of the U.S. census). Thus each individual's value for a given indicator was the corresponding proportion from that person's census tract. For the 635 persons with racial data available in the Medicaid records, the validity of geocoding was supported by comparing the tract-based percentage of white individuals between whites (N= 563, 93%±9%) and nonwhites (N=72, 66%±31%) (t=–15.6, df=633, p<.001).
Means and 95% confidence intervals were computed for the geocoded demographic data of new enrollees from 2000 and 2006. The mean values were compared with population values from the 2000 census for all of Wisconsin by one-sample t tests. Independent-samples t tests were used to compare the mean values from these two enrollee cohorts. Time trends based on mean monthly values from 2000 to 2006 were tested for discontinuities in the prewaiver (2000–2003) and postwaiver (2004–2006) periods with piecewise regression analysis (
12 ).
The study received institutional review board approval at the University of Wisconsin-Madison.
Results
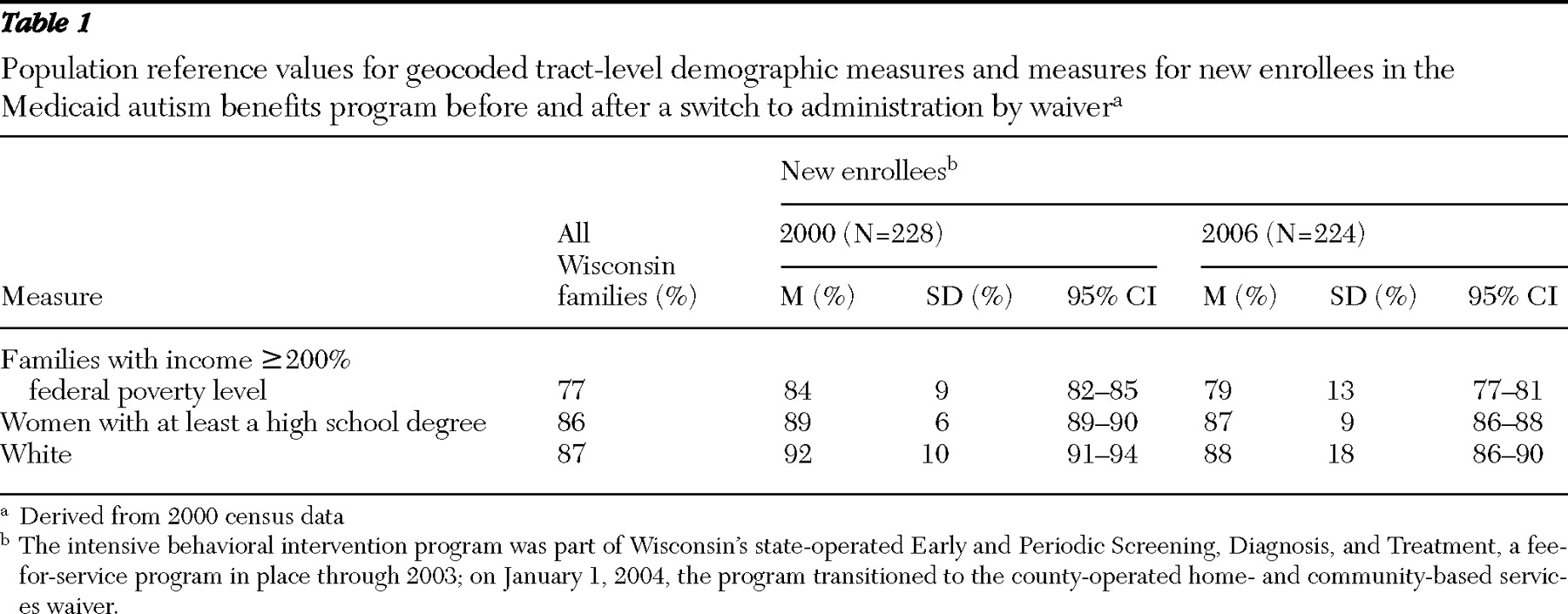
The participants who entered the EPSDT-funded program in 2000 (
Table 1 ) lived in tracts where the proportion of families with incomes ≥200% of the federal poverty level (84%) was significantly higher than the proportion for all Wisconsin families (77%) (t=11.1, df=227, p<.001). The proportion of mothers with a high school or greater level of educational attainment was higher in tracts where participants lived (89%) compared with the proportion for all of Wisconsin (86%) (t=7.8, df=227, p<.001). The proportion of residents who were white was higher in tracts where participants lived (92%) compared with all Wisconsin residents (87%) (t=7.7, df=227, p<.001).
