There is no health without mental health. This simple yet profound statement is at the heart of transformation not only of the mental health system in the United States but of health care itself. At a time when the new Administration is seeking pragmatic and progressive solutions to health care reform, the Center for Mental Health Services (CMHS), part of the Substance Abuse and Mental Health Services Administration (SAMHSA) in the U.S. Department of Health and Human Services (DHHS), has both the opportunity and the responsibility to play a leading role in health care policy, financing, and services. We are in the business of building resilience and facilitating recovery for all Americans. The time to do so is now.
External events are shaping discussions about mental health services and health reform. Passage in October 2008 of mental health parity legislation has ushered in a new era of opportunity for the integration of mental health care and general medical care. The current economic downturn places stress on individuals, provider systems, and states and communities. And a number of groups have called for an increased focus on public health and prevention to promote the well-being of individuals, families, and communities and to strengthen U.S. competitiveness and national security.
CMHS is well positioned to implement a public health approach to mental health. Several major reports—including those by the Surgeon General, Institute of Medicine, and the President's New Freedom Commission on Mental Health—have called for fundamental transformation of the nation's mental health system. In response, CMHS has led the effort to advance a recovery-oriented, person-centered approach to mental health recovery and state mental health systems transformation. This effort anticipates the development of a defined strategy for mental health care for the nation as a whole.
Together with mental health care consumers and family members and key stakeholders at the federal, state, national, and local levels, CMHS has initiated dialogue and begun to implement change in a number of critical areas. Most notably, CMHS has helped develop programs and services that are person centered, recovery focused, evidence based, quality driven, and outcomes oriented.
In the coming years, the sense of what it means to improve the nation's health will continue to evolve. Increasingly, the focus will move from illness to health. New practice models will integrate mental health with general health care. Electronic medical records will improve efficiency and reduce medical errors, and personal health records will put tools for recovery and wellness in the hands of consumers. CMHS is ready to help guide these changes.
To help us do so, I asked staff, consultants, and key stakeholders to reflect with me on the progress CMHS has made vis-à-vis mental health transformation over the past five years and the challenges and opportunities it faces in the next five years. We conducted a comprehensive literature review and formal constituent input process. The result is a strategic forecast to guide the center's work in formulating policy and directing resources. We are in the process of finalizing the forecast, which will serve as the basis for more formal strategic action.
Information gathering
Clearly, no assessment of how the mental health field has evolved in recent years would be complete without a review of the key documents that have both influenced and reflected change.
Mental Health: A Report of the Surgeon General (
1 ) established the historic and scientific base for the existence and treatment of mental health conditions.
Achieving the Promise: Transforming Mental Health Care in America (
2 ) and the subsequent Federal Action Agenda (
3 ) specified the need for a consumer- and family-driven system of mental health care that embraces recovery.
Improving the Quality of Health Care for Mental and Substance-Use Conditions (
4 ), part of the Institute of Medicine's Quality Chasm Series, outlined the evidence base for quality mental health care and the need for services to be person centered and coordinated across all systems of care.
These seminal reports provided a platform for more recent analyses about the ways in which changing market forces—including the predominance of Medicaid as a funder of public mental health services—have affected public and political discourse about mental health and mental illnesses in this country (
5,
6 ). Together with scientific findings that reveal significant disparities in health and health care delivery for people with serious mental illnesses, these policy documents point toward a future in which mental health is regarded as essential for overall health.
Findings in the scientific literature were corroborated and amplified by the voices of individuals who make policy, provide services, and have experienced mental illnesses and recovery. CMHS consulted its staff, key constituents, and leading experts in the field, including members of the CMHS National Advisory Council and its Subcommittee on Consumer/Survivor Issues. Respondents were asked to examine CMHS accomplishments vis-à-vis mental health transformation and suggest areas for future investment. They made it very clear that the time for study and reflection are over; now is the time for concerted, focused, and deliberate action.
