It has been well established that rural residents have poorer access to mental health services. Seventy-five percent of the areas with a mental health professional shortage are in rural areas (
1,
2,
3 ). Some rural communities lack access to any mental health provider (
4 ). Inpatient psychiatric units in general hospitals may be an important source of care for rural residents. These units could provide inpatient services and also support outpatient mental health services. Having an inpatient psychiatric unit may also attract mental health practitioners to these communities. Although these units have potential benefits, little is known about them and their impact on access to community-based mental health services.
Recent changes in Medicare reimbursement present a significant threat to the development and ongoing operation of inpatient psychiatric units in small rural hospitals (less than 50 beds). Before 2005 these units were paid based on reasonable costs. Beginning in January 2005 Medicare began transitioning from a reasonable-cost payment system to a per diem system, which became fully implemented in January 2008. Under this new system, psychiatric units within general hospitals receive the national average daily routine operating, ancillary, and capital costs, or federal per diem rate, adjusted by a number of factors. The Centers for Medicare and Medicaid Services (CMS) adjusts the rate for patient age, 15 related mental health diagnostic groups, 17 comorbid conditions, and electroconvulsive therapy treatments. They also adjust for location in a rural area and several other factors. CMS uses a variable per diem adjustment based on patient length of stay. The highest payment occurs on day 1, when a significant amount of diagnostic services are provided. The per diem rate decreases each subsequent day, reaching the base per diem rate for days 9 and 10. Payments fall below the base rate at day 11, and they continue to decline as the number of days increases. If a patient is readmitted to any psychiatric facility within 72 hours of discharge from another facility, the admission is considered continuous (
5 ).
This payment method may have a significant impact on the financial status of small rural hospital psychiatric units. First, many who commented on the rule felt that a 17% increase for units located in rural areas is too low and would result in a payment decrease for rural programs, compared with payments based on the reasonable-cost system (
6 ). Second, CMS estimates show that units with fewer than 12 beds would receive 1% less under the new system (
5 ) and would thus affect critical access hospitals, which are limited to only ten psychiatric beds. Critical access hospitals are specially licensed small hospitals that receive cost-based reimbursement for Medicare beneficiaries treated in nonpsychiatric units. To obtain this status, a hospital must be located in a rural area and have 25 beds or fewer, 24-hour emergency room coverage, and an annual average length of stay of 96 hours. Starting in 1999 critical access hospitals were allowed to have a psychiatric distinct part unit (DPU) with a maximum of ten beds. These units do not count toward the average length of stay calculation and do not receive cost-based reimbursement. Third, a recent study by RTI International found that dementia and cognitive impairment, severe psychiatric diagnoses, deficits in activities of daily living, and assaultive or agitated behavior were associated with high-intensity staff days (
7 ). Because some of these characteristics are not found in claims data, CMS opted to exclude them from payment adjustments (
5 ). In the most recent rule change, mild cognitive impairment was added as an adjustment, but only if this is the patient's primary diagnosis. Higher percentages of rural residents are elderly and in poor health, increasing the likelihood of rural psychiatric patients having these characteristics, especially in geriatric units.
This study sought to identify the typical characteristics of inpatient psychiatric units in small rural general hospitals, determine the availability of community-based services, and investigate the new payment system's early impact on closures of these units. We therefore conducted a survey of unit managers in small rural hospitals. For units that had closed in the past four years, we conducted a short semistructured interview with the hospital's director of nursing.
Methods
Our sampling frame included all rural and micropolitan hospitals with fewer than 50 beds that had an inpatient psychiatric unit in their general hospital at the time the survey was fielded in 2006. We identified these hospitals using three sources: the American Hospital Association's (AHA's) 2004 Annual Survey of Hospitals (
8 ), the Flex Monitoring Team's list of critical access hospitals with psychiatric DPUs as of June 2006 (
9 ), and the Substance Abuse and Mental Health Services Administration's (SAMHSA's) mental health services locator (
4 ). Using the AHA's annual survey, we identified all rural hospitals with fewer than 50 beds that stated that they offered inpatient psychiatric care. Next, we identified all critical access hospitals with a psychiatric DPU found in the Flex Monitoring Team's complete list of critical access hospitals. Finally, we searched for general hospitals with separate psychiatric units on SAMHSA's mental health services locator Web site. We used the AHA survey to identify whether each SAMHSA hospital had fewer than 50 beds, and we used Zip code-based Rural-Urban Commuting Area codes to determine whether each was rural. After removing all duplicate hospitals, we had a universe of 100 hospitals. Three of these were dropped when we found that they had never operated a psychiatric unit. We identified 11 hospitals that had closed their units within the past four years. These hospitals were all contacted for closed-unit interviews. We completed interviews with 74 of the remaining 86 hospitals, for a response rate of 86%. (Four of the hospitals operated two units, so the 74 respondents gave data on 78 units. However, respondents did not distinguish between the two units when responding to questions.)