By 2006, two years after the shift to the home- and community-based services waiver, the tract-level proportion of families with income ≥200% of the federal poverty level in tracts where participants lived (79%) had declined by 5% compared with 2000, but the proportion was still significantly higher than the mean proportion for all Wisconsin families (77%) (t=2.6, df=222, p=.009). The 2006 tract-level measures of mothers' educational attainment and proportion of enrollees who were white did not differ significantly from the corresponding overall Wisconsin population values.
There were significant differences between the 2000 EPSDT enrollees and the 2006 waiver enrollees on all three demographic measures. The 2006 waiver enrollees lived in tracts with a lower proportion of families whose mean income was ≥200% of the federal poverty level (t=4.2, df=449, p<.001), a lower proportion of women with a high school or greater level of educational attainment (t=3.8, df=449, p<.001), and a lower proportion of residents who were white (t=3.0, df=449, p=.003).
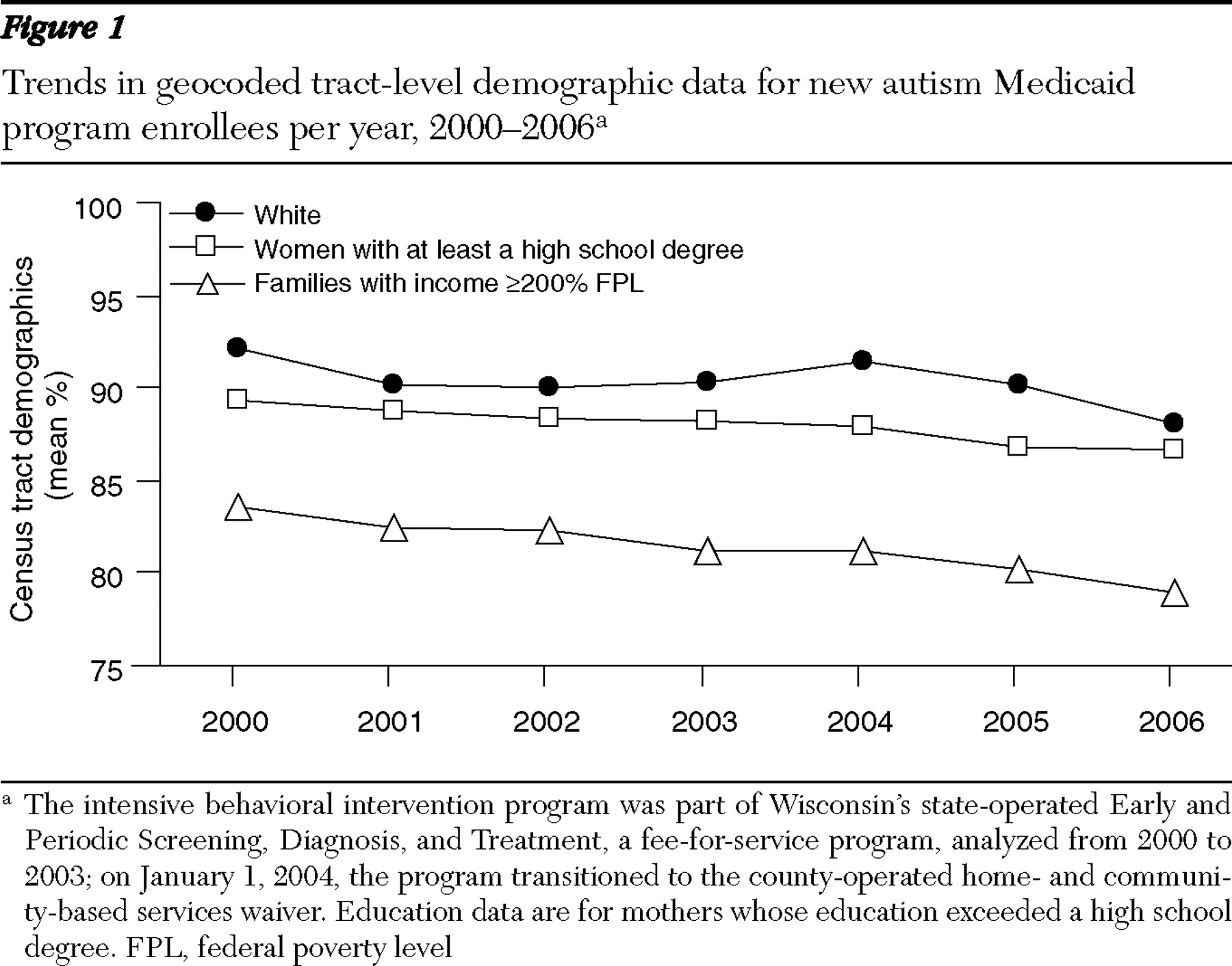
Visual inspection of the trend data (
Figure 1 ) indicates that the percentage of families with incomes ≥200% of the federal poverty level and the percentage with women's education of high school or more declined from 2000 to 2006. Piecewise regression models did not indicate a significant discontinuity in the rate of change before and after the waiver was implemented for these two outcomes. However, the piecewise regression model for the white-only indicator revealed a significant discontinuity, whereby the postwaiver slope was significantly steeper and indicated that more enrollees were from tracts with a lower proportion of whites.
Discussion
Families who entered the EPSDT-funded program in 2000 tended to live in tracts with higher socioeconomic status and a higher proportion of whites compared with Wisconsin families overall. These disparities had decreased significantly by 2006. Although families who entered the program in 2006 were still more likely to live in tracts with a higher percentage of families with incomes ≥200% of the federal poverty level, race and women's educational attainment were no longer significantly different from state averages. There was a preexisting trend toward greater equity concerning federal poverty level and maternal education before implementation of the waiver.
The impact of the new home- and community-based services waiver on disparities appears mixed. On the one hand, trends toward greater equity in income compared with the federal poverty level and maternal education measures before 2004 continued after implementation of the waiver. Implementation might have accelerated the trend for women's education status, but supporting data were inconclusive. In contrast, waiver implementation was followed by accelerated program enrollment among families living in tracts with higher proportions of nonwhites, indicating a lessening of racial disparity.