In particular, these individuals made some important observations. Many respondents pointed out that mental health care and general medical care services need to be better coordinated and integrated. There was a great deal of discussion about recovery from mental illnesses and the tools and resources needed to promote it. Respondents encouraged CMHS to build on its recovery focus and develop tools and financial incentives to support the development of recovery-oriented systems of care. Most respondents raised concerns about future funding for public mental health systems. Financing issues include both the allocation of resources and the scope of coverage. Some respondents expressed the need for a defined national mental health policy that reflects and guides the U.S. global position on mental health and mental illness. Respondents also expressed concern about the size, quality, and aging of the mental health workforce. Some respondents stressed the fact that data can be a powerful tool in quality improvement, and outcomes need to be standardized to promote their use. They also noted opportunities for expanded use of technology in data collection, as well as in support of direct services, health promotion, and wellness. Finally, most respondents believe that transformation of the mental health system will continue to evolve in the coming years.
On the basis of our literature review and key informant input, we developed a framework for our strategic forecast that includes a vision, values, priorities, and strategies, coupled with basic core functions. Taken together, these key elements assisted us in creating a template that both guides our work and serves as a pulse check on our progress.
Vision, values, and priorities
The CMHS vision is grounded in and inclusive of the SAMHSA vision of "a life in the community for everyone." We advance our vision as both a signpost of where the nation must head and a benchmark for the use of CMHS resources.
CMHS envisions a nation in which mental health is regarded as essential for overall health and in which all individuals have access to the community opportunities and health and social supports that will help them excel in a complex and competitive society. To achieve this vision of a preferred future, our work must be grounded in a set of values that guide the programs CMHS supports, the services that these programs provide, and the infrastructures that support them. In our preferred future:
• Recovery is the expected outcome. All mental health services and supports are driven by the primary goal of recovery, and all providers acknowledge and offer the hope of recovery. Consumer-operated services and programs are implemented as an evidence-based approach to promote recovery.
• Service recipients direct their own care. Consumers of mental health services have full access to and make informed use of effective services and tools that allow them to take charge of their recovery and their lives.
• Services are evidence based. Routine mental health care is grounded in evidence-based practice and practice-based evidence and is coordinated across all medical and social systems of care.
• Performance management drives quality improvement. Process and outcome measures support evolving cycles of change, and performance goals are tied to specific outcomes.
These values form the basis for and are embedded in our key priorities. In the next few years, every service, program, or activity we support must adhere to, advance, and promote the following five priorities.
First and foremost, CMHS will embrace the concept and practice of a public health model of health care. The public health model is a community approach to preventing and treating illnesses and promoting well-being. It addresses treatment for individuals across the lifespan while developing interventions for the entire population. As steward of the nation's mental health, together with our SAMHSA partners in substance abuse treatment and prevention, CMHS informs and educates individuals about mental health and well-being; develops policies and mobilizes public-private partnerships that support individual and community health efforts; ensures a competent workforce; and evaluates the effectiveness, accessibility, and quality of our services, programs, and activities. Each of these is considered an essential public health service, and all are reflected in our principal strategies, highlighted below.
Second, we will use the tools of public health to advance holistic, person-centered health care. A holistic approach is grounded in the knowledge that health is a function of the complex interplay between body, mind, spirit, and community. Person-centered care is respectful and responsive to the needs and values of individuals and honors and supports recovery and wellness. All of our programs, services, and activities must meet this standard.
Third, we know that in the spirit of public health, which considers both the health of individuals and the health of the community, we must attend to the broad determinants of health. These include the personal, social, economic, and environmental factors that influence health, well-being, and wellness. For people with mental illnesses this means focusing on such issues as poverty; widespread unemployment; inequitable distribution of health care resources; and the discrimination, fear, and bias that keep people with mental health problems at the margins of society. Without access to housing, health care, employment, and social support, individuals are excluded from all that it means to be healthy in today's society.