The research team designed the survey instrument using current literature and a site visit at an inpatient unit in northern Maine. The survey was targeted to unit managers because they were expected to have the most knowledge about the unit and its daily activities. The instrument examined unit characteristics, staffing, and patients commonly treated in the unit. To identify commonly treated patients, we asked respondents about the types of symptoms or diagnoses and the types of patients or admissions they typically saw.
We asked several questions about clinical staff, including psychiatrists, Ph.D.-level psychologists, social workers, other counselors and therapists, nurse practitioners, and several types of unlicensed staff. For each provider type, interviewers asked whether the unit used any providers of that type, the number of these providers staffing the unit, and the total number of full-time equivalents (FTEs) or total number of hours worked per week. We also asked about staffing patterns for day, evening, and weekend shifts.
We asked three questions to evaluate access to community-based services. First, we asked respondents how frequently they had difficulty obtaining discharge care for their patients. Second, interviewers asked what services were available for postdischarge care. Third, we asked whether the units' psychiatrists, psychologists, social workers, other counselors, and nurse practitioners also offered noninpatient services in the local community.
Before fielding the survey, we successfully obtained institutional review board approval at the University of Southern Maine. Because the surveys and interviews were conducted by phone, we obtained verbal informed consent from the respondents. A pretest with four unit managers resulted in minor changes to the survey instrument. Surveys were conducted between October and December 2006.
For closed inpatient psychiatric units, we used a semistructured interview with questions about the unit before its closure, including the number of beds, average yearly admissions, the types of patients it treated, and whether it was a specialty unit or not. The second section of the interview included questions about when and why the unit closed, the impact of the closing on the community, and policies or resources that could have prevented the closing. Because of the small sample, the interview protocol was not pretested. A single research team member conducted all the closed-unit interviews with the director of nursing or the staff member with the most knowledge about the unit and its closure.