It is not possible to attribute these changes definitively to waiver implementation. Contextual factors that could have influenced these trends include the political controversy surrounding the proposed elimination of autism funding and negotiations to preserve funding. It is possible that news coverage increased awareness of the program and stimulated demand from a more representative cross-section of the population independently of the waiver program.
Program differences may have influenced these trends as well. The funding for autism services under EPSDT was administered by the state's central Medicaid office. During this era, families had to educate themselves about the program and navigate their way through the application and eligibility process without professional case management. In contrast, the waiver is administered through county human services agencies and includes mandatory case management. The approach used with waiver implementation therefore penetrates underserved geographic areas and assists families who may be less capable of navigating complex eligibility procedures on their own because of socioeconomic disadvantage. Future research should examine whether different methods of outreach are needed to reach other underserved demographic subpopulations.
Limitations of this study include reliance on administrative data and geocoded values as proxy measures of demographic characteristics. However, Wisconsin's financial support for autism intervention and the ability to examine disparities before and after policy change make this study uniquely relevant for state policy makers considering similar programs elsewhere.
Conclusions
Autism program utilization in Wisconsin has become more equitable over time. Some of the increased equity came from continuation of a trend that preceded changes in program funding and organization, which might reflect a tendency for new services to become more equitably utilized over time. The switch to a home- and community-based services waiver was associated with an increase in racial equity, although a causal relationship is impossible to determine with these data. Other states considering carve-out programs for autistic children should carefully evaluate whether the administrative structure will promote equitable utilization and prospectively incorporate evaluation into program rollout.
Acknowledgments and disclosures
This study was made possible by a grant from a cooperative agreement between the Centers for Disease Control and Prevention (CDC) and the Association of University Centers on Disabilities. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC. The authors give special thanks to Marshalyn Yeargin-Allsopp and Laura Schieve of the CDC's National Center on Birth Defects and Developmental Disabilities for their constructive comments.
The authors report no competing interests.