Fourth, the public health approach demands that prevention, early intervention, and treatment services be delivered by a customer-focused workforce. Practicing in a 21st century health care environment demands a competent, capable, sustainable, and culturally diverse workforce. Members of this workforce—including mental health consumers—must be recruited, educated, trained, and supported to practice whole-health, person-centered health care.
Finally, health care that is inclusive of individual, community, and social factors must demonstrate its value as measured by both short- and long-term outcomes—hence our focus on continuous quality improvement. Evaluating the effectiveness, accessibility, and quality of personal and population-based health services is a key tenet of the public health approach. We must assess not only the programs, services, and activities we support but also the way in which our decisions are made.
Principal strategies
Creating whole-health, person-centered health care, achieved through a public health approach that addresses the broad determinants of health, demands attention to strategic change in several important spheres of influence. CMHS is well positioned and prepared to address the following three key areas, with specific actions and policies.
Building the information base
Information is the foundation on which a public health approach is built. Four specific actions are included in this area. First, CMHS will review, disseminate, and provide technical assistance on effective mental health promotion and mental illness prevention strategies. Promoting mental health and preventing mental illnesses are the essence of a public health approach to health care. The concepts of mental health promotion and mental illness prevention rest on the knowledge that mental health exists on a continuum, with neither health nor illness existing in pure isolation from one another. The recently released Institute of Medicine report on prevention, supported by SAMHSA, has some exciting findings about our ability to promote mental health and prevent mental health problems, particularly among our nation's youth (
7 ). CMHS can promote these strategies to preclude the onset of mental disorders, lessen their impact, and forestall comorbid conditions and long-term disability.
Second, CMHS will help develop, disseminate, and measure the broad determinants of mental health. Without action to address the broader social, economic, political, and environmental factors that have an impact on health and well-being, both individual and community health suffer. This is evidenced by the fact that individuals with serious mental illnesses die, on average, 25 years earlier than the general population. They die from treatable medical conditions that are caused by modifiable risk factors, including smoking, obesity, substance abuse, and inadequate access to medical care (
8 ). CMHS can ensure that such disparities will be addressed.
Third, CMHS will promote the dissemination of evidence-based practice and practice-based evidence. In its broadest sense, inequality in health care is driven by social, economic, and political factors. Inequality also results, particularly in mental health treatment, when providers rely on outdated science rather than on the best available evidence-based interventions. Many communities lack the financial or technological resources required to keep abreast of the latest developments in science and service. To address these gaps, CMHS can ensure that resources for the development and use of evidence-based practice and practice-based evidence are made available to those who need this help the most.
Fourth, CMHS will harness communications technology to promote involvement in treatment, services, and policy. Informing, educating, and empowering people about health issues are considered essential public health services. Electronic communication can promote health literacy, disseminate public health messages, support healthy behaviors, and create virtual learning communities. Internet-based and other interactive tools, including social networking, put information and decision-making technology that supports recovery directly into the hands of consumers. CMHS can use these powerful tools to foster peer support, convene national policy discussions, and promote online learning about person-centered care and recovery.
Providing national mental health policy leadership
Information is ineffective without policies that support its use. Two specific actions are included in this area. First, CMHS will emphasize and coordinate the role of mental health in evolving health reform, including the development of a national mental health policy. Public health is a population-based approach that supports the development of whole-health, person-centered health care. This requires that the mental health community be intimately involved in any and all discussions of health care policy at the federal, state, and local levels. As a leading voice for mental health promotion, mental illness prevention, recovery, and treatment, CMHS can lead discussions with key stakeholders about evolving health policy and the role for mental health.
Second, CMHS will cultivate leaders in the public and private sector who are informed about all aspects of mental health financing. As several observers have noted, financing policies were the principal driver of system change in mental health in the latter half of the 20th century. Medicaid policy in many ways is synonymous with mental health policy; managed care also shapes the delivery of mental health services. In addition, passage of mental health parity will have an impact on employer-sponsored health insurance coverage and, by extension, on private and public systems of care. CMHS can help create shared objectives for public and private payers for mental health services to promote whole-health, person-centered health care.