We calculated descriptive statistics using SAS, version 9.1.3. Frequencies were used for categorical variables, and medians were used for continuous variables. We used medians rather than means because median rates are more reliable when dealing with small samples. Because we contacted the universe of all rural inpatient psychiatric units, p values are not reported in our findings. For the qualitative data, we reviewed the information to identify common themes.
Results
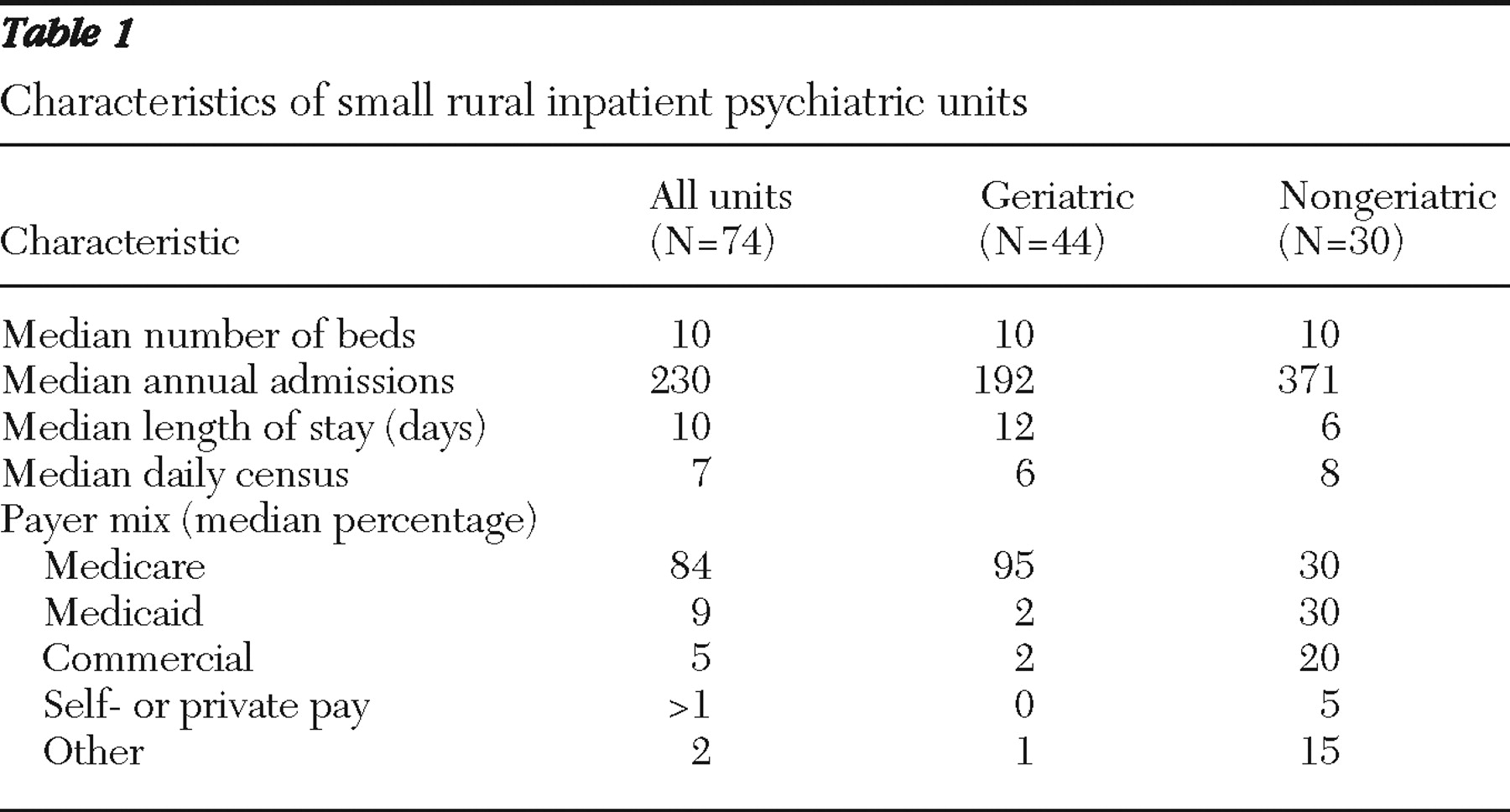
We were able to interview 74 unit managers: 44 from geriatric units and 30 from nongeriatric units. The typical small rural hospital psychiatric unit was a ten-bed geriatric unit with just over 200 admissions per year (
Table 1 ). The units had a median daily census of seven, with patients typically staying ten days, and were paid primarily through Medicare. Compared with nongeriatric units, geriatric units had fewer admissions per year, had longer lengths of stay, and relied more heavily on Medicare reimbursement.
All units reported having at least one registered nurse on staff, nearly all (N=73, 99%) had a social worker or psychiatrist, and most (N=51, 69%) had psychiatric technicians and licensed practical nurses on staff. Fewer units (30% or less) employed certified nursing assistants, other counselors or therapists, nurse practitioners, or Ph.D.-level psychologists. A typical unit had no more than one staff member from each category—psychiatrist, psychologist, social worker, counselor or therapist, and nurse practitioner—representing a total of four FTEs. Psychiatric technicians, registered nurses, licensed practical nurses, and certified nursing assistants were more abundant, with a median total of 23 providers on staff, representing about 18 FTEs. Geriatric units typically had more certified nursing assistants on staff (median=5.8), compared with nongeriatric units (median=5.0). In all the units, a psychiatrist, psychologist, social worker, counselor, or nurse practitioner was on staff only during the day. Also on staff in all the units were one or two of each of the following: psychiatric technicians, registered nurses, licensed practical nurses, and certified nursing assistants. The median number of staff at night was four, with approximately six people available on weekends during the day.
