Attribution theory suggests that beliefs about the causes of mental disorders have an influence on stigmatizing attitudes and behaviors toward persons with mental illness. Findings from attribution theory-informed studies have implications for antistigmatization efforts, in which education about causation is typically a central strategy for reducing negative attitudes toward people with mental disorders (
1,
2,
3,
4,
5,
6 ).
Research on causation is informed by a central tenet of attribution theory suggesting that a person with a mental disorder will be perceived relatively more favorably when the cause of the disorder is seen as outside of the individual's control (such as a biological, genetic, or environmental cause) and, conversely, that such a person will be perceived more negatively if he or she is seen as somehow causing the condition through a lack of willpower or effort or some other moral failing (
7,
8,
9,
10 ). Although predictions derived from attribution theory are supported for the most part, findings regarding attribution to genetic or biological causes are mixed. In some studies, attribution to biological or genetic causes was associated with less negative perceptions (
8,
11 ), but in others, genetic or biological causal attributions were associated with more negative perceptions (
10,
12,
13,
14 ), perhaps because behavior arising from these factors is likely to be perceived as serious, persistent, or difficult to control (
9,
10,
12,
13,
14,
15 ).
Research on beliefs about the causes of mental disorders documents variation across cultures (
10,
16,
17 ) and between cultural groups within Western societies (
16,
18,
19,
20,
21 ). Antistigmatization efforts that include a focus on causal attributions may thus require sensitivity to subpopulation differences in beliefs about causation.
Although there is a small body of literature about exploring causal attributions among people who have mental illnesses (
22,
23,
24 ), there appears to be only one study that compared these attributions with those of the general public (
23 ). In that study, people with mental illness were much more likely than the general public to make negative causal attributions, for example, seeing their condition caused by their "own bad character" (
25 ).
Comparatively little research has examined causal beliefs among children and adolescents. Existing studies are typically small, and few have explored differences by sex or by race and ethnicity, even though these variables have proven significant in studies that focused generally on children's perceptions of peers with emotional or behavioral difficulties (
5,
26,
27,
28 ). This limited body of research indicates that children generally endorse the same types of causes of mental illness or emotional and behavioral disorders as adults, including genetic or biological causes and stress or trauma (
5,
29,
30,
31 ). Available evidence also suggests that, like adults, children tend to have more negative views of peers whom they see as responsible for their problematic behavior (
29,
32,
33,
34,
35 ) and more positive views of peers whose difficulties are caused by life stress (
36 ).
In the study reported here, we used data from the first national study of children's attitudes toward peers with mental health problems to examine beliefs about causation. Earlier analyses of data from the same source examined stigmatization generally and found marked stigmatization of depression and attention-deficit hyperactivity disorder (ADHD) compared with asthma, with depression generally more stigmatized than ADHD (
28 ). The level of stigmatization was relatively consistent across most demographic variables. This study built on these earlier analyses in examining young people's beliefs about the causes of depression and ADHD, the most commonly diagnosed emotional and behavioral disorders among children (
37,
38 ). Seven well-studied and theoretically meaningful causes were identified from the literature and used in this study: parenting, substance abuse, lack of effort, genetics, brain differences, God's will, and stress.
Although this study was informed by attribution theory and related research, the limitations of the existing literature made the formulation of specific hypotheses difficult. As a result, an exploratory approach was used to address the primary research question: what are the factors associated with endorsement of the various causal beliefs? The independent variables tested were condition (ADHD and depression), age, sex, race and ethnicity, and whether the respondent reported having received a diagnosis of the target condition.
To help clarify the meaning of the primary analyses, we explored two preliminary research questions. First, as evidence of the relative stigmatization of the causal attributions, what is the correlation of each of the seven causation items to social distance, the most widely used stigmatization construct (
39,
40,
41,
42 )? Second, what is the interrelationship of the causation items?
Methods
The survey was administered online in 2006 by the polling firm Harris Interactive, which maintains a panel of more than six million members who have agreed to participate in its surveys. Harris Interactive is a member organization of the Council of American Survey Research Organizations and thus adheres to its code of ethics (
43 ), which prescribes specific protections for survey respondents. Procedures include written informed parental consent and child consent or assent. The institutional review board at Portland State University certified that the study met the criteria for a secondary analysis and provided a waiver of review.