Providing leadership to the field
Finally, information and policy are two components of our approach to public health. The third is field leadership. Four specific actions are included in this area. First, CMHS will help states and communities adopt whole-health, person-centered health care. Many states and communities have made great strides in this area, but others lag behind. By definition, all sectors that have an impact on the lives of people with mental health problems must be involved and invested in transforming mental health services. These sectors include, but are not limited to, health care, housing, transportation, employment, education, social services, services for veterans, criminal and juvenile justice, and child welfare. CMHS can play a leading role in promoting and supporting the level of collaboration required to have an impact on the financing, delivery, and evaluation of mental health and general health care services.
Second, CMHS will help educate, train, and support a 21st century health care workforce. Mental health and general medical treatment and services are only as good as the workforce that delivers care. The practice of mental health care and general medical care must include assessment of the full range of health-related issues, treatment planning that takes each of these factors into account, and support for the whole person. Such services must be offered in both mental health and general medical settings by practitioners and providers who can practice in a culturally diverse, multidisciplinary, high-tech health care environment. CMHS can play a leadership role in educating, training, and supporting the modern health care workforce.
Third, CMHS will help empower and mobilize the individuals who will lead the mental health and general health care fields. Significant change in accepted practice—represented by the adoption of whole-health, person-centered health care—requires transformational leaders. Consumers and family members who have experiences with mental illnesses must be empowered and mobilized to shape, inform, and provide leadership to the mental health care and general medical care fields. Likewise, practitioners and providers must become leaders capable of engaging with consumers and family members and of embracing the technological tools and resources that support a public health approach. CMHS will continue to define key leadership skills and provide the training and technical assistance to advance them.