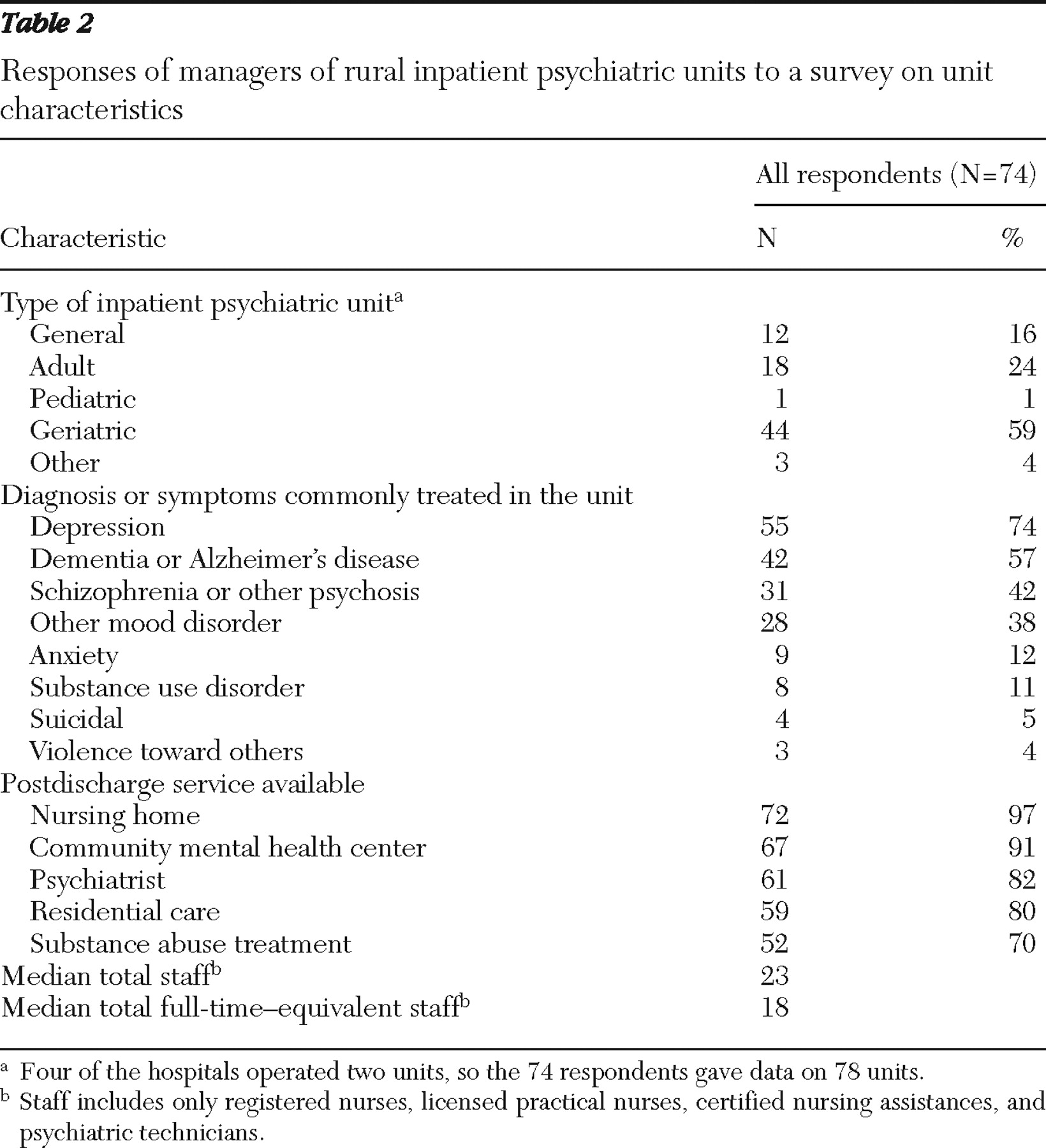
The three most common diagnoses treated were depression, dementia or Alzheimer's disease, and schizophrenia or other psychoses (
Table 2 ). Only 12% of units treated patients for anxiety disorders, and 4% treated patients who were violent toward others. It was common for units that treated patients with dementia or Alzheimer's disease to also treat depression and schizophrenia. Almost all units treated elderly persons (59%) or persons with dementia and Alzheimer's disease (57%). Sixty-four (87%) treated patients who had been involuntarily admitted, and 59 (80%) treated some patients with dual diagnoses.