Children of adult panel members were recruited into the panel with parental permission and ranged in age from eight to 12. Youth panel members aged 13 and over were either recruited in a similar manner or else directly, via e-mail. Randomly selected youth panel members were invited by e-mail to participate in the survey. For children under 13, an informational e-mail was first sent to the parent panel member, who then allowed the child to participate. Responses were gathered until U.S. Census-based demographic targets were approximated. The data were then weighted for age and sex to bring them in line with their proportions in the general population. Weighted samples from the Harris Interactive panels have provided data that are comparable with data from random samples of general populations (
44,
45 ).
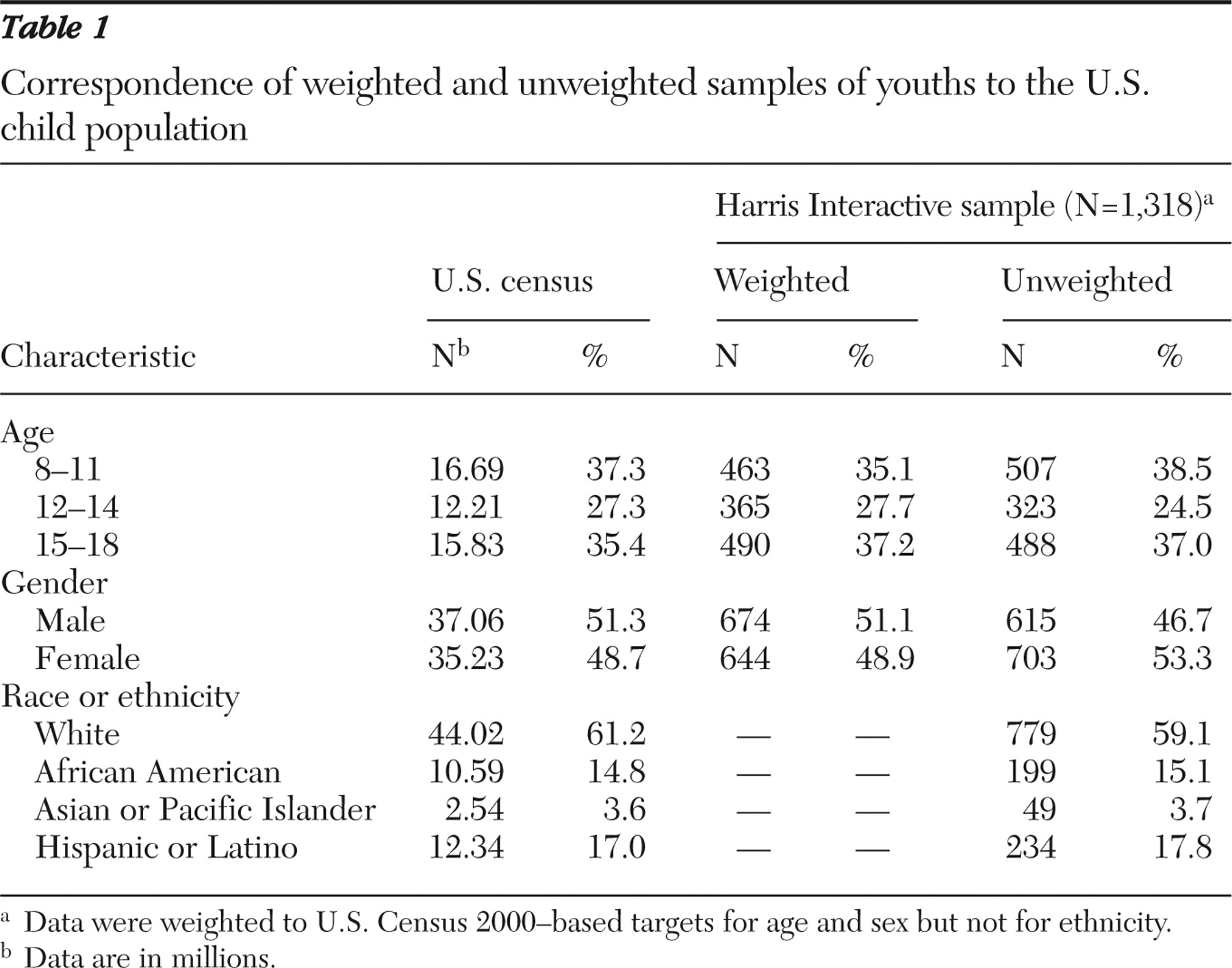
Table 1 shows the correspondence of the weighted and unweighted sample of 1,318 children and adolescents to the U.S. child population. Because of the cognitive complexity of the items, the eight- and nine-year-olds were not asked about causation; the analysis therefore used the data from 1,091 respondents aged ten and older.