Fourth, CMHS will develop a performance management culture that uses data to make financing and programmatic decisions. Programs that use public funds to provide health care services must be held accountable for producing results. CMHS uses a variety of tools to collect and report process and performance data on its services, programs, and activities. These data must become the centerpiece of performance management tools and processes that provide timely, relevant, and actionable information. Performance improvement activities based on the judicious use of data will ensure that all CMHS-funded services, programs, and activities promote person-centered, recovery-focused, evidence-based, quality-driven, and outcome-oriented health care.
CMHS core functions
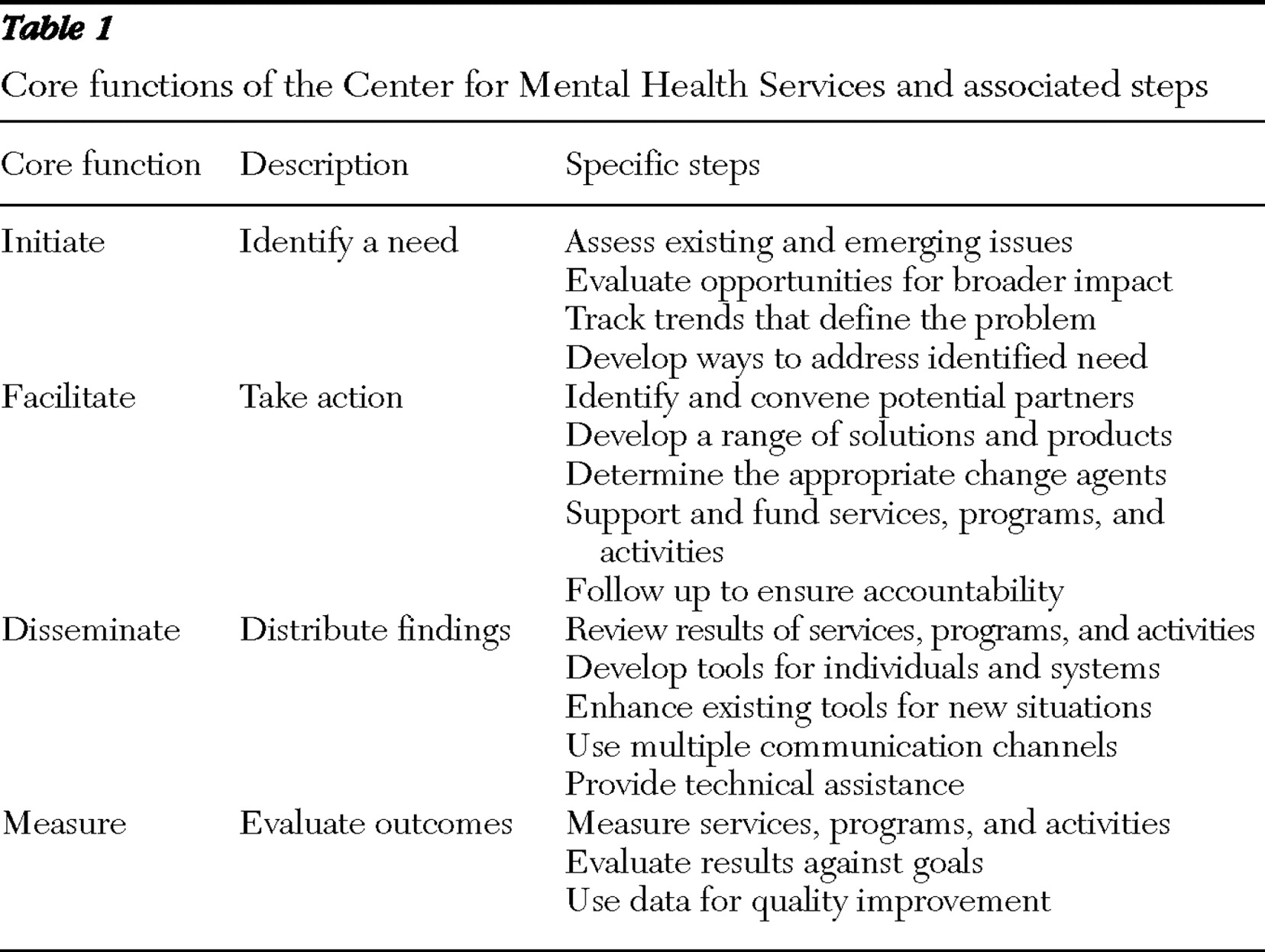
Each of the strategies enumerated above can be realized by using a set of public health tools and processes that CMHS calls its "core functions." These core functions reflect the center's legislative and congressional mandates and provide a standard by which any potential service, program, or activity can be judged and implemented.
Most resources under CMHS stewardship are responsive to congressionally mandated programs. These include the Mental Health Block Grant, Children's Mental Health Initiative, Protection and Advocacy for Individuals With Mental Illness, and Projects for Assistance in Transition From Homelessness. A set of discretionary activities, called Programs of Regional and National Significance, focuses on new and emerging priorities. These include such areas as reducing and eliminating the use of seclusion and restraint, developing trauma-informed services and systems, and addressing the overrepresentation of individuals with mental illnesses in the criminal justice system.
To ensure that both its congressionally mandated and discretionary programs are designed to create and sustain a public health model, CMHS uses the tools highlighted in
Table 1 . Each of these tools or core functions is one element in an overarching framework for change that ensures accountability, transparency, and alignment with available resources. Taken together, they are part of an iterative and continuous process that provides a framework for current and future action.
Next steps
The development of this strategic forecast is not the end point in a process of change; instead, it is a critical step toward achieving the vision of a preferred future. The task going forward is to ensure that every current and planned service, program, and activity is grounded in the values and emerging priorities of DHHS and SAMHSA and implemented according to the core public health functions. In order for a strategic forecast to have lasting value, there must also be an ongoing process of review, measurement and accountability, and process improvement. As we finalize our work on the strategic forecast, we will create a formal vehicle for performance management to ensure that our work is person centered, recovery focused, evidence based, and quality driven. The individuals we serve deserve nothing less.
Acknowledgments and disclosures
The author reports no competing interests.