Surprisingly, unit managers reported having difficulty obtaining discharge care for only 5% of their patients. At least two-thirds of the units surveyed had access to all the services listed in the survey (
Table 2 ). Sixty-three unit managers (85%) also reported that some providers working in their units also provided services in the local community. Providers who most commonly offered community-based services included psychiatrists, nurse practitioners, and psychologists.
We completed interviews with eight of the closed inpatient psychiatric units: four general units and four geriatric units. One of the units, a ten-bed geriatric unit, had been widely used before its closure, having an average daily census of nine and 96% of its patients coming from outside the hospital's service area.
We found that five of these eight units had closed, at least in part, because of changes in Medicare reimbursement. Before the reimbursement change, one hospital had been given a higher estimated payment rate. The unit was forced to close when CMS reduced reimbursement for inpatient psychiatric services. Another hospital found that reimbursement was just too low and closed its unit only eight months after opening it. The unit would have lost $1 million if it had remained open until the end of the year. Another unit treated patients with chronic mental health problems and significant medication management issues, making their lengths of stay longer. These longer stays resulted in financial losses under the new payment system.
Only two of the hospitals with closed units offered outpatient psychiatric services at the time of the survey. One hospital offered limited services 45 miles from the hospital. Since the units closed, patients have had to travel a minimum of 30 miles and a maximum of 160 miles for inpatient psychiatric care. Some hospitals felt that resources or policy changes could not have kept their units open. Others felt that they could have remained open with better Medicare reimbursement. This was especially true for geriatric units.
Discussion
This study examined the characteristics of inpatient psychiatric units in small rural hospitals, their access to community-based services, and the early impact of changes in Medicare reimbursement on these units.
Surprisingly, we found that unit managers had good access to community-based services. In a previous study, 43% of critical access hospital emergency departments reported having no local mental health providers (
10 ). In the study presented here, at least 70% of unit managers stated that they had access to a variety of postdischarge services. In addition, over 80% had clinical staff that provided services outside the inpatient setting. Although we cannot establish causality, our findings suggest that having an inpatient psychiatric unit may improve a community's access to mental health providers.
Medicare payment policy changes were a factor contributing to recent unit closures and may continue to affect these units in rural areas. Similar to previous findings (
6 ), our study showed that units that closed felt that a 17% increase in reimbursement in rural areas was too low, since the end result was a decrease in payments from those received in the reasonable cost system. We also found that many patients treated before closure had or were at higher risk of having characteristics associated with high-intensity staff days. However, CMS has excluded these patient-level adjustments because they are unavailable in administrative data (
6 ). We found a median length of stay of 12 days in geriatric units, compared with only six for nongeriatric units. Because reimbursement decreases to below the base rate starting on day 11, these geriatric units have a significant disadvantage. With consideration of the few rural inpatient units, a return to cost-based reimbursement, as is currently used for critical access hospitals, may be a simple remedy to prevent further closures.
This study had the following limitations. First, identifying units eligible for the study was difficult because the sample was selected through various sources. Because of this difficulty, we cannot be sure that we identified all units eligible to participate in our study. Second, for access to community-based services, we were unable to capture causality. Therefore, we cannot say whether having an inpatient unit attracts more community-based providers or having community-based services is a precondition for opening a unit. Third, the sample of closed units was small and inferences regarding the reasons for closure should be guarded.
Conclusions
Despite these limitations, our results provide important information about the typical inpatient psychiatric unit in a small rural hospital and its impact on the local community. Units in our study had better than expected access to community-based services. Future research is needed to compare rural communities with and without these units to determine the relationship between inpatient units and access to outpatient services.
The study also interviewed personnel at eight small rural hospitals that had closed their units. For five hospitals the closures were, at least in part, because of recent changes in Medicare reimbursement. The closures have resulted in poorer access to services. We should continue to monitor rural hospital inpatient psychiatric units for more closures and assess the financial impact of changes in Medicare reimbursement on units that continue to operate.
Acknowledgments and disclosures
This study was supported by grant CA U1CRH03716 from the Federal Office of Rural Health Policy, Health Resources and Services Administration. The authors thank Joanne M. Fortin, R.N., and Gabriella Cherascu, M.D., for their assistance in conducting the research.
The authors report no competing interests.