Survey respondents were randomly assigned to one of three survey versions, each with a focus on depression, ADHD, or asthma. The first two conditions were chosen because of the likelihood that children and adolescents between ages eight and 18 would have had contact with peers who had these emotional and behavioral conditions. Asthma, a physical illness, was used as a comparison condition.
The study survey was developed collaboratively by children's mental health researchers, staff from Harris Interactive, and young people with emotional and behavioral disorders. The first section of the survey includes a brief vignette about Michael, a young person who has the target condition. Respondents are asked to imagine that Michael is a student in their class and that, because of this condition, Michael sees a doctor, has been in the hospital several times, and spends part of the school day in special classes or activities. Respondents then answer a series of questions about Michael, including questions about what might be causing Michael's condition and about peer preferences for social distance from Michael.
Measures
Causal beliefs were assessed with seven items parallel to those used in studies of adults (
8,
40,
46 ). Respondents were also asked whether a psychologist or physician had ever given them a diagnosis of the target condition.
This study used an adapted version of the Social Distance Scale (SDS), which asks respondents to rate their willingness to interact with people with mental illness in different situations. The published reliability of the SDS ranges from .75 to .92 (
39 ). For this study, the SDS was adapted to reflect situations more typical of childhood; for example, the item asking about willingness to "work with" a person was changed to "work on a school project with." The adapted five-item scale had very good reliability (
α =.89).
Based on theoretical considerations and examination of the distributions of the items, Likert scale items were dichotomized by collapsing responses that indicated agreement (for example, maybe and yes responses were recoded as 1, and no was recoded as 0). The nondichotomized variables were used for the computation of correlations.
Analysis
Correlations were computed between social distance and the seven causation items. Scaling of causation items was explored, but no parsimonious scale summary of the seven causation items was found, so the individual items were used in further analyses. Hierarchical logistic regression models were constructed for each causation item, with main effects entered in step 1 and interaction terms in step 2. Age, sex, race or ethnicity, target condition, and diagnosis were entered simultaneously in step 1. To arrive at a parsimonious final model, step 2 used backward removal to test 15 theoretically selected terms: the interaction of condition (depression or ADHD) with each demographic variable and with diagnosis and the interaction of race or ethnicity and gender.
Results
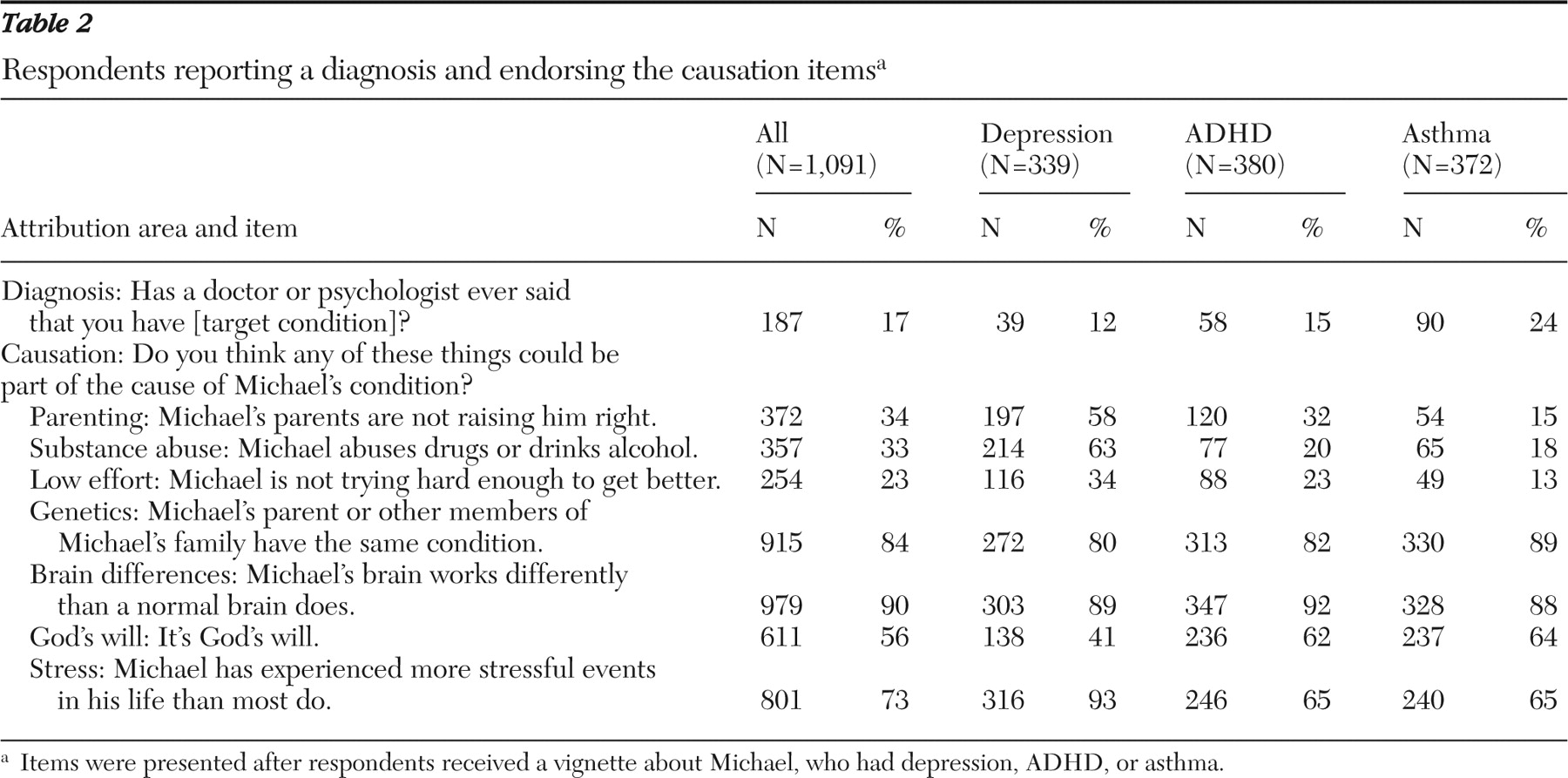
Table 2 shows the percentages of respondents in each condition who endorsed the causation items and reported having received a diagnosis of that condition. Tests of significance are not reported for these bivariate relationships because the relationships were tested later in the multivariate logistic analysis. Within each of the three conditions, participants were asked if they had ever received a diagnosis of that condition. More children reported diagnoses of ADHD than depression. Three causation items (parenting, substance abuse, and low effort) were endorsed by markedly higher proportions of children given the depression vignette (compared with ADHD or asthma conditions). These items were also rated higher by those in the ADHD condition than those in the asthma condition. Genetics and brain differences were consistently endorsed by 80% to 90% of respondents across conditions. Stress was endorsed at high rates across conditions, with a very high proportion in the depression condition. Just over half of the participants (56%) thought it likely that Michael's condition was due to God's will, with a lower proportion (41%) in the depression condition endorsing that cause.
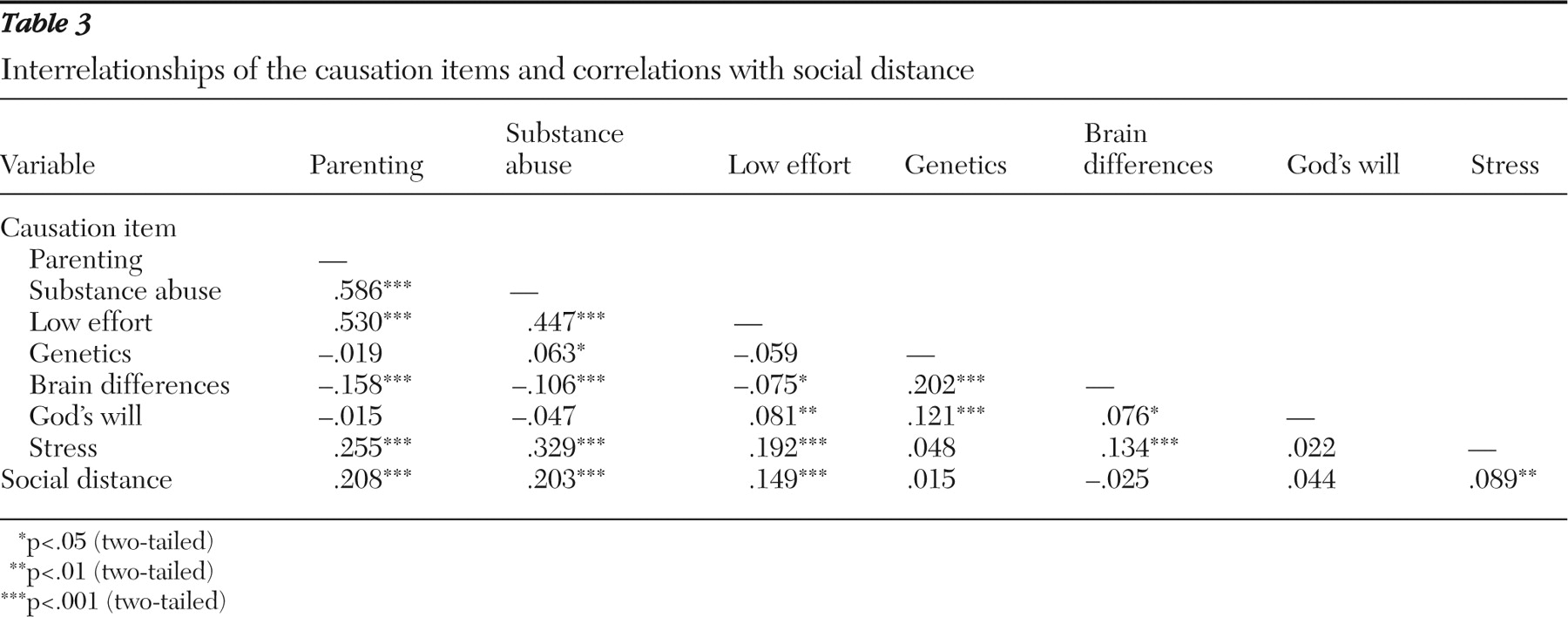
Table 3 shows the correlations between the causation items and between the causation items and social distance. There was a convergence of strong correlations among parenting, substance abuse, and low effort. In addition, stress had small to medium correlations with those three items. More modest convergence was found for genetics and brain differences, with a small to medium correlation. Small correlations were observed between God's will and genetics and God's will and low effort.
Three items—genetics, brain differences, and God's will—had no association with social distance. Using Cohen's (
47 ) guidelines for interpreting correlation coefficients, we found that three causation items had small to medium correlations with social distance: parenting, substance abuse, and low effort. A small correlation was observed between social distance and stress.
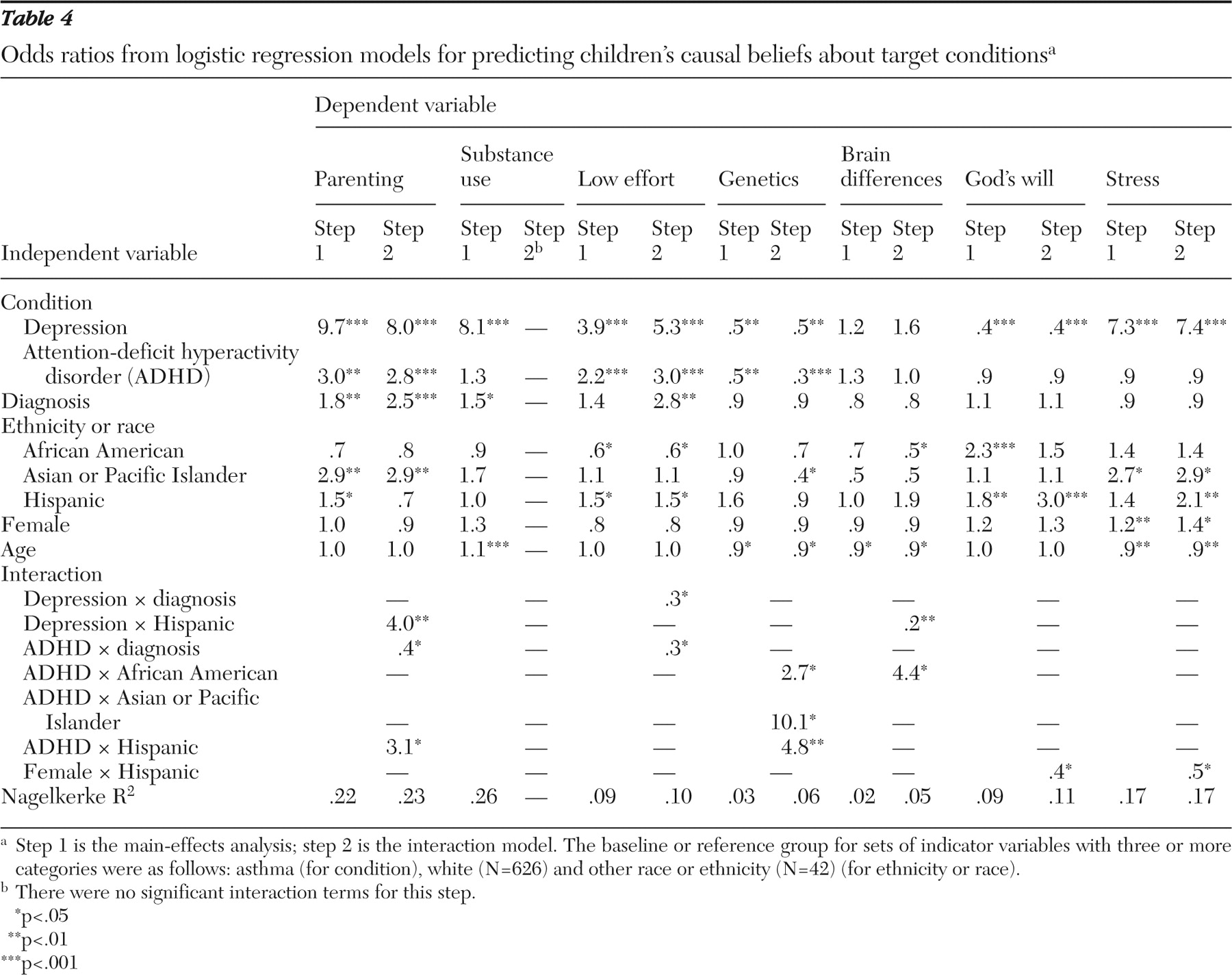
Table 4 shows the logistic regression results for each causation item as a dependent variable (step 1 is the main-effects analysis; step 2 is the interaction model). All of the models were significant at p<.001, except the main-effects models for brain differences (not significant) and genetics (p<.01). The Nagelkerke approximation of R
2 underestimates the multiple associations of the independent variables to the dependent variable (
48 ). Therefore, the R
2 approximation should be viewed as a very conservative estimate of the effect size for the model. Nagelkerke R
2 values ranged from small to moderate.
The strongest main effect for six of the models was the depression condition. Asthma was the comparison condition. The size of these effects ranged from very large—nearly ten times more likely to endorse parenting as a cause of depression—to small to medium—half as likely to endorse genetics (effect size interpretations according to Rosenthal's [
49 ] guidelines for odds ratios). In addition to the very large effect of parenting, large effects were found for respondents who were given the depression vignette, who were more likely to endorse substance abuse, low effort, and stress as causes. Effects for the ADHD vignette were smaller and present in fewer models. Participants in the ADHD condition were more likely to endorse parenting and low effort and less likely to endorse genetics.
Those who reported a diagnosis of depression or ADHD were more likely to attribute the condition to parenting and substance abuse (small to medium effects). In the parenting interaction model, those who reported a diagnosis of depression or asthma were 2.5 times more likely to endorse parenting, but this effect did not hold true for children diagnosed as having ADHD. A similar pattern of main and interactive effects was found in the low-effort interaction model.
For race or ethnicity, the comparison group consisted of white youths and youths of other racial or ethnic backgrounds. Asian or Pacific Islanders were nearly three times more likely than youths in the comparison group to endorse parenting and stress as causes (small to medium effects). Hispanic youths were 1.5 times more likely to endorse parenting and low effort. African-American respondents were approximately half as likely as the comparison group to endorse low effort. In the interaction term model, youths who were Asian or Pacific Islanders were 2.5 times more likely to endorse genetics across conditions, with a very strong effect (ten times more likely) to endorse genetics as a cause of ADHD.
As causes of depression, Hispanic children were four times more likely than the comparison group to endorse parenting and five times less likely to endorse brain differences. Hispanic children were also three times more likely than the comparison group to endorse parenting and nearly five times more likely to endorse genetics as causes of ADHD. A main effect for Hispanic youths to be twice as likely to endorse stress as a cause did not hold true for Hispanic girls (Hispanic × female interaction term indicated that endorsement was half as likely).
Girls were more likely to endorse stress, the one significant effect of gender. Age of participants was associated with increased likelihood to attribute Michael's condition to substance abuse (10% increase per year older). The probability decreased 10% for each year older for endorsing genetics, brain differences, and stress as a cause.
Respondents were 2.5 times less likely to attribute depression to God's will, and African-American and Hispanic children were roughly twice as likely as the comparison group to endorse God's will (medium effect sizes). In the interaction model, Hispanic children overall were three times more likely to endorse God's will, but this effect was almost entirely attenuated for Hispanic girls (2.5 times less likely).
Discussion
The beliefs about the causes of depression and ADHD were associated with varying levels of stigmatization. We used the face-valid meaning of items, correlations with social distance, and intercorrelation of the causal beliefs to interpret the degree of stigmatization inherent in each causal belief. The item on low effort had high face validity as a stigmatizing causal belief. One-third to one-quarter of the respondents agreed that not trying hard enough to get better was a cause of Michael's depression or ADHD. Thus, for a child with depression or ADHD, at least one in four peers believes the child is to blame for the condition.
There was further evidence of stigmatization in the small to medium correlations of parenting and substance abuse with social distance, and both had strong correlations with low effort. The stigmatizing meaning of low effort, parenting, and substance abuse converged with similar research for adults (
8 ). The strong intercorrelation of these three items reflects an underlying construct of an individualistic, moralistic, and blaming view of the causation of mental health difficulties. This result is consistent with previous attribution theory-based research that found blaming and moralistic attributions associated with higher stigmatization (
7,
8,
9,
10 ).
Endorsements of the three items—low effort, parenting, and substance abuse—were four to 9.7 times more likely in depression than in the asthma condition. More modest effects were found for ADHD. In a separate analysis of this data set, the same three-step pattern of stigmatization, depression more stigmatized than ADHD and ADHD more stigmatized than asthma, was found by Walker and colleagues (
28 ) in negative and positive attributes, social distance, and family attitudes.
Studies of adults have found mixed evidence of stigmatization for beliefs centering on biological or genetic causes (
8,
10,
13,
14,
15 ). In our study, brain differences and genetics were not associated with social distance. However, brain differences had small negative associations with the moralistic and blaming causal attributions of parenting, substance abuse, and low effort. The causal attribution of brain differences modestly countered the moralistic causal beliefs, but genetics was neutral.
Stress was modestly stigmatizing (correlated with social distance, parenting, substance abuse, and low effort), in contrast to some previous studies using attribution theory (
7,
10,
36 ). God's will did not show a correlation with social distance and had small correlations with low effort, genetics, and brain differences. There was some evidence that God's will tapped a fatalistic causal belief that combines biologically based difference with personal weakness.
The clearest effects—the moralistic causal attributions that were correlated with social distance and much more likely for depression and ADHD—were consistent with previous attribution theory research. However, the weaker effects—such as stress being modestly stigmatizing—point to the complexity of meaning in causal attributions. Although some children perceive stress as an external cause, raising genuine empathy for their peer, other children may blame a peer for not coping well with stressful life circumstances.
The participants reported diagnoses of depression at a slightly lower rate than prevalence estimates (
50 ) but reported ADHD diagnoses at rates markedly higher than prevalence estimates (
37,
51 ). The discrepancy of self-reported ADHD diagnosis and epidemiological estimates may reflect growing awareness of ADHD or that real-world diagnosis of ADHD is less rigorous than epidemiological diagnosis.
As a main effect, reporting a diagnosis was associated with the moralistic causal beliefs (parenting, substance abuse, and low effort). This likely reflects both children who are struggling to understand the meaning of having a diagnosis as well as internalized stigmatization. In the interaction model, most children with an ADHD diagnosis were less likely to endorse parenting, possibly because of the widespread neurological explanation for ADHD. Counter to the pattern of internalized stigmatization, those with a diagnosis of depression or ADHD were less likely to endorse low effort.
Cultural emphasis on family and religion was evident with Asian and Pacific Islander youths' and Hispanic youths' greater likelihood of endorsing parenting and African-American and Hispanic youths' greater likelihood of endorsing God's will (
52 ). There was modest evidence that Asian and Pacific Islander youths may have been more disposed toward genetic causal beliefs and that Hispanic youths may have been less disposed toward biological explanations. Further quantitative and qualitative research will provide a richer account of cultural variation and mental health stigmatization; however, these findings imply that antistigmatization efforts should be adapted to the racial and ethnic composition of the target group to synthesize the available evidence of how cultural worldviews shape beliefs about mental health problems.
The findings should be considered with several limitations in mind. The diagnosis of a target condition was based only on the child's recall of receiving a diagnosis. The study relied on self-report, and although the sample was drawn from and weighted to national population targets, it is not a probability sample. With Web-based research, participants from lower socioeconomic strata may be underrepresented because of lower rates of Internet access. Finally, although online surveys have been found to compare favorably to other survey methods (
44,
45,
53 ), these studies have been conducted almost exclusively with adults.
Conclusions
These analyses are based on data from the first large national study of children's stigmatization of other children with mental health problems. Earlier analysis of prevalence of social distance and negative attributes found marked stigmatization of depression and ADHD (
28 ). The moralistic and blaming causal beliefs found in this study provide further evidence of stigmatization and demonstrate how causal attributions are related to other stigmatization constructs such as social distance.
The findings suggest that causal beliefs are a promising target for stigma reduction programs, in combination with directly targeting other stigma constructs, such as social distancing or disproportionate associations of mental disorders with dangerousness (
8,
54 ). The modest to moderate effects of ethnicity indicate that culturally based beliefs about mental illness should be considered in planning antistigmatization programs. Professionals and family members should also be aware that children with ADHD or depression may be more likely to hold stigmatizing causal beliefs about their own conditions. This internalized stigmatization should be addressed in both prevention and treatment efforts.
Acknowledgments and disclosures
This research was supported by grant H133B990025 from the National Institute of Disability and Rehabilitation Research and by the U.S. Department of Education and the Center for Mental Health Services of the Substance Abuse and Mental Health Services Administration. The content does not necessarily represent the views or policies of the funding agencies. The authors give special thanks to Suzanne Martin and Harris Interactive.
The authors report no competing interests.